Ask If There Are Disability Services
Not all resorts or destinations, especially those outside of the United States, offer disability services for visitors, but some do. Disney, for example, offers visitors a Disability Access Service while visiting their parks.
Kosciuk recently took advantage of this DAS program while on vacation with her family at Disney World. It allows people who have some sort of reason that they cant stand in line for long periods of time to avoid standing in line, she says. I used it for one day of my Disney vacation after I ate something that disagreed with me. It allowed me to participate fully in my vacation with my children.
Ulcerative Colitis: Let’s Talk
Colitis, Ulcerative Colitis, and Crohn’s are often used interchangeably – but in reality, they explain three different conditions. Colitis is the general inflammation of large intestine lining . It is synonymous with Irritable Bowel Disease and encompasses multiple conditions. Ulcerative Colitis: is a specific digestive issue, identified by ulcers on your large intestine.
How Can I Track Foods That Cause Flare
The Crohns and Colitis Foundation of America recommends people with ulcerative colitis keep a food journal to keep track of what they eat. Note what you eat and drink, and how you feel afterward, noting any symptoms that arise. Start to keep a list of any foods you suspect may trigger or aggravate your ulcerative colitis symptoms. A food diary will also help you figure out if you are getting adequate nutrition, and can help your doctor or dietician determine the right diet for you to manage your symptoms and prevent flares.
The Crohns and Colitis Foundation of America also has an interactive food tracking tool. It is available online or as a mobile app. www.ccfa.org/gibuddy
Dont Miss: Pressure Relieving Mattress For Pressure Ulcers
Read Also: Simponi Dose For Ulcerative Colitis
Nutrition Tips For Inflammatory Bowel Disease
Inflammatory Bowel Disease is a term used for two specific and separate diseases: Crohn’s disease and ulcerative colitis. Nutritional recommendations are different for each disease and for each individual patient. It is important to discuss the treatments that are right for you with a registered dietitian and with your doctor.
Is Ulcerative Colitis A Genetic Condition

One of the most significant risk factors for Ulcerative Colitis is family history. Scientists believe that individuals inherit genes that put them at risk for Ulcerative Colitis. At some point in life, environmental factors trigger the immune systems to attack the large intestine and the disease sets in.
Researchers estimate that between 10 and 25 percent of people with Ulcerative Colitis have an immediate family member with IDB. It is also believed that if one parent of a child has IBD, the child has a two percent risk of also developing IBD at some point in life. If both parents have IBD the risk for the child increases. Ulcerative Colitis is also more prominent in individuals who have more distant relatives that suffer from Ulcerative Colitis. Research also indicates that in individuals with a family history of Ulcerative Colitis, the age of disease onset tends to be earlier.
More specifically, studies have been conducted on both identical and fraternal twins who have Ulcerative Colitis. If one twin has Ulcerative Colitis, their identical twin will also have Ulcerative Colitis about sixteen percent of the time, while their fraternal twin will have Ulcerative Colitis about four percent of the time.
Despite all these statistics, it is important to note that most individuals with Ulcerative Colitis do not have a family history of IBD.
Read our full discussion of Ulcerative Colitis and Genetics here.
You May Like: Is Stelara Approved For Ulcerative Colitis
It Can Affect You Mentally Too
Beyond the physical symptoms, UC might also impact your mental health.
Fighting a war with your own body can take a mental toll.
- Around 35% of people with UC or Crohn’s disease experience symptoms of anxiety.
Note: A UC flare on its own typically doesn’t lead to a new mental health condition like depression or anxiety, says Dr. Max Pitman, gastroenterologist at Salvo Health. But UC might worsen your existing anxiety or mood-based issues through the gut-brain connection.
When I’m flaring up, it’s like being stuck in a dark fog. I feel hopeless, anxious, and even guilty often because I feel too exhausted to stick to work deadlines and have to cancel plans.
But, I had to learn how to give myself a break. I’m not lazy: I’m just tired. I have a chronic illness that impacts my gut. And my gut may affect my brain, in turn: One review found that people with IBD have higher rates of anxiety when the disease is active versus in remission, suggesting an upset gut may play a part in mental distress.
If you’re having trouble managing your mental health, treatments like cognitive behavioral therapy could help.
Pitman recommends a form of CBT called gut-directed cognitive behavioral therapy, which helps you learn coping methods for your thoughts and emotions when you have a GI illness. Some research even suggests that gut-based CBT might improve digestive tract symptoms.
What Should I Eat During A Flare
Youre feeling good, taking your medication, eating generally anti-inflammatory foods, and all of suddenbamyou start to feel those telltale flare symptoms. What should you do now? Adjusting your diet may help you over the hump.
If you are in a flare, you may want to eat foods that are gentle on your digestive tract, while the inflammation calms down, says Dr. Singh.
Practically speaking, you can do this in a few ways. For instance, Freuman works with her clients to tailor a well-rounded diet to avoid their specific triggers and address their needs. This may include:
Its best to work with a professional when making changes to your diet, as they can ensure that you are getting the nutrients that you need, help you assess your trigger foods, and address any underlying history of disordered eating or dietary changes that could trigger those behaviors.
Read Also: Patient Education On Pressure Ulcer Prevention
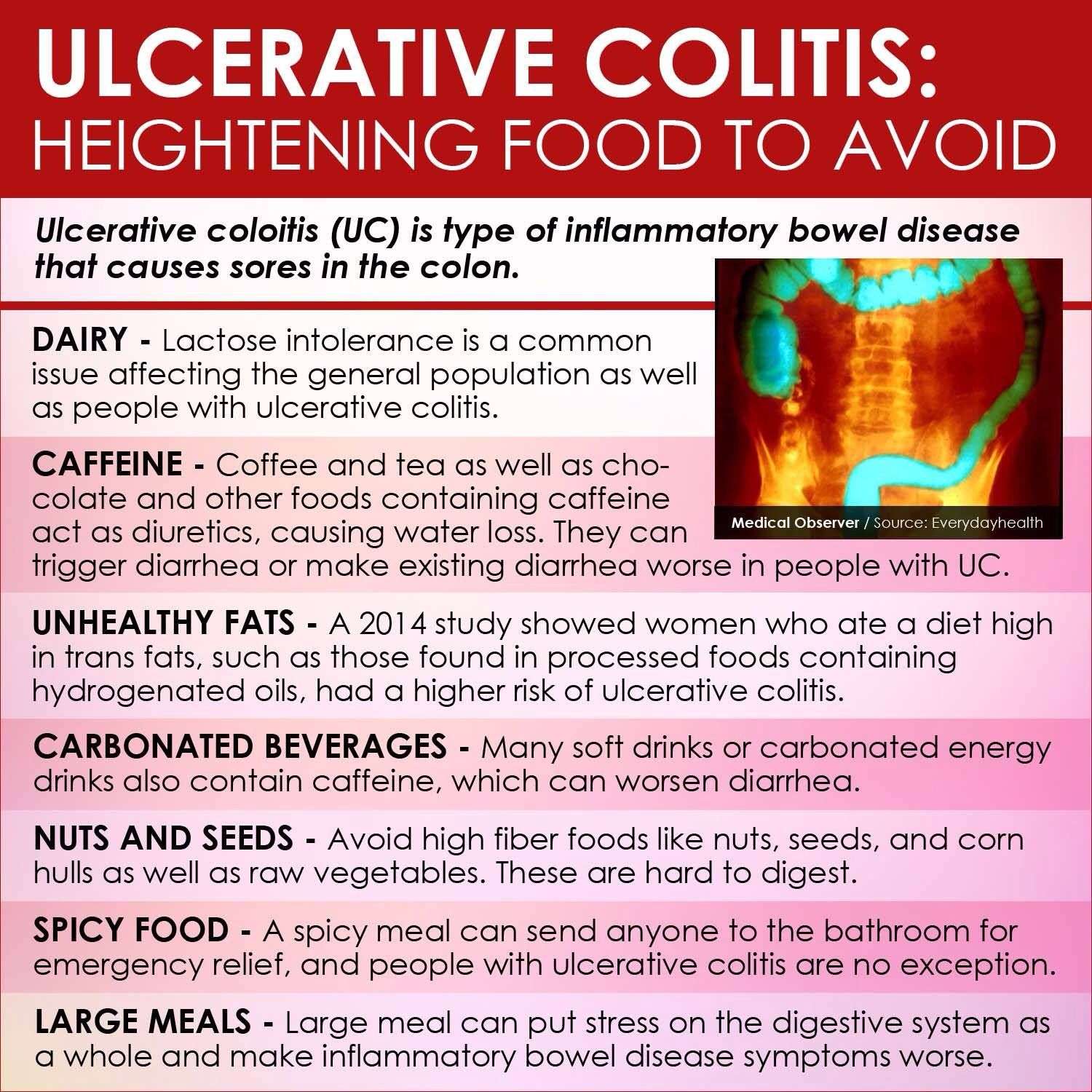
Foods To Avoid With Ulcerative Colitis
Although there are foods that are common triggers during both Ulcerative Colitis flares and remission, the list expands when youre experiencing active Ulcerative Colitis symptoms. Keep in mind that Ulcerative Colitis triggers differ from person to person, so the real key to long-term Ulcerative Colitis management is identifying what works for you. Easier said than done, right?
If youve ever searched on your own to figure out how to manage your Ulcerative Colitis, youve probably found a ton of information. The challenge is that the information on the internet can be contradicting and confusing. If youre struggling with Ulcerative Colitis, we recommend enlisting the help of a registered dietitian. They will be able to help you better understand your UC and determine what foods and behaviors most trigger your symptoms.
Remember to limit fiber when you are experiencing an Ulcerative Colitis flare. High fiber foods are part of a healthy, well-rounded diet. However, when UC symptoms are active, you may need to temporarily limit fiber intake to reduce inflammation and allow your gut to heal. High fiber foods are harder to digest and can trigger UC symptoms. High fiber foods include whole grains, fruits with skin and seeds, vegetables with skin and seeds, raw vegetables, cruciferous vegetables, nuts, seeds, beans and legumes.
It Can Be Challenging To Differentiate Between Crohn’s And Ulcerative Colitis
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
|
|
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
Also Check: Hyaluronic Acid For Ulcers In Horses
Understanding Ulcerative Colitis Flare
A flare-up is the reappearance of disease symptoms. And for people living with ulcerative colitis , an inflammatory bowel disease , flare-ups can be unpredictable, lasting hours, days, or weeks.
- Frequent and/or urgent bowel movements
- Lack of appetite
- Joint and body aches
Because these symptoms may also be caused by something other than UC, it can sometimes be difficult to tell whether youre experiencing a flare-up. Below, we look at factors that might affect a UC flare-up, and what can help if you are experiencing a UC flare-up.
Uc And Lactose Intolerance
People with UC often think they have lactose intolerance, which means they cant properly digest the sugar in milk and milk products, because some symptoms are similar. But UC doesnât make you more likely to have lactose intolerance. Your doctor can do a simple test to find out.
If you can, keep milk and dairy products in your diet. They are a very good source of calcium and vitamin D, which keep your bones healthy. Using steroids such as prednisone for a long time can thin your bones and make it harder for your body to absorb calcium, raising your chance of having osteoporosis.
If dairy products cause you discomfort, see if you can eat them in small amounts. Or try a lactase supplement to break down the lactose in dairy products.
If you just cant stomach dairy products, your doctor may want you to take calcium and vitamin D supplements. Watch a video on how dairy affects ulcerative colitis.
You May Like: Can Tylenol Cause Stomach Ulcers
Read Also: Venous Leg Ulcer Pain Relief
Ulcerative Colitis Diet: What To Eat To Manage Symptoms
A tailored diet for ulcerative colitis may provide you with some relief
Ulcerative colitis is a type of inflammatory bowel disease in which the immune system is thought to attack the gut lining, failing to recognise it as part of the body. A focused ulcerative colitis diet may therefore help with the management of symptoms. With the guidance of an IBD team or a dietician, those suffering from ulcerative colitis can be put on an elimination diet in order to identify potential trigger foods, or may be encouraged to keep a food diary in order to track links between certain foods and symptoms.
Those who have undergone surgery or are struggling with an ulcerative colitis flare up may be put on a low residue diet or a low fiber diet in order to manage symptoms and lessen the burden of their disease.
However, ulcerative colitis diets are often unique to the individual, so some experimentation under medical supervision may be necessary to find the right eating pattern for you. An ulcerative colitis diet may not work at all either, so it is important to collaborate with your medical team in order to properly manage your condition.
Inflammatory Bowel Disease Management
Inflammatory bowel disease is not caused, nor can it be cured, by what you eat. Doctors and dietitians agree, however, that food may play some role in the underlying inflammatory process that causes IBD symptoms.
Certain foods may aggravate symptoms, while others may calm them and promote healing. Therefore, paying attention to what you eat and how your body responds to different foods is an important component of a total treatment plan for IBD.
A diet plan can supplement but should never replace medical treatment for IBD. Always take your medications exactly as prescribed by your doctor.
Read Also: How Can You Get Rid Of Ulcers
Ulcerative Colitis Diet: What To Avoid In A Flare Up
A study in the journal of Advances in Nutrition found that a high fat diet can increase intestinal permeability, something that is already a problem for those with ulcerative colitis. A review in the Mediators of Inflammation journal indicates that the upset caused to the gut wall by ulcerative colitis may also increase intestinal permeability and as such, reducing foods that also impact intestinal permeability, particularly during a flare up, is advisable.
A spokesperson from Crohns & Colitis UK explains that there is no one-size-fits-all approach to eating while in a flare up.
No particular diet has been proven to help people with ulcerative colitis, they say. Some people find that certain foods trigger symptoms or flare-ups but others do not. Everyone is different and what works for one person may not work for another. Theres no single diet that works for everyone. While changing your diet can help you manage your symptoms, it does not replace medical treatment. Its important not to make any changes to your diet without speaking to your IBD team or dietitian first.
Tips For Managing Ulcerative Colitis Symptoms
- Consult your healthcare provider or dietitian before making any changes to your diet
- Eat a well-balanced nutrient rich diet
- Eat more frequently. Eat five to six smaller meals over the course of a day
- Stay hydrated by drinking water and fluids with salt like broth, tomato juice or rehydration solutions
- Drink slowly and avoid using a straw because these may cause gas due to taking in air
- Use a food diary to record the foods you eat and how these impact your symptoms
- Avoid your specific trigger foods
- Use simple cooking methods boil, steam, grill, poach, broil or saute
Don’t Miss: How Would You Know If You Have Ulcer
Food Swaps For A Healthy Ulcerative Colitis Diet
Follow these tips to reduce flares while enjoying the foods you love.
The effect that food can have on a persons ulcerative colitis flares can be unpredictable. Tomatoes or onions, for example, may irritate one persons digestive system, but they may not trigger the same symptoms in someone else.
Still, even though there is no specific ulcerative colitis diet, there are some foods, generally speaking, that can worsen a flare and should be avoided.
When we think of ulcerative colitis, we have to ask, Is this person in a flare meaning, is there inflammation in the GI tract? Eating insoluble fiber like nuts, seeds, peels of fruits, and raw veggies only further irritates an ulcerated, inflamed colon, says Stacy Cavagnaro, a registered dietitian for the Inflammatory Bowel Disease Medical Home at Cleveland Clinic.
If you have UC, you may feel helpless against the flare-ups, wondering if youll ever be able to enjoy normal food again. But dietary and lifestyle modifications may help control your symptoms and extend the time between flares. Here are seven food swaps to help minimize symptoms and keep you in remission.
Cooked And Peeled Vegetables
Many vegetables are high in fiber, but as with fruit, peeling them removes a layer of insoluble fiber.
Some vegetables do not need peeling, such as asparagus tips and mushrooms, but it can help to remove the skins of potatoes, carrots, and squash.
Cooking vegetables also makes them easier to digest, and it can reduce the fiber contents.
However, avoid roasting or frying vegetables in oil or butter, because fats can irritate the digestive system and worsen symptoms of Crohns. Try boiling or steaming them instead.
Read Also: Best Ulcerative Colitis Diet Book
Recommended Reading: Can You Drink Coffee With Ulcerative Colitis
Ulcerative Colitis Treatment Medications
Treatments for ulcerative colitis includes both medications and surgery however, there is no medication that can cure ulcerative colitis. Medicationsthat treat ulcerative colitis are
- anti-inflammatory agents, for example, 5-ASA compounds like sulfasalazine , and olsalazine , and topical and systemic corticosteroids), and
- immunomodulators, for example, 6-mercaptopurine , azathioprine , methotrexate , cyclosporine .
Treatment of ulcerative colitis with medications is similar, though not always identical, to treatment of Crohns disease.
Also Check: Pepto Bismol And Ulcerative Colitis
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohns Disease and ulcerative colitis.
Liquid Supplements for Crohns Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
Recommended Reading: L Glutamine Ulcerative Colitis Dosage
You May Like: Diet For Someone With Stomach Ulcers
Ulcerative Colitis In Children
Without proper care, pediatric ulcerative colitis will result in slower than normal growth and/or stunted growth.Intestinal inflammation lowers a childs appetite, which mean less food is eaten resulting in fewer nutrients to support healthy growth. Supplements are often a good idea as is making sure that enough calories are consumed, which sometimes requires a high-calorie diet for some kids. Additionally, a therapy or counseling may be sought to help a child develop the tools to cope with their disease.
Recommended Reading: Wound Care Treatment For Diabetic Foot Ulcer