The Impact Of Stress On Ibd
Life always includes stresses which change over time. In adulthood, stress mainly originates from family, work, economic status, and major life-threatening events. Early life and childhood exposure to antibiotics, vaccination, diet, smoke, and psychosocial stress seems to lead to a long-term adverse influence throughout life. The stressors of the above different periods may increase adulthood susceptibility to diabetes, cardiovascular disease, autoimmune disease, stroke, and certain cancers .
Stress and the Risk of IBD Onset
A Manitoba IBD cohort study in Canada ascertained the first onset of psychotic symptoms via a structured diagnostic interview. The report showed that approximately two-thirds of patients who had both anxiety disorder and IBD actually developed psychiatric symptoms predating the IBD diagnosis by over 2 years. This more than 2-year time interval for diagnosis was also present in more than half of IBD patients with mood disorders. Moreover, IBD patients with lifelong anxiety or mood disorders displayed an earlier onset of IBD symptoms than those without the above disorders, and there was a tendency for an early diagnosis of IBD . These results reminded us of the potential interactions between IBD and psychiatric diseases. It is possible that the existence of these psychiatric illnesses may increase the susceptibility of individuals to IBD.
Effect of Stress on IBD Course
Effect of Stress on IBD Prognosis
You May Like: Does Stress Cause Low Blood Pressure
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
Medication For Inflammatory Bowel Disease In Adults
Gastroenterologists at NYU Langones Inflammatory Bowel Disease Center may prescribe one or more medications to reduce inflammation in the digestive tract caused by inflammatory bowel disease, or IBD. The goals of treatment are to improve symptoms and heal any damage to the intestines.
Our gastroenterologists develop a personalized treatment plan for you based on the type of IBD, the severity of the condition, and the results of diagnostic tests. These tests may have confirmed that you have Crohns disease, which can affect any part of the gastrointestinal tract, or ulcerative colitis, which only affects only the colon, or large intestine.
Medications work differently in different people, so your gastroenterologist closely monitors how well you respond to treatment. He or she adjusts the type or dose of medication as often as needed.
Medications for IBD can often reduce inflammation and promote healing in the intestines, resulting in remissionmeaning long-term symptom relief. However, for many people with IBD, the condition is chronic and treatment is lifelong. It is very important to follow up regularly with your gastroenterologist.
Dont Miss: Can You Get Acid Reflux From Stress
You May Like: Can You Drink Coffee With Ulcerative Colitis
Take Some Deep Breaths To Calm Your Gut
Breathing deeply can help reduce UC gut pain and cramping, says Sara Kinsinger, PhD, director of behavioral medicine for the digestive health program at Loyola University Health System in Maywood, Illinois.
Deep breathing elicits a parasympathetic relaxation response that physiologically helps the body relax by increasing blood flow and oxygen to the gut, she says.
Experiment with different deep breathing techniques, including diaphragmatic breathing and alternate nostril breathing, to learn what helps you relax.
Whole Grain Breads Cereals And Pastas
Whole grain flour is high in fiber because it hasnt had the germ or bran removed.
Its important to avoid eating food made from any whole grain flour, such as:
, including beans, lentils, and peas, are high fiber, high protein foods. Because of the indigestible sugars in beans, theyre also notorious for causing gas. If you are experiencing a UC flare-up, youll want to pass on the following:
- all beans, including chickpeas
- soy nuts, including soybeans and edamame
Also Check: Foods Not To Eat With Ulcerative Colitis
When Youre In The Hospital
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
Also Check: New Meds For Ulcerative Colitis
How Long Do Flares Last
Flares occur at different times and may last for days or weeks. They can happen anywhere from weeks to years apart, depending on the person and the effectiveness of treatment.
Your doctor will work with you to treat your flare and help return your UC to a more manageable state.
The Crohns & Colitis Foundation recommends waiting to become pregnant until UC has been in remission for at least 3 months.
If you conceive during a flare-up, you may have more symptoms during pregnancy.
Youre likely to have a healthy pregnancy if you have UC, but youll still have a higher chance of complications than someone without the condition. Particularly if your UC is active, you may have a greater risk for:
- miscarriage
In general, UC medications can be taken during pregnancy.
Talk with your doctor about any possible changes to your medications while pregnant.
Ideally, having a conversation with your doctor prior to getting pregnant can allow them to prepare a UC treatment plan in advance that can be revised, if and as needed, during your pregnancy.
Read Also: Is Omeprazole Good For Ulcers
Ulcerative Colitis Risk Factors
Anyone can develop ulcerative colitis. UC onsets are most common between ages 15-30 but can occur any time, and gender doesnt appear to be a factor in risk level . Despite UC lacking a target market, there are certain factors that make some lower intestines more at risk from UC than others.
- Smoking. Smoking = bad for you. You can add Ulcerative Colitis to the list of conditions it increases your risk of developing.
- Alcohol. Theres some evidence that prolonged/excess alcohol consumption might increase risk of IBDs. More research is needed into UC specifically, but if proved true would track with alcohols habit of being linked to health problems.
- Environmental Pollutants. Pollutants and toxins in the environment, such as air pollution or chemicals in some water supplies, increase UC risk. Research has shown this time and time again.
- Hereditary Risks. Probably the highest risk with UC is having close family members with UC. Genetics determine autoimmune response, gut bacteria, how we process alcohol and toxins basically everything else thats a UC risk/causal factor. If your family member has a UC-making DNA helix your chances of doing so too are, for obvious reasons, higher.
Dont Miss: Ulcerative Colitis Abdominal Pain Relief
Warning Signs Of A Flare
Flares often are acute, meaning they come on suddenly. They can last from days to weeks. Between flare-ups, you may experience weeks, months, or years of remission.
Symptoms of a flare may be different depending on the severity and location of the inflammation in the colon and rectum. Nevertheless, common symptoms include:
- Abdominal pain or cramps
Also Check: Pressure Ulcer Cream Over The Counter
What Are The Signs & Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are cramping belly pain and diarrhea. Other symptoms include:
- blood in the toilet, on toilet paper, or in the stool
- urgent need to poop
- low energy
- weight loss
Ulcerative coliits can cause other problems, such as rashes, eye problems, joint pain and arthritis, and liver disease. Kids with ulcerative colitis may not grow well as well as other kids their age and puberty may happen later than normal.
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Don’t Miss: How Do Doctors Treat Stomach Ulcers
Correlation Between Disease Activity And Endoscopic Findings
There was a consensus that endoscopic findings would usually affirm patients own assessment of their level of disease activity.
Testing has always been pretty much a confirmation of how Im feeling at the time.
The colonoscopy reports and photos are basically, well, heres what this looks like and this looks like and heres the issue. So, theyre pretty in synch.
Reduce Stress To Combat Uc Flare
While stress doesnât cause ulcerative colitis, it can trigger flare-ups and make your symptoms worse. Try the following for lowering your stress levels:
- Exercise. Youâve probably heard it a lot, but itâs true â even mild exercise is important for combating stress and inflammatory disease. It can also give you a boost in fighting depression, and it can help keep you more regular.
- Biofeedback. This is a technique that uses a device to help you reduce tension in your muscles and slow your heart rate. There are lots of types of biofeedback machines out there. They give you information about how your body is functioning by measuring different things using sensors. These include brain waves, your breathing or heart rate, muscle contractions, sweat glands, and temperature. Talk with your doctor about what device might be best for you.
- Relaxation and breathing exercises. This could include trying things like yoga and meditation. There are many options depending on your needs, from in-person classes to videos online.
- Get enough sleep. This can help you better cope with stress and prevent flare-ups.
- Talk to a mental health pro. A therapist, counselor, or psychiatrist can help you navigate all of these strategies. They can also help you talk through the negative and sometimes embarrassing effects that UC can have on your life.
Also Check: What Is A Venous Stasis Ulcer
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Manage Symptoms Of A Flare
While you work with your doctor to get your flare under control, you can take steps to ease certain symptoms:
Pain. Experts say acetaminophen is the safest way to get pain relief. If it doesnt help you enough when you have pain in your stomach or another body part, ask your doctor what other meds theyd recommend.
Sometimes UC is linked to pain beyond your gut. If you get eye pain or if your eyes feel sensitive to light, see a doctor called an ophthalmologist as soon as possible. Some people living with UC develop eye problems that need fast treatment.
If you have leg pain or pain in another large joint, it might be due to arthritis linked to your UC. Your doctor may tell you to rest the joint that hurts. They may also recommend that you occasionally soothe it with moist heat, like from a warm bath or heated wash cloth. You could also ask the doctor if physical therapy might help.
Irritated bottom. Keep it clean with moist wipes and protect it with diaper cream. You could also soak in a saltwater bath.
Diarrhea. Ask your doctor if you can take an anti-diarrheal drug, like bismuth subsalicylate or loperamide .
Canker sores. Medicated mouthwash may ease the irritation that these small mouth ulcers bring on. A balanced diet and a multivitamin or mineral supplement may help, too. Talk to your doctor before you try any new supplement.
Recommended Reading: Calcium Alginate For Pressure Ulcers
Food As Trigger Of Flare
Participants frequently discussed the possibility that certain foods could trigger flares, but had great difficulty in identifying common themes across participants.
I never could figure out what triggers it. When Ive got a flareup going, I mean, its always, I eat, and then half an hour later Im in the bathroom.
I know until I kept a food journal, I had no concept of what would or wouldnt trigger it. I just its hard to isolate.
Read Also: How To Cope With Anxiety Stress And Depression
Ulcerative Colitis Questions To Ask Your Doctor
Whether youâre worried your symptoms are UC, or you already have the condition and want more information, here are questions to ask your doctor:
- Are my symptoms a sign of ulcerative colitis or another condition?
- Are there different kinds of UC? Do they have different symptoms?
- What tests will I need?
- If I have ulcerative colitis, what will my treatment plan be?
- Will changing my diet or lifestyle help ease my symptoms?
- How serious is my ulcerative colitis?
- If I take medication for ulcerative colitis, will there be side effects?
- Should I take nutritional supplements like probiotics?
- How often will I need to come in for checkups?
- What should I do if my symptoms suddenly get worse?
- How do I know if my ulcerative colitis is getting worse?
- How do I know if I should change my ulcerative colitis medication?
- Should I consider surgery? What does surgery involve?
- What is my risk of getting colon cancer?
Recommended Reading: What Should You Not Eat If You Have An Ulcer
Get Regular Exercise To Reduce Uc Inflammation
Snider says exercise is useful in managing many of the complications associated with ulcerative colitis, including decreased bone density, a weakened immune system, emotional health problems, stress, and weight gain.
Try to engage in a moderate-intensity exercise like swimming or biking, three or four days per week, he says. A review published in August 2016 in Pharmacological Reports noted that moderate exercise releases protective myokines such as irisin from working skeletal muscles, which promotes healing and helps with inflammatory bowel disease inflammation.
Snider also strongly recommends yoga as a natural treatment for ulcerative colitis, as it promotes relaxation and targets the digestive system, flooding the area with oxygen and nutrition for healing. Find what type and frequency of exercise works for you and take it slow: Too much exercise can cause mild systemic inflammation.
Research indicates that stress plays a role in inflammatory bowel diseases such as ulcerative colitis. Researchers analyzed data on 2,007 adults in a Swiss IBD study and found a relationship between depression and anxiety and disease symptoms. The results were published in June 2016 in Clinical Gastroenterology and Hepatology.
Counteract stress with relaxation techniques such as meditation, deep breathing, and progressive muscle relaxation to help your body relax.
How To Ease Flare
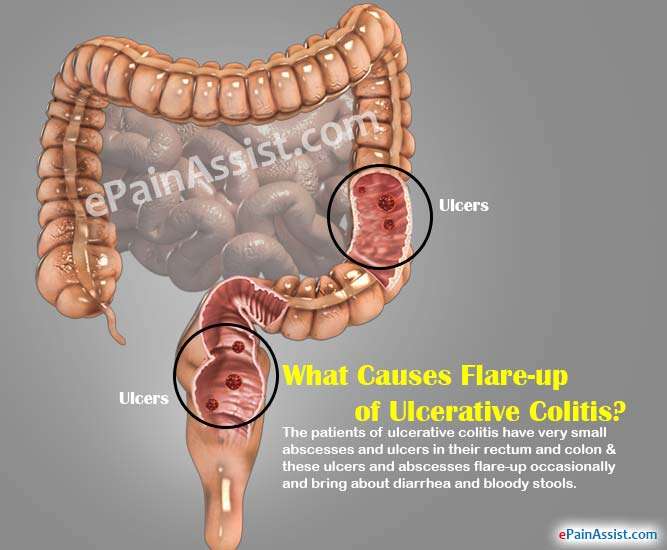
One of the major problems of suffering with ulcerative colitis is the sudden flare-ups which are caused by the triggers of ulcerative colitis. These flare-ups will cause diarrhea and bloody stools and can lead to complications. These flare-ups would possibly occur, no matter staying on your treatment. So it is crucial to understand the way to manage and ease the flare-ups in ulcerative colitis.
Getting treatment as long as you begin experiencing the symptoms is the major step in managing ulcerative colitis. However, this could be tough and you must so acknowledge what is traditional and is not traditional. The target of remission is to make sure you are feeling well for long durations. Therefore, you must not anticipate your symptoms to be worse so as to hunt medication. Besides, you must pay additional attention once exposed to triggers of the condition, like foods and stress that provoke your symptoms.
Getting treated by your doctor is that the best approach of easing the symptoms of ulcerative colitis. However, the below mentioned tips can help you in a long way in easing flare-ups caused by ulcerative colitis:
Read Also: What Is A Perforated Ulcer
Make Time For Activities That Make You Happy
Tip number three to help you prevent an ulcerative colitis flare-up: Always make time for things that make you happy. For me, its dancing. I have been taking dance classes since my pre-school years and continues to do so to this day. Its wonderful exercise, I have met amazing friends through this hobby, and it is also my favourite form of exercise. When I am in the dance studio, I forget about everything else in the world and focus on being in the present. So, whether it be dance, a sport that you love, or something as beautiful as painting, make time to feed your hobbies with your time and hopefully you will feel more fulfilled and less stressed!
Also Check: What Is The Definition Of Post Traumatic Stress Disorder