Ulcerative Colitis: Symptoms Causes Treatment And More
- www.healthline.com
- Highest rating: 3
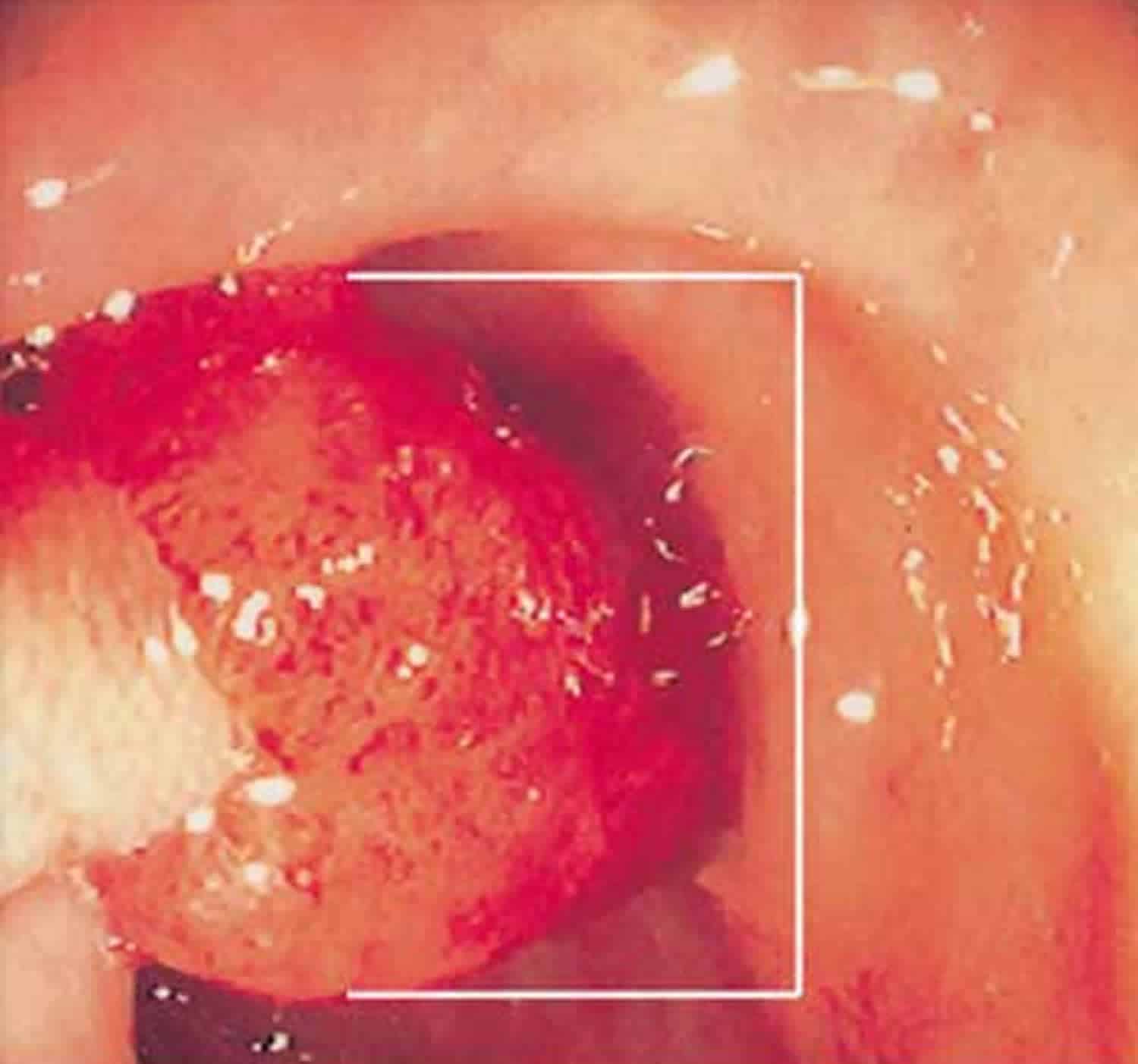
- Summary: UC occurs when the lining of your large intestine , rectum, or both become inflamed. This inflammation produces tiny sores called ulcers
See Details
- Highest rating: 3
- Summary: Small ulcers can develop on the colons lining, and can bleed and produce pus. Symptoms of ulcerative colitis. The main symptoms of ulcerative colitis are:.
See Details
- Highest rating: 3
- Summary: Ulcers are sores in the lining of the large intestine caused by inflammation due to a disease called Ulcerative colitis, also called colitisor proctitis.
See Details
Also Check: What Foods To Avoid When You Have An Ulcer
What Tests Are There For A Stomach Ulcer
If your doctor thinks you may have a stomach ulcer, the initial tests will include some blood tests. These tests will help to check whether you have become anaemic because of any bleeding from the ulcer. The blood test will also check to see that your liver and pancreas are working properly.
The main tests that are then used to diagnose a stomach ulcer are as follows:
- A test to detect the H. pylori germ is usually done if you have a stomach ulcer. The H. pylori bacterium can be detected in a sample of stool , or in a breath test, or from a blood test, or from a biopsy sample taken during a gastroscopy. See the separate leaflet called Helicobacter Pylori for more details.
- Gastroscopy is the test that can confirm a stomach ulcer. Gastroscopy is usually done as an outpatient day case. You may be given a sedative to help you to relax. In this test, a doctor looks inside your stomach by passing a thin, flexible telescope down your gullet . The doctor will then be able to see any inflammation or ulcers in your stomach.
- Small samples are usually taken of the tissue in and around the ulcer during gastroscopy. These are sent to the laboratory to be looked at under the microscope. This is important because some ulcers are caused by stomach cancer. However, most stomach ulcers are not caused by cancer.
Drugwatchcom Has Been Empowering Patients For More Than A Decade
Drugwatch.com has provided reliable, trusted information about medications, medical devices and general health since 2008. Weve also connected thousands of people injured by drugs and medical devices with top-ranked national law firms to take action against negligent corporations.
Our team includes experienced medical writers, award-winning journalists, researchers and certified medical and legal experts. Drugwatch.com is HONCode certified. This means the high-quality information we provide comes from credible sources, such as peer-reviewed medical journals and expert interviews.
The information on Drugwatch.com has been medically and legally reviewed by more than 30 expert contributors, including doctors, pharmacists, lawyers, patient advocates and other health care professionals. Our writers are members of professional associations, including American Medical Writers Association, American Bar Association, The Alliance of Professional Health Advocates and International Society for Medical Publication Professionals.
Recommended Reading: Ulcerative Colitis Causes And Treatment
Stomach Ulcer Remedies: 10 Ways To Heal And Reduce Inflammation
An ulcer is a kind of erosion or open sore on the surface of an organ or tissue. Ulcers generally occur in the esophagus, stomach, and duodenum and are known as peptic ulcers.
Types of Peptic Ulcers
- Gastric ulcer: A peptic ulcer in the stomach is called a gastric ulcer.
- Duodenal ulcer: A duodenal ulcer is a type of peptic ulcer that develops in the first part of the small intestine .
- Esophageal ulcer: An esophageal ulcer develops in the lower part of the esophagus.
A peptic ulcer is among the most common forms of stomach disease. About 4 million Americans suffer from this condition every year.
You May Like: Can I Donate Blood If I Have Ulcerative Colitis
Ulcerative Colitis In Children
According to one study of IBD in the United States, 1 in 1,299 children between ages 2 and 17 years old were affected by the condition in 2016. Crohns disease was twice as common as UC, and boys were more likely to have IBD than girls.
For children with IBD, a diagnosis is more likely after 10 years old.
UC symptoms in children are similar to symptoms in older individuals. Children may experience bloody diarrhea, abdominal pain and cramping, and fatigue.
In addition, they may experience issues compounded by the condition, such as:
- anemia due to blood loss
- malnutrition from poor eating
- unexplained weight loss
UC can have a significant effect on a childs life, especially if the condition isnt treated and managed properly. Treatments for children are more limited because of possible complications. For example, medicated enemas are rarely used as a treatment method in children.
However, children with UC may be prescribed medications that reduce inflammation and prevent immune system attacks on the colon. For some children, surgery may be necessary to manage symptoms.
If your child has been diagnosed with UC, its important that you work closely with their doctor to find treatments and lifestyle changes that can help. Check out these tips for parents and children dealing with UC.
Don’t Miss: Dog Skin Ulcer Home Treatment
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
You May Like: Stage Iv Sacral Decubitus Ulcer
Is Ulcerative Colitis A Genetic Disease
Nearly 15% of those with Ulcerative Colitis have a first degree relative who also suffers from the condition. In identical twins, the rate of UC is about 16%, whereas in non-identical twins that number drops to 4%.
The exact genes are yet to be determined, but the following highlights some of the newest research on genetics and Ulcerative Colitis:
- A total of163 at-risk genes/loci have been identified in UC. A large study of 29,838 IBD patients recently identified three new loci in association with inflammatory bowel disease: NOD2, MHC, and MST1 3p21.
- IL-13 is the main interleukin responsible for the inflammation and chronic symptoms of UC. It causes epithelial barrier damage, reduces the speed of mucosal repair, and contributes to alterations of the tight junctions in the gut. The addition of IL-13 to cell cultures increases the flux of large molecules such as mannitol and lactulose and also affects the speed of mucosal repair by 30%.
- IL-10 is an anti-inflammatory cytokine which has a positive effect on UC. It inhibits the production of certain players that cause inflammation and the inactivation of IL-10 was shown to cause chronic ileocolitis in mice, indicating a protective role within the mucosal layer.
So, what does this all mean?
Genetics certainly play a role when it comes to UC, but genetics alone arenât enough to explain why IBD has jumped from 2 million people in 1999 to over the 3 million mark weâre seeing today.
What Causes Gi Bleeding
Many conditions can cause GI bleeding. A doctor can try to find the cause of your bleeding by finding its source. The following conditions, which are listed in alphabetical order, include possible causes of GI bleeding:
Angiodysplasia. Angiodysplasia is when you have abnormal or enlarged blood vessels in your GI tract. These blood vessels can become fragile and bleed.
Benign tumors and cancer.Benign tumors and cancer in the esophagus, stomach, colon, or rectum may cause bleeding when they weaken the lining of the GI tract. A benign tumor is an abnormal tissue growth that is not cancerous.
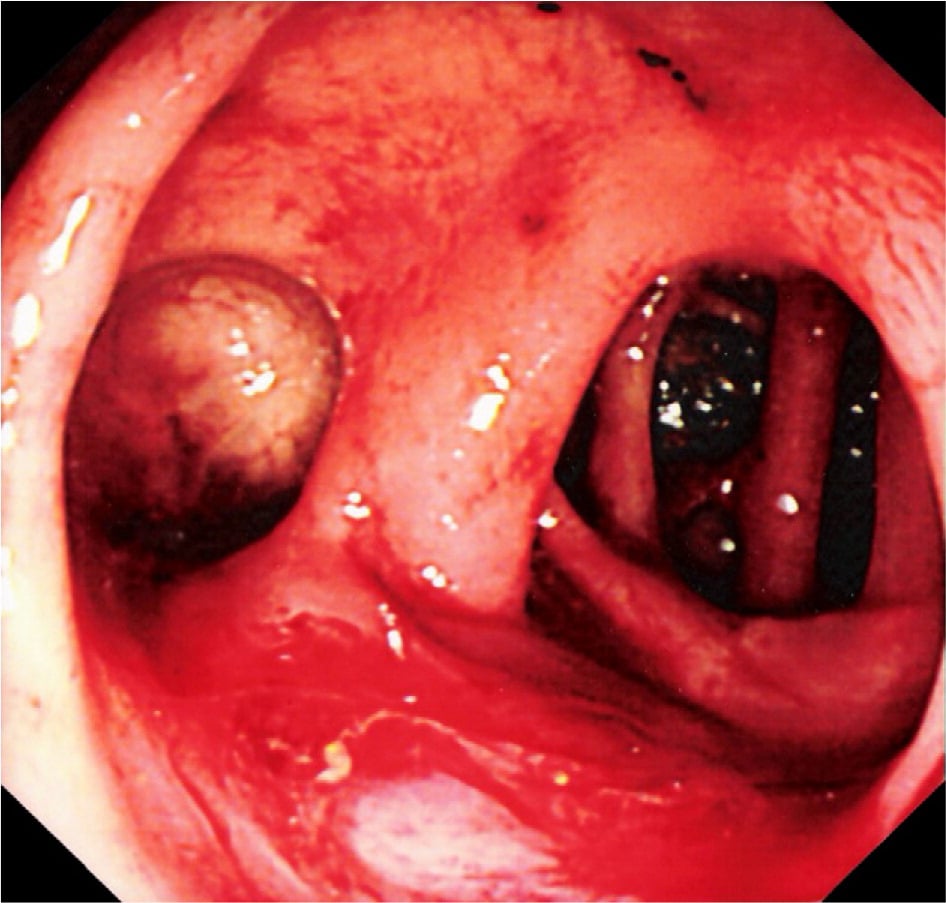
Colitis. Ulcers in the large intestine are a complication of colitis. Ulcerative colitis is an inflammatory bowel disease that can cause GI bleeding.
Colon polyps.Colon polyps can cause GI bleeding. You can have more than one colon polyp at a time. Some types of polyps may be cancerous or can become cancerous.
Diverticular disease.Diverticular disease can cause GI bleeding when small pouches, or sacs, form and push outward through weak spots in your colon wall.
Esophageal varices.Esophageal varices can cause GI bleeding. Esophageal varices are usually related to a chronic liver condition called cirrhosis.
Esophagitis. The most common cause of esophagitis is gastroesophageal reflux . GER happens when your lower esophageal sphincter is weak or relaxes when it should not. Stomach acid can damage your esophagus and cause sores and bleeding.
Gastritis. Some common causes of gastritis include
Don’t Miss: Does Ulcerative Colitis Cause Acne
News Result For Ulcers In Stomach Symptoms
Jagran Dialogues: Troubled by gastric problems? Know its causes, symptoms and treatment from expertYour browser indicates if youve visited this link
Jagran
Jagran Dialogues: Troubled by gastric problems? Know its causes, symptoms and treatment from expertYour browser indicates if youve visited this link
Jagran
The official NHS list of the 20 most painful health conditions UK people are living with right nowYour browser indicates if youve visited this link
leeds-live
The official NHS list of the 20 most painful health conditions UK people are living with right nowYour browser indicates if youve visited this link
leeds-live
Painkiller warning: Five sensations warning of a developing stomach ulcerYour browser indicates if youve visited this link
Daily Express
Painkiller warning: Five sensations warning of a developing stomach ulcerYour browser indicates if youve visited this link
Daily Express
20 ulcer symptoms to watch out forYour browser indicates if youve visited this link
symptomsstomachulcerstomachstomachulcer
Gastric Ulcer vs. Peptic Ulcer: Whats the Difference?Your browser indicates if youve visited this link
U.S. News & World Report
ulcerssymptomssymptomssymptomstomach
Foods to eat and avoid on a gastritis dietYour browser indicates if youve visited this link
Medical News Today
Dont Miss: Ways To Prevent Pressure Ulcers In Hospitals
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Don’t Miss: What Causes Acute Ulcerative Colitis
Diagnosing Lower Gi Bleeding
A doctor may perform the following tests to determine the cause of lower GI bleeding:
- Colonoscopy. During a colonoscopy, your doctor will insert a small, flexible tube into your rectum. A camera is attached to the tube so your doctor can view the entire length of your colon. Air moves through the tube to provide a better view.
- Biopsy. During the colonoscopy, the doctor may take a biopsy for additional testing.
- X-ray. You may also undergo a scan to locate your GI bleeding. A harmless radioactive tracer will be injected into your veins. The tracer will light up on an X-ray so your doctor can see where youre bleeding.
- CT angiography. A CT scan is an imaging test that can help the doctor locate GI bleeding in the abdomen and pelvis. It often shows more detail than an X-ray.
- Capsule endoscopy. If your doctor cant find the source of your bleeding with an endoscopy or a GI bleeding scan, they may perform a capsule endoscopy. Your doctor will have you swallow a pill that contains a small camera that will take pictures of your bowel to find the source of your bleeding.
- RBC nuclear scan. In this exam, a doctor injects a harmless radioactive tracer to track your red blood cells. This can show how the cells perform in your body.
Two Methods For Endoscopic
Balloon-dilation methods can be divided into two general categories. One is the through-the-scope method, in which a balloon dilator is inserted through the forceps channel and dilation is done under direct observation. The other is the radiologic method, in which a guidewire is inserted endoscopically. After the endoscope is withdrawn, a balloon dilators position is aligned and dilation is done under fluoroscopy. Usually the TTS method is selected with a therapeutic scope unlike the radiologic method which is adopted when a diagnostic scope is used, since the balloon dilator does not match the diameter of the forceps channel.
Also Check: Can Ulcerative Colitis Cause Blood In Urine
Read Also: What Do I Take For An Ulcer
How Is Ulcerative Colitis Diagnosed
Colitis shares many symptoms with other common conditions, such as Crohn’s disease, irritable bowel syndrome, gastroenteritis and coeliac disease. Your doctor will examine you and take a detailed history of your symptoms to help rule these out.
There is no single test that can be used to diagnose UC, so a combination of tests is usually required:
- Blood tests help to rule out other medical conditions, and certain markers in the blood can indicate that inflammation is present.
- A stool sample may find other possible causes of diarrhoea and inflammation, such as an infection.
- A colonoscopy may be performed, where a thin, flexible tube that contains a tiny camera looks inside the bowel for ulcers, inflammation and bleeding.
- A biopsy may be taken from inside the bowel so a pathologist can examine it under a microscope to look for signs of disease.
Other types of imaging are sometimes used to help in the diagnosis and to help rule out other diseases.
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Don’t Miss: Do Ulcers Cause Weight Loss
Get Regular Exercise To Reduce Uc Inflammation
Snider says exercise is useful in managing many of the complications associated with ulcerative colitis, including decreased bone density, a weakened immune system, emotional health problems, stress, and weight gain.
âTry to engage in a moderate-intensity exercise like swimming or biking, three or four days per week,â he says. A review published in August 2016 in Pharmacological Reports noted that moderate exercise releases protective myokines such as irisin from working skeletal muscles, which promotes healing and helps with inflammatory bowel disease inflammation.
Snider also strongly recommends yoga as a natural treatment for ulcerative colitis, as it promotes relaxation and targets the digestive system, flooding the area with oxygen and nutrition for healing. Find what type and frequency of exercise works for you and take it slow: Too much exercise can cause mild systemic inflammation.
Research indicates that stress plays a role in inflammatory bowel diseases such as ulcerative colitis. Researchers analyzed data on 2,007 adults in a Swiss IBD study and found a relationship between depression and anxiety and disease symptoms. The results were published in June 2016 in Clinical Gastroenterology and Hepatology.
Counteract stress with relaxation techniques such as meditation, deep breathing, and progressive muscle relaxation to help your body relax.
How Are Peptic Ulcers Treated
The treatment for ulcers depends in part on the specific cause. If your doctor finds H. pylori in your digestive tract through a lab test, we will prescribe antibiotics that will kill the bacteria. Ulcer treatment usually also requires medication to control stomach acid, usually for 8 weeks or so. These medications include protein pump inhibitors that block the production of stomach acid.
If your ulcer is from using NSAIDs, your doctor may recommend switching medications or lowering the dose. If you require on-going pain relief from NSAIDs, we usually recommend a daily dose of a proton pump inhibitor.
Recommended Reading: Whipworm Therapy For Ulcerative Colitis
No Pouch For Crohns Disease
Because Crohnâs disease can attack the small intestine as well as the colon, the pouch is not used for Crohnâs disease. When surgeons tried the pouch for Crohnâs disease, the complication rate was very high. In most cases, the Crohnâs disease attacked the pouch and it could no longer be used.
For those with Crohnâs disease, if the colon is very diseased but the rectum is not, then the colon can be removed except for the rectum, and the small intestine can be connected directly to the rectum. In many cases, if the Crohnâs disease involving the rectum is not severe, it can be controlled with Rowasa enemas or Rowasa suppositories.
General signs of colitis can include:
- Swelling of the colon tissue
- Erythema of the surface of the colon
- Ulcers on the colon which may bleed
- Mucus and/or blood in stool and rectal bleeding
- Diarrhea, which may occur, although some forms of colitis involve constipation so the stool and bowel movements may appear normal.
Other symptoms may include gas, bloating, indigestion, heartburn, gastro esophageal reflux disease, cramps, bowel urgency and many other uncomfortable aches in the gastrointestinal system.