How Are Causes And Risk Factors The Same And Different
Doctors arenât sure what causes you to get UC or diverticulitis, but the two conditions have some common risk factors:
- Age. Your odds for either condition go up as you get older.
- Race. White people are more likely than those of any other race to have UC or diverticulitis.
UC might be caused by an abnormal immune response in your body. This means that if your immune system is fighting off a virus or bacteria, it may mistakenly attack cells in your digestive tract, too.
Genes might also play a role. If a close relative like your parent or sibling has UC, youâre more likely to have it, too. If youre of Ashkenazi Jewish descent , your risk is even higher. Diet and stress donât cause UC, but they may trigger your symptoms and cause flare-ups.
As for what causes diverticulitis, experts believe bacteria found in your poop might get pushed into the bulging sacs as it passes through the colon. This causes the sacs to become infected or inflamed. Another theory is that your poop, especially if youâre constipated, might put a lot of pressure against the colon walls as it passes through. This can cause tears in the sacs and increase your chances of an infection.
Other risk factors for diverticulitis include:
- Diet low in fiber and high in animal fat
- Certain medications
Dietary And Lifestyle Modifications
As most nutrients are absorbed higher up in the digestive tract, those with ulcerative colitis generally do not have nutrient deficiencies however, other factors might influence your nutritional state. Disease symptoms may cause food avoidance, leading to food choices that might not provide a balanced diet. If bleeding is excessive, problems such as anemia may occur, and modifications to the diet will be necessary to compensate for this.
Generally, better overall nutrition provides the body with the means to heal itself, but research and clinical experience show that diet changes alone cannot manage this disease. Depending on the extent and location of inflammation, you may have to follow a special diet, including supplementation. It is important to follow Canadas Food Guide, but this is not always easy for individuals with ulcerative colitis. We encourage you to consult a registered dietitian, who can help set up an effective, personalized nutrition plan by addressing disease-specific deficiencies and your sensitive digestive tract. Some foods may irritate the bowel and increase symptoms even though they do not worsen the disease.
In more severe cases, it might be necessary to allow the bowel time to rest and heal. Specialized diets, easy to digest meal substitutes , and fasting with intravenous feeding can achieve incremental degrees of bowel rest.
What To Look For
The key is to pay attention to your specific symptoms. The more you’re aware of them, the better able you are to spot changes.
And there are lots of ways your symptoms can change. You might get new ones. Or the ones you have may get worse, last longer, or come on more often.
Usually, a flare-up brings at least:
- An urgent need to poop
- Blood or mucus in your stool
- Cramps in your lower belly
If it spreads to more areas of the colon, everything gets more intense. You have more diarrhea. Cramps get more severe. You have more mucus, pus, and blood in your stool. Pain in your belly gets worse and more widespread, especially up the left side. It can also affect your desire to eat and cause you to lose weight.
And some of those symptoms may just be signs of a stronger flare-up. You’ll need to see your doctor to find out for sure. Read more on ulcerative colitis symptoms to look for.
Recommended Reading: What Is Good For Mouth Ulcers
Articles On Ulcerative Colitis Overview
Ulcerative colitis affects your colon, which is part of your digestive system. A lot of things can cause trouble in that general area, so how do you know what it feels like to have ulcerative colitis?
It depends on how severe it is, and on what part of your colon is affected.
Also, symptoms can come and go. You might not have any for weeks, months, or even years, and then they come back. Chances are about 50-50 that the effects will be mild.
Still, most people with the disease have a few common issues:
Dont Miss: Foods That Irritate Stomach Ulcers
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Read Also: Remicade Vs Humira Ulcerative Colitis
You May Like: Ulcer On White Of Eye
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
A Note About Sex And Gender
Sex and gender exist on spectrums. This article will use the terms male, female, or both to refer to sex assigned at birth. .
People who receive a diagnosis before adulthood early-onset account for around 510% of all IBD cases.
Meanwhile, approximately 2535% of people with IBD are under 60. Around 15% had received a late diagnosis, while 20% diagnosed when younger now had transitioned into older age. Specifically with UC, the incidence rate increases from 1.1 per 100,000 people to 16.5 per 100,000 people per year in older people.
The onset of UC and the presentation of the disease varies across the different groups: early-onset and late-onset.
You May Like: What Happens With Ulcerative Colitis
Who Gets Ulcerative Colitis And What Causes It
Colitis can develop at any age, but usually first appears in people aged 15 to 30.
Experts are not sure why UC or Crohns disease occurs in some people. It may be due to a combination of genetic, environmental and infectious factors that cause a fault in the immune system leading to inflammation of the bowel.
Dont Miss: Pressure Ulcer Root Cause Analysis
How Can People With Ibd Manage Their Pain
The first step in developing a pain management approach for a patient with IBD is to determine what is causing the pain. If active IBD is causing the pain, then the first strategy is generally for healthcare providers to change or increase the medication that the patient is taking to manage the disease, such as aminosalicylates, corticosteroids, antibiotics, immunosupressants, or biologics. In many cases, treating the disease and its symptoms can be effective in reducing pain.1
However, some people may continue to experience pain despite the change in medication, or they may have pain that is not due to active IBD but some other cause. In those cases, healthcare providers may recommend trying some kind of pain relievers.
Don’t Miss: What Is An Infusion For Ulcerative Colitis
Ulcerative Colitis Risk Factors
Most people with UC dont have a family history of the condition. However, about 12 percent of people with UC do have a family member with IBD, according to research from 2014.
UC can develop in a person of any race, but its more common in white people. If youre of Ashkenazi Jewish descent, you have a greater chance of developing the condition than most other groups.
Young people with IBD may also be dealing with acne at the same time. Some older studies have suggested a possible link between the use of the cystic acne medication isotretinoin and UC. However, newer research has yet to find a definitive causal relationship.
Theres no solid evidence indicating that your diet affects whether you develop UC. You may find that certain foods and drinks aggravate your symptoms when you have a flare-up, though.
Practices that may help include:
- drinking small amounts of water throughout the day
- eating smaller meals throughout the day
- limiting your intake of high fiber foods
- avoiding fatty foods
- lowering your intake of milk if youre lactose intolerant
Also, ask a doctor if you should take a multivitamin.
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Read Also: List Of Foods To Eat When You Have An Ulcer
The Main Types Of Drugs
The aim of drug treatment for Ulcerative Colitis is to reduce inflammation. The main types of drugs are:
Aminosalicylates reduce inflammation in the lining of the intestine. Examples include mesalazine , olsalazine , sulphasalazine and balsalazide .
Corticosteroids work by blocking the substances that trigger allergic and inflammatory responses in your body. They include prednisolone, prednisone, methylprednisolone, budesonide , hydrocortisone and beclometasone dipropionate .
Immunosuppressants suppress the immune system, and reduce levels of inflammation. The main immunosuppressants used in IBD are azathioprine , mercaptopurine or 6MP , methotrexate, ciclosporin and tacrolimus. They are often used in patients who relapse when they come off steroids.
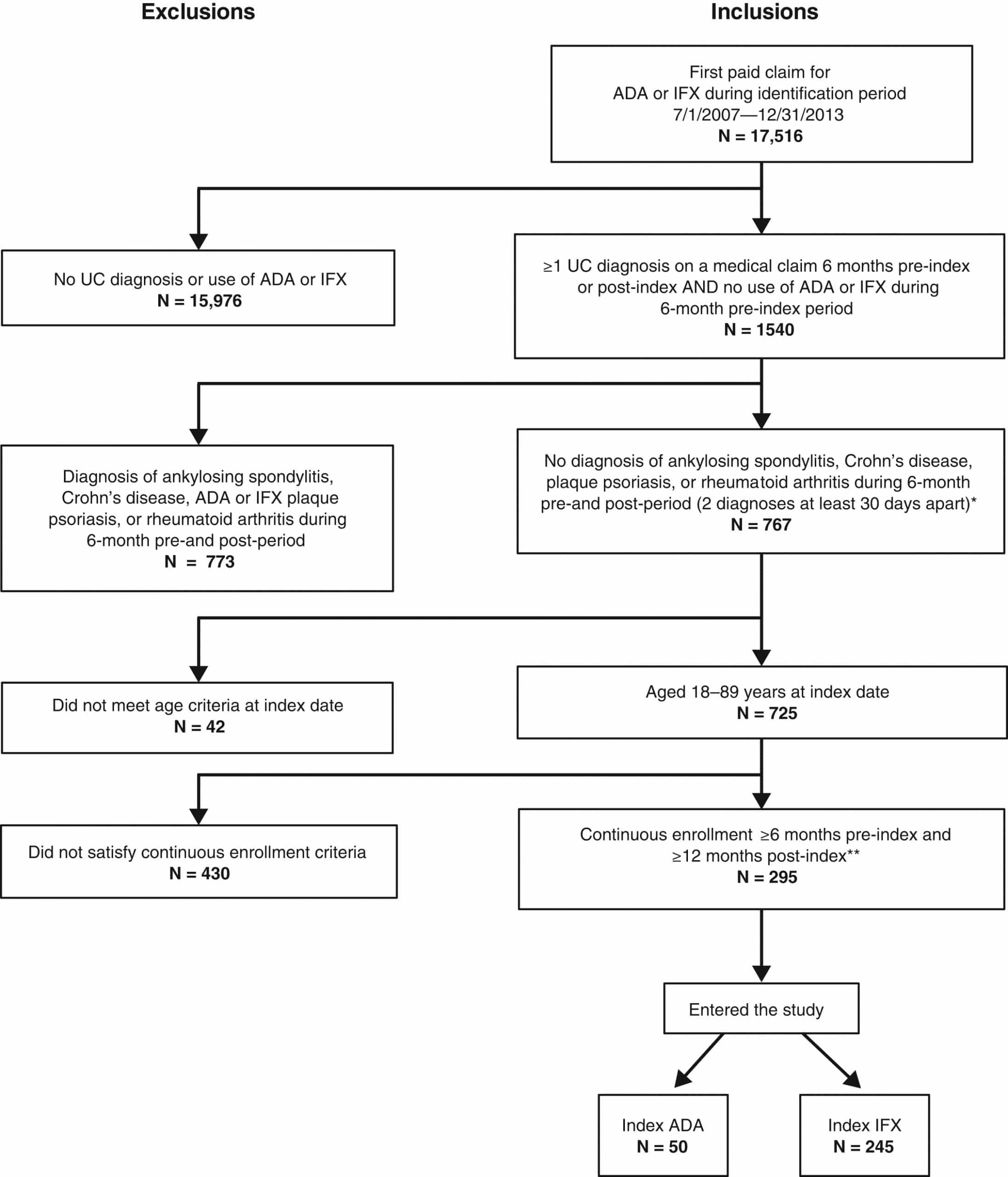
Biological drugs are the newest group of drugs used to treat IBD. Anti-TNF drugs, such as infliximab , adalimumab and golimumab target a protein in the body called TNF, or tumor necrosis factor, preventing inflammation. Another type of biological drug is vedolizumab , which works by stopping white blood cells from entering the lining of the gut and causing inflammation.
You can find more information about some of the drugs used for Colitis: Adalimumab, Aminosalicylates , Azathioprine and Mercaptopurine, Biologic Drugs, Golimumab, Methotrexate, Infliximab, Steroids, Ustekinumab and Vedolizumab.
About a quarter of people diagnosed with Crohnâs or Colitis are children or adolescents at the time they are diagnosed.
Age And Intestinal Cancer Risk
The risk of small bowel cancer and colorectal cancer in patients with CD remains debated. A meta-analysis based on population-based cohort studies exclusively , found a pooled standardized incidence ratio of CRC of 1.9 , whereas the SIR for SBC was 27.1 . Of note, the latter estimate was based on very few cases , which only resulted in the high 27-fold increased relative risk due to the extremely rare occurrence of SBC in the general population. The meta-analysis did not assess impact of age at diagnosis of CD on risk of cancer and the underlying studies either did not report on impact of age or had limited power per se to show any consistent impact. A recent nationwide Danish cohort study suggested a tendency towards increase in risk among patients diagnosed at young age, whereas a recent regional population-based study from North Jutland County, Denmark did not suggest an impact of age on risk of CRC in CD.
In contrast to intestinal cancer risk, a recent study from North Jutland, Denmark of cancer in general among patients with IBD suggested that young age at diagnosis of IBD only plays a role in CD , but not UC.
In France, in a large population-based cohort of paediatric-onset IBD patients with a median follow-up of more than 11 years there was a significant 3-fold increased risk of neoplasia with heterogeneous locations.
You May Like: Signs You May Have Stomach Ulcers
Living With Ulcerative Colitis Symptoms
Your ulcerative colitis symptoms will likely come and go, with longer periods in between flares when you may not experience any discomfort at all. Those periods are called remission, and they can span months or even years. Because there is not yet a cure for ulcerative colitis, your symptoms will eventually return.
Ulcerative colitis is an unpredictable disease, and the length of periods of remission between flares can make it difficult for doctors to evaluate whether your course of treatment has been effective or not.
Recommended Reading: How To Cure A Bleeding Ulcer
Ulcerative Colitis: Treatment And Therapy
The cause of the inflammatory bowel disease ulcerative colitis is not yet known. Therefore, the goal of treatment is to alleviate the symptoms as well as to prolong the symptom-free phases.
Various drugs are used for this purpose: 5-aminosalicylic acid is an anti-inflammatory agent that is prescribed in the form of the precursor mesalazine as tablets, suppositories, foams or enemas. Corticosteroids also have an anti-inflammatory effect and are used either as suppositories, enemas or tablets. Both medications containing the active ingredient mesalazine and cortisone can cause severe side effects. Cortisone in particular can cause long-term side effects.
In severe cases or when cortisone is not effective, some patients receive immunosuppressants . This can have a positive effect on the course of the disease. However, TNF antibodies , which inhibit the inflammatory messenger TNF, can also be considered. When taking immunosuppressants and TNF antibodies, severe side effects such as susceptibility to infections can also occur, and poisoning is also possible.
Which drugs are used in treatment always depends on various factors, such as the extent of the symptoms and how far the inflammation has spread in the intestine, among other factors.
In addition to drug therapy, it is important for those affected to ensure a varied and balanced diet and to avoid hard-to-digest food components and hot spices during an acute episode.
Also Check: Natural Way To Cure Ulcer
You May Like: How Is Ulcerative Colitis Causes
Treatments For Ulcerative Colitis
Treatments for ulcerative colitis wont cure the condition, but it can help to regulate the immune system and manage symptoms. Patients may use one type of treatment or a combination of them depending on their unique condition.
Certain medications can treat inflammation and symptoms such as diarrhea, bleeding, and abdominal pain. Medication may also be prescribed to lower the frequency of flare-ups. Alongside medication, it can be helpful for patients to alter their diet and nutrition.
Experts have found that certain foods can aggravate symptoms in UC patients. This includes spicy, high-fibers, or dairy foods. Instead, eating a healthy diet that involves softer and blander food can cause less discomfort.
In some cases, medicine and diet changes arent enough to treat UC. Surgery may be required to remove the colon and rectum completely with the creation of an ileostomy or external stoma. The type of surgical procedure for UC will greatly depend on the patients age, overall health, and symptoms.
Recommended Reading: Do You Still Have Ulcerative Colitis After Colectomy
Ulcerative Colitis In Children
According to one study of IBD in the United States, 1 in 1,299 children between ages 2 and 17 years old were affected by the condition in 2016. Crohns disease was twice as common as UC, and boys were more likely to have IBD than girls.
For children with IBD, a diagnosis is more likely after 10 years old.
UC symptoms in children are similar to symptoms in older individuals. Children may experience bloody diarrhea, abdominal pain and cramping, and fatigue.
In addition, they may experience issues compounded by the condition, such as:
- anemia due to blood loss
- malnutrition from poor eating
- unexplained weight loss
UC can have a significant effect on a childs life, especially if the condition isnt treated and managed properly. Treatments for children are more limited because of possible complications. For example, medicated enemas are rarely used as a treatment method in children.
However, children with UC may be prescribed medications that reduce inflammation and prevent immune system attacks on the colon. For some children, surgery may be necessary to manage symptoms.
If your child has been diagnosed with UC, its important that you work closely with their doctor to find treatments and lifestyle changes that can help. Check out these tips for parents and children dealing with UC.
Read Also: Best Supplement For Horses With Ulcers
Abdominal And Rectal Pain
People with ulcerative colitis often experience rectal or abdominal pain. Having a large amount of abdominal pain may be a sign that youre having a flare-up or that your condition is getting worse. Pain can range from mild to severe and may also affect your rectum.
Pain may be accompanied by persistent muscle spasms and cramping.
Does Ulcerative Colitis Reduce Immune System
Ulcerative colitis is an autoimmune condition in which the immune system attacks healthy tissue in the gut. This causes inflammation of the large intestine, which causes the symptoms of UC. Without proper treatment, UC could lower the immune system. Certain medications to treat UC may also suppress the immune system.
Recommended Reading: How To Reverse Ulcerative Colitis
Stool Ulcerative Colitis Symptoms
The severity of inflammation in a person with this disease determines the ulcerative colitis stool symptoms presented. While some patients may present some of these, others present most of them to a great degree. The more the severity of inflammation, the more predominant the persisting symptoms are. Some stool symptoms of ulcerative colitis may include:
- Abdominal pain and cramping
- Diarrhea, often with blood or pus in the stool
- Rectal bleeding, often when passing stool
With ulcerative colitis, many people notice flare-ups. They usually occur in a pattern where there comes a period with extreme or active ulcerative colitis and then one of dormancy or remission. During times of high or extreme activity of this inflammatory bowel disease, the ulcerative colitis stool symptoms are recurrent and noticeable. While in periods of dormancy, the person barely presents with any symptoms and may even think they have fully recovered from their condition.
Also Check: When Does Ulcerative Colitis Start