How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
Ulcerative Colitis: Treatment And Therapy
The cause of the inflammatory bowel disease ulcerative colitis is not yet known. Therefore, the goal of treatment is to alleviate the symptoms as well as to prolong the symptom-free phases.
Various drugs are used for this purpose: 5-aminosalicylic acid is an anti-inflammatory agent that is prescribed in the form of the precursor mesalazine as tablets, suppositories, foams or enemas. Corticosteroids also have an anti-inflammatory effect and are used either as suppositories, enemas or tablets. Both medications containing the active ingredient mesalazine and cortisone can cause severe side effects. Cortisone in particular can cause long-term side effects.
In severe cases or when cortisone is not effective, some patients receive immunosuppressants . This can have a positive effect on the course of the disease. However, TNF antibodies , which inhibit the inflammatory messenger TNF, can also be considered. When taking immunosuppressants and TNF antibodies, severe side effects such as susceptibility to infections can also occur, and poisoning is also possible.
Which drugs are used in treatment always depends on various factors, such as the extent of the symptoms and how far the inflammation has spread in the intestine, among other factors.
In addition to drug therapy, it is important for those affected to ensure a varied and balanced diet and to avoid hard-to-digest food components and hot spices during an acute episode.
Also Check: Natural Way To Cure Ulcer
Also Check: Stomach Ulcer Treatment In Homeopathy
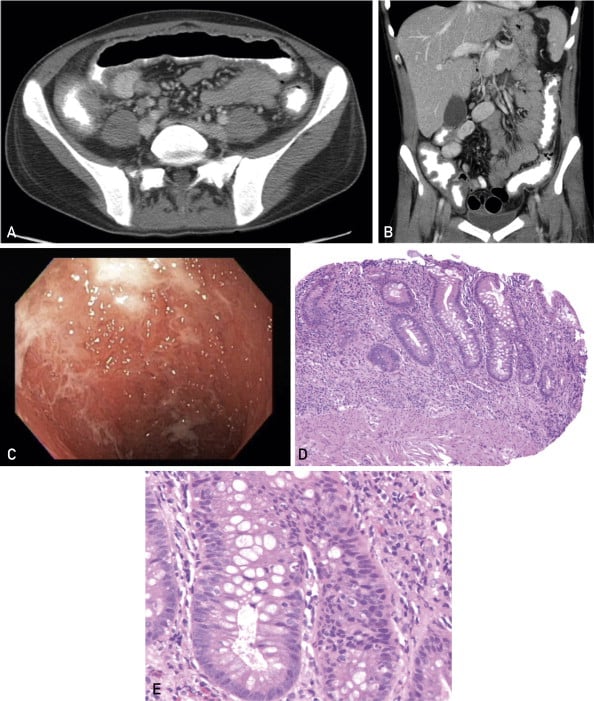
Diagnosis Of Ulcerative Colitis
X-rays of the abdomen taken after barium is given by enema do not require any special preparation . These x-rays usually can show a blockage or paralysis read more ) may indicate the severity and extent of the disease but are not done when the disease is active, such as during a flare-up, because of the risk of causing a perforation. Other x-rays of the abdomen may also be taken.
What Kind Of Diet Is Helpful For Living With Colitis
Your healthcare provider may suggest one or several of these diets, depending on the type of colitis you have and the condition youre in:
- Low-residue diet. A low-residue diet is easy to digest when your symptoms are acute or severe. It limits fiber and fat and emphasizes soft, well-cooked foods. If you have a temporary infection or radiation colitis, your healthcare provider may recommend a low-residue diet.
- Anti-inflammatory diet. To keep chronic inflammation low, your healthcare provider might recommend you avoid highly inflammatory foods, especially fast and processed foods high in sugar and fat. They might suggest more healthy, unsaturated fats to calm inflammation like olive oil, avocados, nuts and oily fish.
- Elimination diet. If you have an inflammatory bowel disease, your healthcare provider will likely recommend an elimination diet to isolate the foods that cause your symptoms to flare up. An elimination diet eliminates certain types of foods and then adds them back in a systematic way so that you can observe how your gut responds to them. After the temporary elimination diet, you can use what you learned to design a personalized, long-term maintenance diet.
A note from Cleveland Clinic
Last reviewed by a Cleveland Clinic medical professional on 06/22/2022.
References
Recommended Reading: How To Treat Gum Ulcers
Ulcerative Colitis Symptoms And Causes Mayo Clinic
Posted: December 27, 2018 at 4:45 pm
This post was added by Alex Diaz-Granados
OverviewIBD blogRead Mayo’s IBD blog, discussing the latest advances in Crohn’s disease and ulcerative colitis.
Ulcerative colitis is an inflammatory bowel disease that causes long-lasting inflammation and ulcers in your digestive tract. Ulcerative colitis affects the innermost lining of your large intestine and rectum. Symptoms usually develop over time, rather than suddenly.
Ulcerative colitis can be debilitating and can sometimes lead to life-threatening complications. While it has no known cure, treatment can greatly reduce signs and symptoms of the disease and even bring about long-term remission.
Ulcerative colitis care at Mayo Clinic
Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs. Signs and symptoms may include:
Most people with ulcerative colitis have mild to moderate symptoms. The course of ulcerative colitis may vary, with some people having long periods of remission.
Doctors often classify ulcerative colitis according to its location. Types of ulcerative colitis include:
See your doctor if you experience a persistent change in your bowel habits or if you have signs and symptoms such as:
Although ulcerative colitis usually isn’t fatal, it’s a serious disease that, in some cases, may cause life-threatening complications.
Ulcerative colitis affects about the same number of women and men. Risk factors may include:
Link:
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Read Also: Remicade Vs Humira Ulcerative Colitis
Recommended Reading: What Is A Duodenal Ulcer And How Is It Caused
Preparing For Your Appointment
Symptoms of ulcerative colitis may first prompt you to visit your elementary wish doctor. Your sophisticate may recommend you see a specialist who treats digestive diseases .
Because appointments can be brief, and there s often a set of information to discuss, it s a good idea to be well prepared. here s some information to help you get quick, and what to expect from your sophisticate .
You May Like: What To Eat With Gastric Ulcer
What Are The Signs & Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are cramping belly pain and diarrhea. Other symptoms include:
- blood in the toilet, on toilet paper, or in the stool
- urgent need to poop
Ulcerative coliits can cause other problems, such as rashes, eye problems, joint pain and arthritis, and liver disease. Kids with ulcerative colitis may not grow well as well as other kids their age and puberty may happen later than normal.
Also Check: Turn Clock For Pressure Ulcer Prevention
Treatment Of Collagenous Colitis And Lymphocytic Colitis
- Watchful waiting some patients with mild symptoms improve without any treatment, for reasons unknown.
- Dietary changes some foods and drinks aggravate diarrhoea. Your doctor may advise you to cut down on fatty or spicy foods, milk products, alcohol, sugary drinks and caffeine. Avoid gas-promoting products such as beans, cabbage and fizzy drinks. Opt for soft and easy to digest foods such as bananas and rice. Eat frequent small meals throughout the day, rather than three large meals.
- Switching medicines some evidence suggests that non-steroidal anti-inflammatory drugs, including aspirin and ibuprofen, can worsen symptoms. Your doctor may recommend that you try different medicines, if possible, to see if symptoms improve.
- Anti-diarrhoea medication this slows the passage of faeces through the colon.
- Other medications if the above measures dont seem to help, your doctor may suggest stronger medications such as corticosteroids to help ease the symptoms. Non-absorbable steroids often help. Medications containing 5-aminosalicylic acid may also help.
- Surgery would rarely be necessary.
Study Variables And Statistics
We studied and compared patients with CD and UC, regarding the following variables: follow-up demographic characteristics and clinical data .
Descriptive analysis included absolute and relative frequencies for categorical variables. Quantitative continuous variables with normal distribution were described as means and standard deviations. For those whose normality could not be determined, we described as medians with the first and third quartiles . To compare quantitative variables of normal unpaired distribution, Students t-test for independent samples for two groups was utilized. For unpaired samples that did not assume a normal distribution, the MannWhitney test was used for two groups and one-way ANOVA for comparisons between three groups. To compare categorical variables, the chi-square test for independent samples and the equality of proportions test were performed when appropriate. Descriptive levels of p< 0.05 were considered significant.
Dont Miss: Chicken Recipes For Ulcerative Colitis
You May Like: What Is A Decubitus Ulcer Why Does It Occur
Is This My Fault
No. Scientists dont really know why your immune system starts to go haywire and inflames your bowel in ulcerative colitis. What seems fairly clear, though, is that it has little to do with what youve done in the past. You didnt catch UC from some infected person or from eating or drinking the wrong thing. Nor did you get it from simply being stressed out.
That said, both hard-to-digest foods and stressful situations can trigger or worsen a flare-up of UC symptoms, if you already have the disease. You can often improve your symptoms if you avoid certain high-fiber foods like uncooked veggies, nuts and seeds, as well as fatty or greasy foods like burgers and fries. Use common sense. If you find that certain foods upset your stomach, try to stay away from them.
It can also help to maintain balanced mental health and avoid unnecessary stress and anxiety. Proper sleep, quitting smoking, and regular exercise could also keep flare-ups at bay.
Diagnosis Of Collagenous Colitis And Lymphocytic Colitis
- physical examination
- tests to rule out other gastrointestinal diseases
- biopsy, the removal of a small tag of tissue for examination in a laboratory, is essential for diagnosis. Changes, including an abnormally thick collagen layer or a build-up of lymphocytes, are visible under the microscope. Multiple biopsies must be taken.
Recommended Reading: Signs Of Ulcers In Humans
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Does Colitis Go Away
Acute colitis that is caused by a temporary infection, food intolerance or radiation exposure typically goes away by itself. Infections take about a week, while radiation colitis takes a few months. Some types of infection may need to be treated with antibiotics to go away, especially parasite infections. Allergic colitis goes away when the substance your child was allergic to has cleared from their body.
Colitis that is an acute reaction to a chronic condition needs treatment to go away. Ischemic colitis resulting from intestinal ischemic syndrome wont go away until blood flow is restored to your colon. Diversion colitis in people with colostomies wont go away until the colostomy is reversed and the full use of your colon is restored . In some people, these solutions arent possible.
Chronic colitis that is caused by inflammatory bowel disease is a lifelong condition. It wont go away forever, but it can go away for a while. This is called remission. Treatment for IBD is focused on improving your symptoms and making remission last as long as possible. This is also true if your colitis is caused by another condition that cant be cured. In some cases, surgery can make it go away.
Read Also: Can A Bleeding Ulcer Cause Blood In Urine
Mayo Score / Disease Activity Index For Ulcerative Colitis
- Patients with known ulcerative colitis, particularly when considering changing, adding, or stopping a UC medication this is not a tool to diagnose ulcerative colitis.
- The Mayo Score is the most commonly used scoring system for UC in clinical trials and routine practice .
- The Mayo Score for Ulcerative Colitis was developed to standardize the severity of a patient’s ulcerative colitis symptoms, which is particularly helpful to assess response to treatment over time.
- The Mayo Score for Ulcerative Colitis was originally devised in 1987 for a clinical trial for pH dependent 5-ASA at the Mayo Clinic.
- Comprised of 4 parts: stool frequency, rectal bleeding, endoscopic findings and physicians global assessment, each scored from 0-3.
- The physicians global assessment accounts for other signs/symptoms including abdominal pain, physical exam findings , functional status, and the patients overall sense of well being.
- Total scores range from 0-12 with higher scores indicating increased severity of disease.
- Response to therapy is defined differently in each trial, but most use a decrease of 3 or more points.
- Remission is often defined as a total score of 2 or less with all individual categories 1. Occasionally, remission is defined stringently as a score of 0.
- Most clinical trials define mucosal healing as an endoscopic score of 0 or 1, although numerous other endoscopic scoring systems exist .
Points to keep in mind:
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Also Check: Mouth Ulcer Treatment At Home
When To See A Doctor
See your doctor if you experience a persistent change in your bowel habits or if you have signs and symptoms such as:
- Ongoing diarrhea that doesn’t respond to over-the-counter medications
- Diarrhea that awakens you from sleep
- An unexplained fever lasting more than a day or two
Although ulcerative colitis usually isn’t fatal, it’s a serious disease that, in some cases, may cause life-threatening complications. Read more about ulcerative colitis.
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Read Also: Crohn’s Vs Ulcerative Colitis Treatment
Webinar Safe Treatment Of Ibd Patients With Thiopurines: Tpmt Genotyping And Phenotyping
Thiopurine methyltransferase testing is important in the detection of individuals with altered TPMT activity who are at risk for severe hematopoietic toxicity when taking thiopurine medications . This webinar will outline the different tests to detect patients who are at risk for thiopurine-related toxicity and the advantages of each test. It is intended to educate clinicians and increase their confidence when treating patients with thiopurine medications.
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
Read Also: How Do You Get A Peptic Ulcer