How Do I Take Budesonide For Inflammatory Bowel Disease
Your IBD team will give you detailed information on your dosage of budesonide for your inflammatory bowel disease and how often you should take it. You can also read the patient information leaflet included in every medicine packet.
Oral budesonide for crohn’s disease and ulcerative colitis
You will usually take budesonide tablets, capsules or granules once a day, in the morning, half an hour before breakfast.
You should swallow budesonide capsules or tablets with a glass of water, and must not chew them as this could stop them working properly. Budesonide granules can be mixed into a small amount of food to make them easier to swallow, but they must not be chewed.
Oral budesonide is usually prescribed as an eight week course of treatment, and your IBD team may ask you to reduce your dose gradually towards the end of your treatment. It is important you dont suddenly stop taking budesonide, even if you feel better, as this could make you very unwell.
Topical budesonide for UC
Budesonide enemas are usually used once a day for between four and eight weeks. Budesonide rectal foam is usually used once a day for between six and eight weeks.
Budesonide enemas and rectal foams are inserted through your anus using a specially designed applicator, delivering medicine into your rectum and the lower part of your colon .
Steroid treatment card
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
What Is Prednisone And What Is It Used For
- Prednisone is a steroid with anti-inflammatory effects. It is used to treat inflammation in ulcerative colitis and Crohns disease. However, steroids do not prevent symptoms from returning and have many side effects.
- Sometimes, it is necessary to use steroids to treat IBD, especially during flares.
Don’t Miss: How To Heal Mouth Ulcers Quick
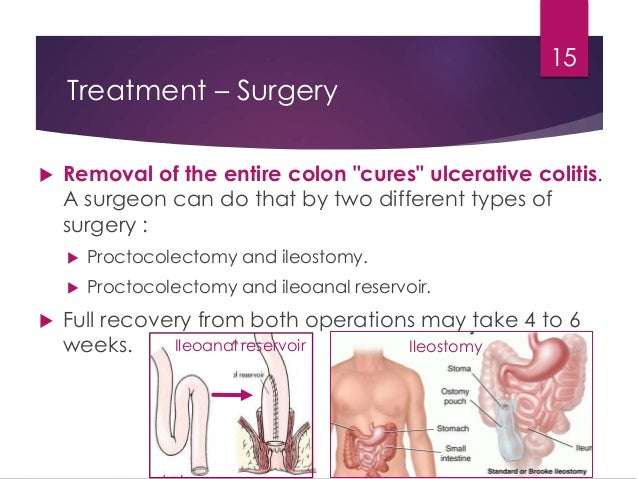
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
The medication released from a suppository will travel upward and usually reach about 15 cm inside from the anus. An enema will reach farther, about 60 cm. Those with ulcerative colitis usually insert these formulations before bedtime, and this way the medication is retained as long as possible. Stool does not typically interfere with the drug, since the bowel area is typically relatively empty right before bed.
Recommended Reading: Oral Antibiotics For Leg Ulcers
What Do I Do If I Miss A Dose
- If you are only taking prednisone once a day, take it as soon as you remember that day. If you dont remember until the next day, just take one dose do not double up on your dose.
- If you are taking Prednisone twice a day, take the missed dose as soon as you remember and resume your regular schedule.
- It is very important that you do not stop taking this drug suddenly. Doing this can have very bad side effects.
Treatment Modalities Administered For Lcv In Patients With Uc
Most patients were treated with corticosteroids . Among thee corticosteroids, prednisone or prednisolone were administered in more than 2/3 of patients . Aminosalicylates and steroid-sparing immunosuppressants were administered in nine , and eight patients, respectively. Biologic agents were given in five cases . Due to the inability to control UC disease course, colectomy was performed in two patients .
Read Also: How Do You Treat An Ulcer Naturally
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Fistulating And Perianal Disease72739596
Active perianal disease or fistulae are often associated with active CD elsewhere in the gastrointestinal tract. The initial aim should be to treat active disease and sepsis. For more complex, fistulating disease, the approach involves defining the anatomy, supporting nutrition, and potential surgery. For perianal disease, MRI and examination under anaesthetic are particularly helpful.
-
Metronidazole 400 mg tds and/or ciprofloxacin 500 mg bd are appropriate first line treatments for simple perianal fistulae.
-
Azathioprine 1.52.5 mg/kg/day or mercaptopurine 0.751.5 mg/kg/day are potentially effective for simple perianal fistulae or enterocutaneous fistulae where distal obstruction and abscess have been excluded .
-
Infliximab should be reserved for patients whose perianal or enterocutaneous fistulae are refractory to other treatment and should be used as part of a strategy that includes immunomodulation and surgery .
-
Surgery , including Seton drainage, fistulectomy, and the use of advancement flaps is appropriate for persistent or complex fistulae in combination with medical treatment .
-
Elemental diets or parenteral nutrition have a role as adjunctive therapy, but not as sole therapy .
-
There is insufficient evidence to recommend other agents outside clinical trials or specialist centres.
Don’t Miss: Early Stage Venous Leg Ulcer
How Fast Does It Work
Prednisone can have a positive effect on acute severe and sudden UC symptoms. The drugs powerful anti-inflammatory properties mean that it can help control stomach pain, diarrhea, and bloody stools, among other symptoms.
According to The Arthritis Society, prednisone usually works within 14 days if a person takes the appropriate dosage. But some people may experience symptom relief within just a few hours. How quickly it works depends on how a person takes it and whether the drug is formulated for immediate or delayed release.
What Are The Treatment Options For A Flare
When you first develop ulcerative colitis it is usual to take medication for a few weeks until symptoms clear. A course of medication is then usually taken each time symptoms flare up. The medicine advised may depend on the severity of the symptoms and the main site of the inflammation in the colon and the rectum .
Topical treatments applied locally by an enema or suppository are widely used for treating ulcerative colitis, particularly aminosalicylate and steroid medicines see below. They are a treatment option if ulcerative colitis affects only the lower part of the bowel .
Medication options include the following:
Read Also: Where Are Stomach Ulcers Located
Recommended Reading: Is Peppermint Tea Good For Ulcerative Colitis
Steroid Use And Misuse
We aim to highlight misuse of steroids in clinical practice through clinical case scenarios, and highlight how timely recognition and intervention with steroid-sparing strategies can reduce the need for steroids and their unwanted side effects in people living with IBD.
Definitions of steroid use
The British Society of Gastroenterology and European Crohns and Colitis Organisation have defined steroid use in IBD as follows :
Steroid relapse disease relapse within 3 months of stopping steroids.
Steroid refractory active disease despite prednisolone 1 mg /kg/day for a period of 4 weeks.
Steroid dependent unable to reduce steroids below the equivalent of prednisolone.
10 mg/day or budesonide 3 mg/day within 3 months of starting steroids without recurrent active disease.
Oral Budesonide For Treatment Of People With Active Ulcerative Colitis
What is ulcerative colitis?
Ulcerative colitis is a debilitating long-term , inflammatory bowel disease that affects the large bowel. When people with ulcerative colitis are experiencing symptoms which may include bleeding, diarrhoea and abdominal pain, the disease is said to be ‘active’ periods when the symptoms stop are called ‘remission’. A common initial treatment of ulcerative colitis is oral steroid therapy. Unfortunately, conventional steroids are usually absorbed into the body and cause significant unwanted side-effects. These may include but are not limited to weight gain, diabetes, growth retardation, acne, mood instability, and high blood pressure.
What is budesonide?
Budesonide is a steroid that is quickly metabolised by the liver thereby reducing corticosteroid-related side-effects. There are currently three formulations of budesonide: two standard capsules both designed to release the drug in the outer part of the small intestine and right colon and the newer Budesonide-MMX® capsule designed to release the drug throughout the entire colon.
What did the researchers investigate?
The researchers investigated whether budesonide produces remission in people with active ulcerative colitis and whether these medications cause any harm . The researchers searched the medical literature up to April 28, 2015.
What did the researchers find?
Don’t Miss: What Is The Difference Between Colitis And Ulcerative Colitis
Check In Check Up: Ulcerative Colitis
You dont have to settle for good enough ulcerative colitis care. Take this series of assessments to evaluate how well your treatment is working.
Prednisone, hydrocortisone, and methylprednisolone work by suppressing the entire immune system, rather than targeting specific inflammatory pathways.
If you take corticosteroids orally or by injection, you may have significant side effects. Local steroids which are applied just to the area that needs treatment are generally the preferred option.
Steroids are ineffective as maintenance therapy to keep ulcerative colitis in remission.
According to Mayo Clinic, possible side effects of steroids include:
- Infection
Before you begin a course of treatment using an immunomodulator, its important to have a recent complete blood count and continue periodic monitoring of your blood levels and chemistry while taking the drug.
Corticosteroids For The Induction Of Remission
Ulcerative colitis
In the seminal double-blind randomised placebo-controlled trial by Truelove and Witts in 210 patients with ulcerative colitis, treated with 100mg cortisone, 41.3% of patients achieved remission at 6 weeks compared to 15.8% in the placebo arm2. Subsequent studies, including the meta-analysis of 5 randomised controlled trials, reported that corticosteroids are more effective than placebo for inducing remission in active UC . Second generation corticosteroids including various preparation of Budesonide MMX as well as multimatrix system enabling targeted release in the colon and beclomethasone dipropionate have emerged as alternatives. In a pooled analysis of the CORE I & II studies, Budesonide MMX 9mg/day demonstrated a combined clinical and endoscopic remission rate of 17.7% versus 6.2% for placebo. Both clinical and endoscopic remission were significantly better with Budesonide MMX in left-sided but not extensive disease. While budesonide MMX still has glucocorticoid side effects , there are lower rates of side effects and no association with adrenal suppression or significant reduction in bone mineral density. BDP was demonstrated to be non-inferior to tapered prednisolone , achieving clinical response in 64.6% for BDP vs. 66.2% for prednisolone. However, there was also no difference in the co-primary end-point of steroid-related adverse events and reduction in morning cortisol below 150nmol/L.
Crohns disease
You May Like: How Do They Treat Stomach Ulcers
What Will You Need
Your needs will depend on your symptoms, and each person is different. Your ulcerative colitis could start out as mild, then stop for a while, only to come back worse than it was before. Or you may have only mild ulcerative colitis your entire life.
Plus, your body may not respond the same way to a drug as someone else’s. And over time, you may find that you need a different type of medicine. For example, something thatâs worked well for years may not work anymore. You may need a whole new treatment plan.
Let your doctor know how youâre really doing, and always tell them about any side effects that you have.
Show Sources
Who Gets Ulcerative Colitis And What Causes It
Colitis can develop at any age, but usually first appears in people aged 15 to 30.
Experts are not sure why UC or Crohns disease occurs in some people. It may be due to a combination of genetic, environmental and infectious factors that cause a fault in the immune system leading to inflammation of the bowel.
Read Also: Can Stomach Ulcers Cause Bloating
Read Also: Safety Considerations For Ulcerative Colitis
What Side Effects Might Happen
Because systemic steroids slow down your immune system to reduce inflammation, your defenses against germs are much lower while youâre taking them. This means youâre at a higher risk for infection. People on steroids commonly deal with:
- Vaginal yeast infection
- Yeast infections of the mouth
The side effects you get from a systemic steroid will depend on how strong a dose youâre on and how long you take it. But many different side effects are possible and common, including:
- Acne
- Stretch marks
- Weight gain
Some side effects go away once you stop taking the steroid. Thatâs not the case for cataracts and osteoporosis, though. Your doctor may recommend you take extra calcium and vitamin D to help counteract the effects of osteoporosis . Cataracts also require extra treatment, even after stopping the steroid.
Medication Options For Ulcerative Colitis
Medication is the first line of treatment for ulcerative colitis. Your doctors recommendation for which medication will work best for you is based on the severity of your disease, your overall health, and other individual factors.
There are six major classes of medication used to treat ulcerative colitis.
Recommended Reading: Best Vitamins For Ulcerative Colitis
What Is Considered Long
Long-term prednisone use is the use of the medication for more than a month.
Using prednisone long term can have adverse effects. The longer the treatment time, the more negative side effects can be expected.
Long-term use of corticosteroids can cause other conditions, such as diabetes, cataracts, high blood pressure, and osteoporosis.
To manage UC long term, talk to your healthcare provider about other options for controlling your disease.
What Are The Symptoms Of Ulcerative Colitis
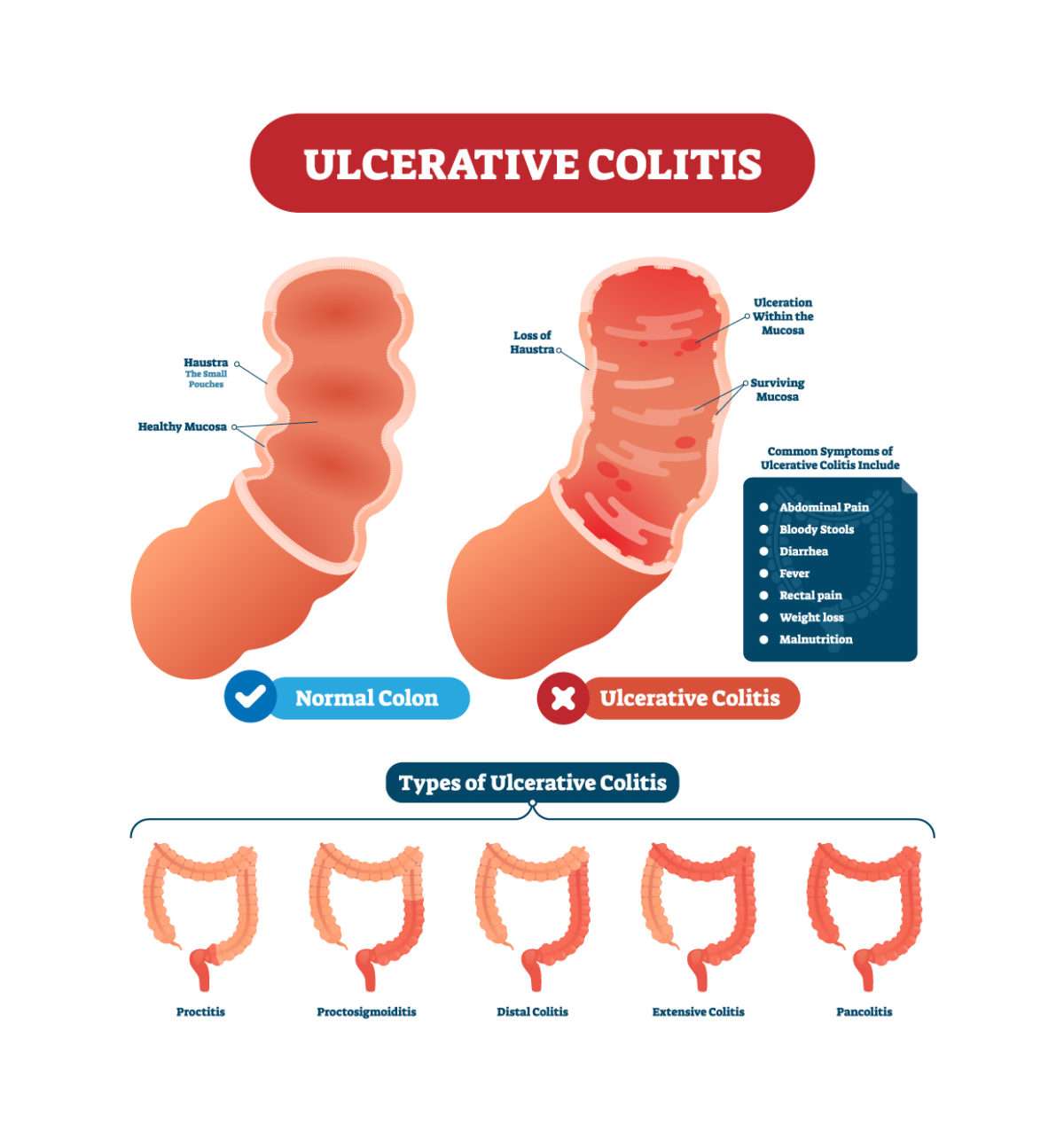
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Liver disease.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Read Also: Ulcerative Colitis And Apple Cider Vinegar
Lifestyle Changes For Ulcerative Colitis
While medical treatment can help control UC and keep it in remission, changing certain lifestyle factors can also help you live well with the disease.
These changes can help lessen the severity of UC. If your UC does worsen, being continuously monitored by your healthcare team can boost chances of early detection and improve colon cancer survival rates.
Lifestyle changes you can consider making include:
- Having regular cancer screening via colonoscopy
- Seeing your gastroenterologist annually, or more often as needed
- Eating a diet that is high in vegetables, fruits, and whole grains
- Limiting dairy product intake
- Reducing your intake of red meat and processed meats, which are connected to risk of colorectal cancer
- Limiting alcohol intake or avoiding it altogether
- Drinking a lot of liquids, all day long
- Eating smaller meals throughout the day
- Exercising regularly
Beclomethasone Vs Conventional Steroids In Uc
Balzano et al. evaluated the efficacy of oral beclomethasone and oral prednisone in a mild to moderately active UC population, in an 8-week, multicentre, randomized, double-blind study. Both drugs achieved comparable clinical and endoscopic efficacy, with oral beclomethasone presenting less steroid-related adverse effects. Out of the context of controlled clinical trials, data suggests that oral beclomethasone also manages to achieve impressive remission rates. In a very recently published, large retrospective study aiming at evaluating oral beclomethasone efficacy in the clinical practice scenario, oral beclomethasone induced remission in more than 40% and response in two thirds of UC patients. In addition, patients with left-sided or extensive, mild or moderately active UC treated for more than 4 weeks presented the best outcome.
You May Like: Bleeding Ulcer Treatment At Home