Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Getting Referred To A Gastroenterology Team
If your blood and stool tests show inflammation, you should be referred by your GP to a defined specialist gastroenterology doctor in an IBD service. They have expert knowledge of gut conditions like Crohns and Colitis, and can do specialist tests like endoscopies . In some areas, you may be able to have some choice over which hospital you go to if you have been referred through the NHS e-Referral Service.
It may take some time to get an appointment with your gastroenterology team. The IBD Standards state that you should have a specialist assessment within four weeks of being referred, but it may sometimes take longer. Your GP should let you know how long you can expect to wait contact your GP surgery if you havent heard from the hospital within that timeframe so that they can chase up for you. You can also talk to your GP about how best to manage your symptoms while you wait for an appointment, and what to do if you start to feel worse.
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
You May Like: How Do You Determine If You Have An Ulcer
How Do You Get An Ulcerative Colitis Diagnosis
One important thing to note is that people with more severe cases of ulcerative colitis are at an increased risk of developing colon cancer and other serious health conditions, like liver disease, Rudolph Bedford, M.D., a gastroenterologist at Providence Saint Johnâs Health Center in Santa Monica, California, tells SELF. Thats why its important to reach out to a medical professional if you do have any of the above symptoms.
However, an ulcerative colitis diagnosis can be challenging because other conditions can mimic symptoms of IBD, like infections or even hemorrhoids, Dr. Sinha says. In terms of differentiating between Crohns and ulcerative colitis, he says, Theres no single test that we have that 100% distinguishes between the two. We rely on the patient history and other information such as radiographic imaging and endoscopy. Doing a colonoscopy, for example, can be one of the most reliable ways to identify IBD and to then distinguish between Crohns and ulcerative colitis.
While a colonoscopy is an effective tool, Dr. Sinha clarifies that its not the only way. Rather, theres an entire constellation of tests and data that can be considered, including imaging, lab tests, and a detailed intake of the patients symptoms and presentation.
When To See A Doctor If You Have Bowel Concerns
If youre having bloody diarrhea, dont wait to get help. Talk to a health professional sooner rather than later, so you can start working on a treatment plan that will get you out of the bathroom and back to normal.
Dr. Philpott also recommends keeping track of your symptoms. It can be hard to assess your response to treatment if you dont know where you started, Dr. Philpott notes. Document your symptoms down to the number of bowel movements you have. Life can be so hard with this condition that people sometimes have a hard time communicating. If you keep track of the symptoms objectively, its easier for your doctor to see how youre doing.
You dont have to just live with uncomfortable symptoms, even if youre already taking medications, Dr. East says, as adjustments to your treatment plan may be necessary. Long-term poorly controlled inflammation increases your bowel cancer risk and decreases your quality of life. New treatments could ease you into remission faster and keep you there longer.
Recommended Reading: Blood Clots In Stool With Ulcerative Colitis
Why Choose Mount Sinai
Mount Sinai has a unique and rich tradition of specialized and individualized treatment and scientific research and discovery in ulcerative colitis. The physicians/scientists in the Mount Sinai Health System are constantly conducting clinical trials and are developing new drug therapies to help patients manage their disease. Learn more about ulcerative colitis.
There are 3 basic tests for colon cancer a stool test , sigmoidoscopy , and colonoscopy . All 3 are effective in catching cancers in the early stages, when treatment is most beneficial.
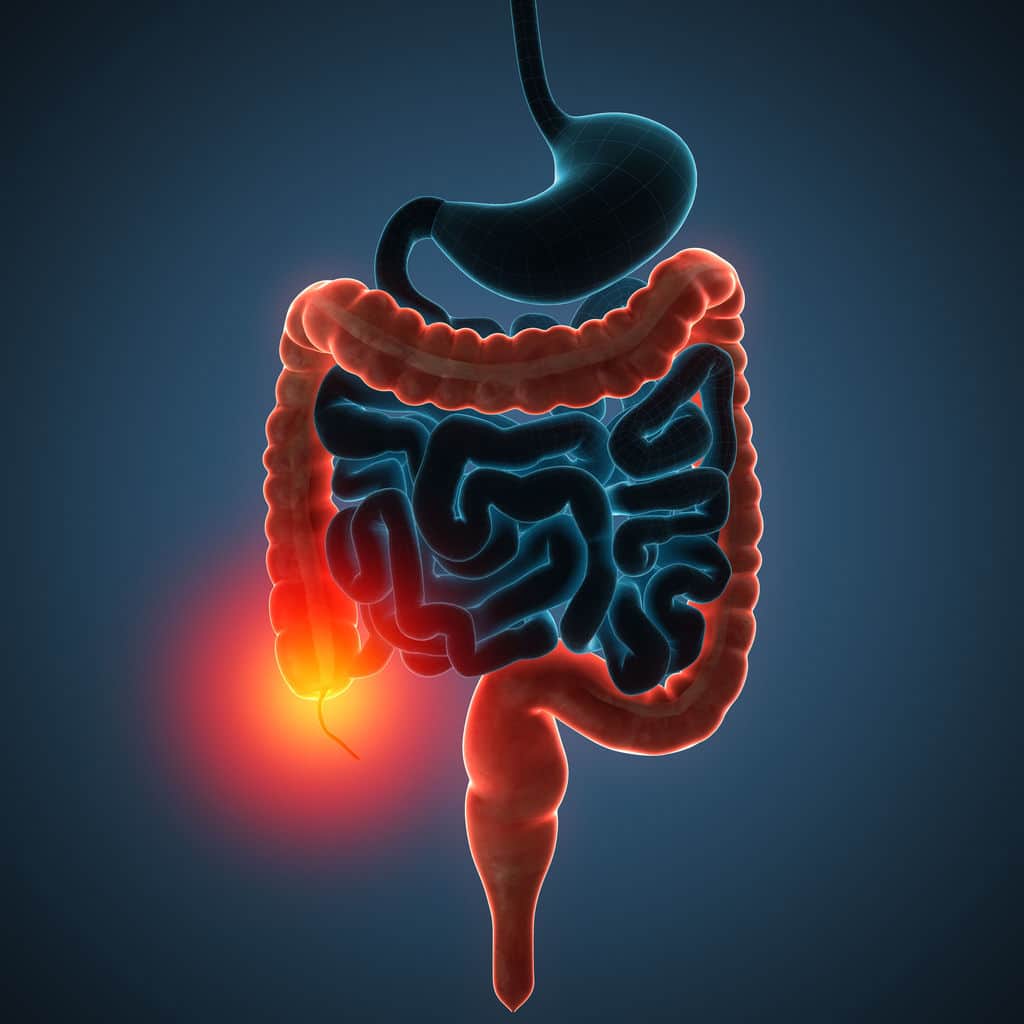
The esophagus, stomach, large and small intestine, aided by the liver, gallbladder and pancreas convert the nutritive components of food into energy and break down the non-nutritive components into waste to be excreted.
Ulcerative colitis is categorized according to location. Proctitis involves only the rectum. Proctosigmoiditis affects the rectum and sigmoid colon. Left-sided colitis encompasses the entire left side of the large intestine. Pancolitis inflames the entire colon.
Most Symptoms Of Ulcerative Colitis Relate To Bowel Movements
The symptoms of ulcerative colitis can vary from person to person, based on where the disease is in the body and how bad the inflammation is.
Most common symptoms:
- Diarrhea , which is often the first symptom.
- Blood in the stool.
- Urgency, or immediate need, to go to the bathroom.
- Increased number of bowel movements.
- Belly pain and cramping.
Ulcerative colitis can cause symptoms throughout your body.
You might have weight loss or other symptoms that affect the entire body. The inflammation of ulcerative colitis can also affect your joints or skin, leading to painful joints and skin rashes. During a flare-up, symptoms may go beyond those that affect the digestive system, including:
- Rashes or patches of red, swollen skin.
- Painful or swollen joints.
- Red, irritated eyes.
Keep of track of any symptoms, how often you have them, and how bad they are to talk about with your health care provider.
Read Also: Prevention Of Diabetic Foot Ulcer
What Can I Expect From The Test Results
Your doctor will typically talk with you about your results after the procedure, and they will be either negative or positive. Negative results mean nothing abnormal was found during the test. Positive results mean that polyps or other abnormal tissue was found during the exam. If youve only had a sigmoidoscopy, your doctor may want to schedule a colonoscopy to see the rest of your colon, per the Mayo Clinic. If your colonoscopy results were positive, your doctor will talk with you about a treatment plan moving forward.
What To Know About Ulcerative Colitis Triggers And Flare
Once you have an ulcerative colitis diagnosis, its important to know that triggers and symptoms vary from one person to the next. A big part of your UC journey will be figuring out exactly what causes symptoms to flare up for you. Stress, loss of sleep, and the foods you eat can all play a role in triggering a flare, according to the Crohns and Colitis Foundation. Once a flare subsides, you could find yourself in a remission that lasts weeks, months, or years.
During flares, it could feel like déjà vu with a return to symptoms you noticed at the start of your journey, including:
- frequent trips to the bathroomsometimes a dozen or more a day
- bloody diarrhea
- fatigue, exhaustion, or physical weakness
- loss of appetite or weight loss
Flares can occur without a trigger, James East, M.D., colonoscopist and gastroenterology consultant at Mayo Clinic in London, tells SELF, although stress, infection, and running out of medication can all start a flare.
He recommends an at-home stool test to help you pinpoint when a flare is starting. This can help patients self-monitor their disease at home and pick up flares early so treatment can be initiated promptly.
Recommended Reading: Can Tylenol Cause Stomach Ulcers
While There Is No Cure For Ulcerative Colitis There Are Many Options To Help Treat It
The goals of treatment are to:
- Control inflammation, or swelling.
- Ease symptoms, like pain, diarrhea and bleeding.
- Fix nutrition deficiencies, if needed.
Treatment will depend on the severity of the disease, past complications and response to earlier treatments. Remember, everyone experiences symptoms of ulcerative colitis differently. If one treatment doesnt work as well, there are other options. Just be sure to be in touch with your gastroenterologist often.
Treatment options for ulcerative colitis involve medications, surgery or a combination.
Medications
The goals of using medications are to start or keep up remission and to improve quality of life. Each person reacts a little bit differently to each drug and many need a combination of drugs. While some of them have side effects, the benefits and symptom relief often outweigh those drawbacks. Learn more about each class of drug in theLiving with IBDpages.
Biosimilars have been approved by the U.S. Food and Drug Administration to use as treatment in place of existing biologic drugs.
They are based on an existing biologic but are not an exact copy.
Biosimilars work the same way as their originator biologics and are given the same way.Read more about biologics and biosimilars.
Your doctor can prescribe a biosimilar as a substitute for a biologic drug however, your pharmacist cannot change you from a biologic drug to a biosimilar without your doctors approval.
Other medications
Causes Of Ulcerative Colitis Flares
Ulcerative colitis flares can be caused by a variety of things, including:
- Skipping medications or not taking the correct dose. If you regularly take medicine for your ulcerative colitis, you need to be consistent even when your disease is in remission. If you dont follow prescription instructions, flares can occur.
- Taking non-steroidal anti-inflammatory drugs. Common drugs like aspirin, naproxen, and ibuprofen can inflame the bowel and bring on serious symptoms. If you need mild pain relief or fever treatment, you should take acetaminophen.
- Taking antibiotics. Although theyre useful when you have bacterial infections, they affect the bacteria that live in your intestine. These changes can result in diarrhea or the growth of too much of a certain bacteria that then causes inflammation. If you have a bacterial infection, make sure your healthcare provider knows you have ulcerative colitis.
- Not managing stress. Physical and emotional stress can bring on flare-ups. Once you understand that stress causes such a reaction, you can find out what stress management strategies work to keep flare-ups at bay.
- Eating and drinking triggering items. The foods and drinks that bring on symptoms vary by person. Youll need to track your diet so you can pinpoint triggering items when you experience ulcerative colitis flares.
You May Like: How To Get Rid Of Ulcers In Horses
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Living With Uc: Diet Changes
Although it has not been found that diet has an effect on ulcerative colitis, it generally is recommended that patients eliminate any foods that they find are making their symptoms worse. For example, milk in people with UC who are intolerant to the sugar in milk, lactose, may be causing gastrointestinal symptoms such as abdominal bloating, flatulence, and diarrhea, symptoms that may overlap with those of ulcerative colitis. Despite not being the cause of the ulcerative colitis, eliminating milk may improve gastrointestinal symptoms in these people. It is important to be sure that the diet is nutritionally adequate, and this may require the assistance of a dietician.
Donât Miss: Preventing Pressure Ulcers In Nursing Homes
Recommended Reading: Ulcerative Colitis Flare Up Causes
What Is The Treatment For Ulcerative Colitis
Treatment for ulcerative colitis depends on the severity of the condition and how often a patients symptoms worsen . The goal of treatment is to reduce symptoms, and induce and maintain remission .
Ulcerative colitis is usually treated with medication to induce or maintain remissions and improve quality of life. Surgery is a last-resort for patients who have severe inflammation and life-threatening complications.
Medications used to treat ulcerative colitis include:
- Anti-inflammatory drugs
What Exams And Tests Diagnose Colitis
While unpleasant, the rectal examination is very important. Using a finger, the doctor feels inside the rectum, exploring for any masses or tumors. The color and consistency of stool can be evaluated, and if it is not grossly bloody, can be tested for occult blood .
Laboratory Tests
The history will assist the health-care professional decide the tests to order and what cultures would be appropriate. Blood tests help assess the stability of the patient, and also explore any potential issues associated with colitis.
- A complete blood count will assess the red blood cell count, the white blood cell count, and the number of platelets.
- The red blood cell count will help define the amount of bleeding.
- White blood cell counts elevate when the body is undergoing physical , physiological, or emotional stress.
- Platelets help blood to clot, so knowing the platelet number in a patient with bleeding may be useful.
Colonoscopy
Recommended Reading: How To Eat With Ulcerative Colitis
Don’t Miss: What Are The Symptoms Of An Ulcer In Your Stomach
Taking A Look At Your Gut
Crohns and Colitis cause painful sores and inflammation in your gut. Your doctor will need to take a look directly at your gut to check if you have these ulcers. This is done by an endoscopy.
In an endoscopy, a doctor or specialist endoscopist uses an endoscope a long, thin tube with a camera in its tip to examine your digestive system. There are several types of endoscopy which can have different names according to the part of the gut being examined. The main types are:
Upper Gastrointestinal Endoscopy
This type of endoscopy goes through your mouth, and is used to examine the upper part of the digestive system the oesophagus, stomach, and duodenum . You may have this procedure if youre experiencing symptoms such as nausea and vomiting.
Colonoscopy
A colonoscopy goes through your bum to look at the whole of the large intestine, including rectum and colon.
Sigmoidoscopy
This is similar to colonoscopy but only examines the rectum and lower part of the colon.
If you have any worries about your endoscopy, discuss them in advance a with your healthcare professional. Endoscopies may be uncomfortable, so you may be offered a sedative to help you relax, but they are normally not painful. Biopsies are often taken during an endoscopy. These can then be examined under a microscope to confirm the diagnosis.
Ulcerative Colitis Diagnosis And Testing
The path to receiving a chronic disease diagnosis can be overwhelming and even frightening at times. The best thing you can do during this time is be educated and prepared. We can help you understand the process of diagnosing ulcerative colitis and learn about common procedures your healthcare team may recommend.
An ulcerative colitis diagnosis is based on several factors, including your medical history, a physical exam, and a series of medical tests. The tests your doctor recommends will help your healthcare team determine if you have ulcerative colitis and which type of ulcerative colitis you have.
Don’t Miss: Is Ashwagandha Safe For Ulcerative Colitis