Primary Sclerosing Cholangitis And Cholangiocarcinoma
The possibility of developing CCA in patients with PSC is 10%. The risk is 4001,400 times higher than that of the general population,12,22 and is even higher if PSC associates with IBD.23 CCA is mainly associated with intra and extrahepatic PSC, with some cases reported in small duct PSC.24,25 Over half of patients with PSC and CCA are diagnosed at an advanced stage, in part because of the challenges of achieving an early diagnosis. Therefore, the diagnosis of CCA in patients with PSC requires a high index of suspicion and active surveillance.12
Some Of The Common Symptoms Of Ulcerative Colitis Are:
- Frequent Diarrhea
- Loss of appetite
The disease may also cause other health issues like joint pain, eye problems or the liver disease. Small ulcers in the lining of the colon could cause bleeding and the passage of mucus. Often the symptoms of ulcerative colitis might disappear, but they have a tendency to relapse. About 0.5 to 1% people out of a 100 may suffer from these symptoms all the time.
Read Also: What Is Ultra Ulcerative Colitis
Common Hepatobiliary Manifestations Of Ibd
Hepatic Steatosis is one of the more common hepatobiliary manifestations of IBD found in patients with Crohns disease and ulcerative colitis. This is characterized by large collections of fat droplets found within liver cells seen when tissue from a liver biopsy is analyzed. Hepatic Steatosis may also be seen with abdominal ultrasound with the liver appearing large and fatty. There are usually no signs or symptoms, or laboratory abnormalities to suggest fatty infiltration of the liver. As well, the presence of hepatic steatosis is usually benign and usually does not present with any further complications. However, one must realize that fatty infiltration can be directly related to the severity of the IBD, and also to malnutrition and corticosteroid use. As the IBD improves and better nutritional status is maintained then the fatty infiltration may improve and be reversible.
You May Like: Ulcerative Colitis And Back Pain
You May Like: Skin Graft Diabetic Foot Ulcer
How Do We Diagnose Ulcerative Colitis
The Digestive Health Center at Stanford Health Care delivers expert diagnosis for all forms of inflammatory bowel disease, including ulcerative colitis. Part of what makes Stanford different is our expertise in measuring the degree of intestinal injury for each patient. This helps us understand the severity of your condition and how best to treat it.
How Can I Tell If I Have Ulcerative Colitis Or Crohns Disease
Its important that you, your healthcare provider, and a GI specialist work together closely to figure out whats causing your symptoms. This is especially important since the symptoms of Crohns disease and ulcerative colitis can be similar. Your providers may check blood work and a stool sample. To get an accurate diagnosis, your GI specialist may do a colonoscopy, where a camera is pushed into the colon. Your provider will look at the inside of the colon and take tissue samples, which are important for making the right diagnosis. Your providers might get a CT scan or an MRI of your abdomen to check for complications related to your condition.
Also Check: Home Remedies For Stomach Ulcers During Pregnancy
You May Like: Medications Used To Treat Ulcerative Colitis
Liver Conditions Linked To Ulcerative Colitis
Thereâs more than just proximity between your colon and your liver. Find out about ulcerative colitis and liver disease risks.
Yaroslav Danylchenko/Stocksy Everyday Health
Liver disease can be a complication of inflammatory bowel disease , such as ulcerative colitis or Crohns disease. The liver, which processes the food you ingest, can develop inflammation if IBD isnt treated appropriately. Unfortunately, some drugs used to treat IBD may also damage the liver.
According to a study published in 2019 by the American Gastroenterological Association, the prevalence of nonalcoholic liver diseases in patients with UC was more than double that of the general population. Considering the increased risk, it makes sense to take precautions. Laura Raffals, MD, a gastroenterologist at the Mayo Clinic in Rochester, Minnesota, recommends that people with UC have their liver enzymes checked annually. Its also wise to be aware of the common symptoms of liver disease so you can address the problem before it gets worse. According to the Crohns & Colitis Foundation, these symptoms include the following:
- Fatigue or low energy
- Fluid retention
Here are five conditions related to the liver or ducts that transport bile that may develop alongside ulcerative colitis.
Also Check: Best Treatment For Diabetic Foot Ulcer
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Also Check: Can Ulcerative Colitis Cause Urinary Problems
Daisys Story: Blood Tests
My symptoms worsened as I went through various tests to work out their cause. One of the first tests was a blood test, which doctors ordered when they believed my symptoms were happening due to a parasite. When the results came back, the doctors told me I had clear signs of inflammation.
I began taking some medications to ease my symptoms, and after these blood test results came back, the doctors referred me for further tests.
Serum Liver Enzyme Concentrations In Chronic Intestinal Disorders
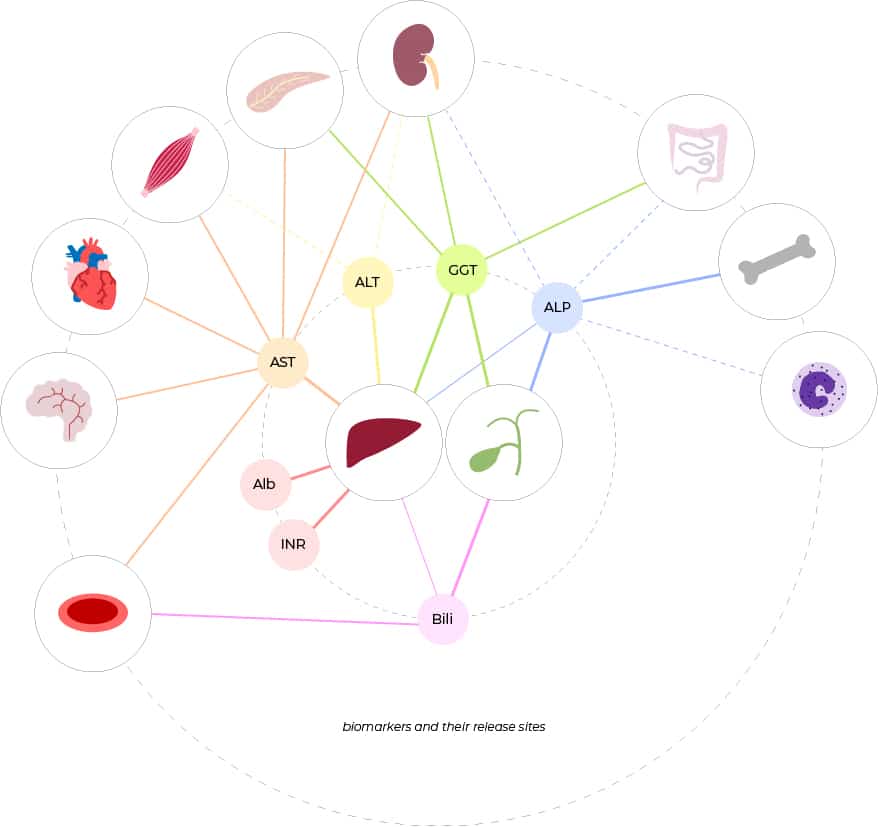
Mean alanine aminotransferase and aspartate aminotransferase concentrations in the CeD cohort were significantly higher than in controls . Accordingly, CeD participants more frequently displayed elevated AST/ALT values than controls . While the CD or UC cohorts were also more likely to have AST elevations above the upper limit of normal than controls , the corresponding odds ratios were substantially lower . In contrast, participants with IBD showed significantly higher gamma-glutamyl transferase concentrations and more often had elevated GGT than controls . Notably, all cohorts with intestinal disorders including CeD, CD, and UC displayed significantly higher alkaline phosphatase concentrations than controls and more often had increased ALP concentrations . In the vast majority, only mild elevations of AST/ALT/ALP were seen , whereas moderately elevated GGT levels were detected in 46% of all individuals and were more common in the UC/CD cohorts . While the number of patients with elevated total serum bilirubin was comparable in all groups, serum albumin concentrations were significantly lower in all disease cohorts with lowest concentrations seen in the CD cohort. .
Figure 1
Read Also: What Does Ulcerative Colitis Affect
Growth And Development Problems For Children
You can get ulcerative colitis at any age, but its more common among 15- to 30-year-olds. A child with UC may:
- Red or discolored
Continued
Talk to your doctor right away if youre worried that you might have DVT. Its possible for a deep-vein blood clot to break loose and get stuck in a lung artery. If that happens, its an emergency called a pulmonary embolism . You could have symptoms like shortness of breath, sharp chest pain, and a cough with or without blood. Call 911 if you have these signs.
Doctors can treat DVT and pulmonary embolisms with medications, a filter through a vein that removes the clot, or surgery.
You could be more likely to get DVT or PE if you:
- Have ulcerative colitis that flares often or affects a large amount of your colon.
- Get surgery for severe ulcerative colitis.
Some studies also link certain ulcerative colitis meds, like steroids or tofacitinib, to DVT and PE.
What Causes Autoimmune Hepatitis
Experts dont know what causes autoimmune hepatitis, but it is more likely to show up in people with other autoimmune conditions, including:
- Fluid buildup in the belly
- Rectal bleeding or vomiting blood
The symptoms of autoimmune hepatitis may look like other health problems. Always see your healthcare provider for a diagnosis.
Read Also: Is Oatmeal Good For Ulcerative Colitis
Health And Medical Information
This Blog is designed to be a resource center. Complete information on topics including Healthy Life Style, Beauty Tips, Fashion Tips, Yoga, Naturopathy, Ayurvedic & Medical Knowledge, Herbal Remedies, Ayurvedic Herbs, Natural Cosmetics, Rejuvenation Therapies, Aroma Therapy, Herbal Diet, Meditation, Yoga Styles, Men’s Health & Women’s Health Topics, Health Calculators,Entertainment and more..
Complications Of Ulcerative Colitis And How To Avoid Them
Learn how to identify and avoid potentially life-threatening complications of ulcerative colitis.
If you have an inflammatory bowel disease like ulcerative colitis , a gastroenterologist can prescribe medication and create a treatment plan for the inflammation and sores, called ulcers, that occur in the lining of the large intestine and rectum. But this autoimmune disorder is often associated with complications in other parts of the body that should be addressed as well.
Extraintestinal complications those that exist outside the intestines can even overshadow symptoms in your bowels, making UC tricky to diagnose. They are also highly prevalent, occurring in nearly half of UC patients and appearing more often in women, according to a review published in May 2019 in Current Gastroenterology Reports. While it remains unclear why UC complications can arise beyond the intestines, the review noted that genetic predisposition, irregular immune response, and changes to the gut microbiome are some common contributing factors.
âItâs easy to forget that ulcerative colitis is not just a disease of the intestines but a systemic or body-wide disorder of the immune system,â says Jessica Philpott, MD, PhD, a gastroenterologist at Cleveland Clinic in Ohio.
Below are five conditions commonly linked to ulcerative colitis, along with some treatment options.
Also Check: Probiotics Good For Ulcerative Colitis
Recommended Reading: What Foods To Eat If You Have An Ulcer
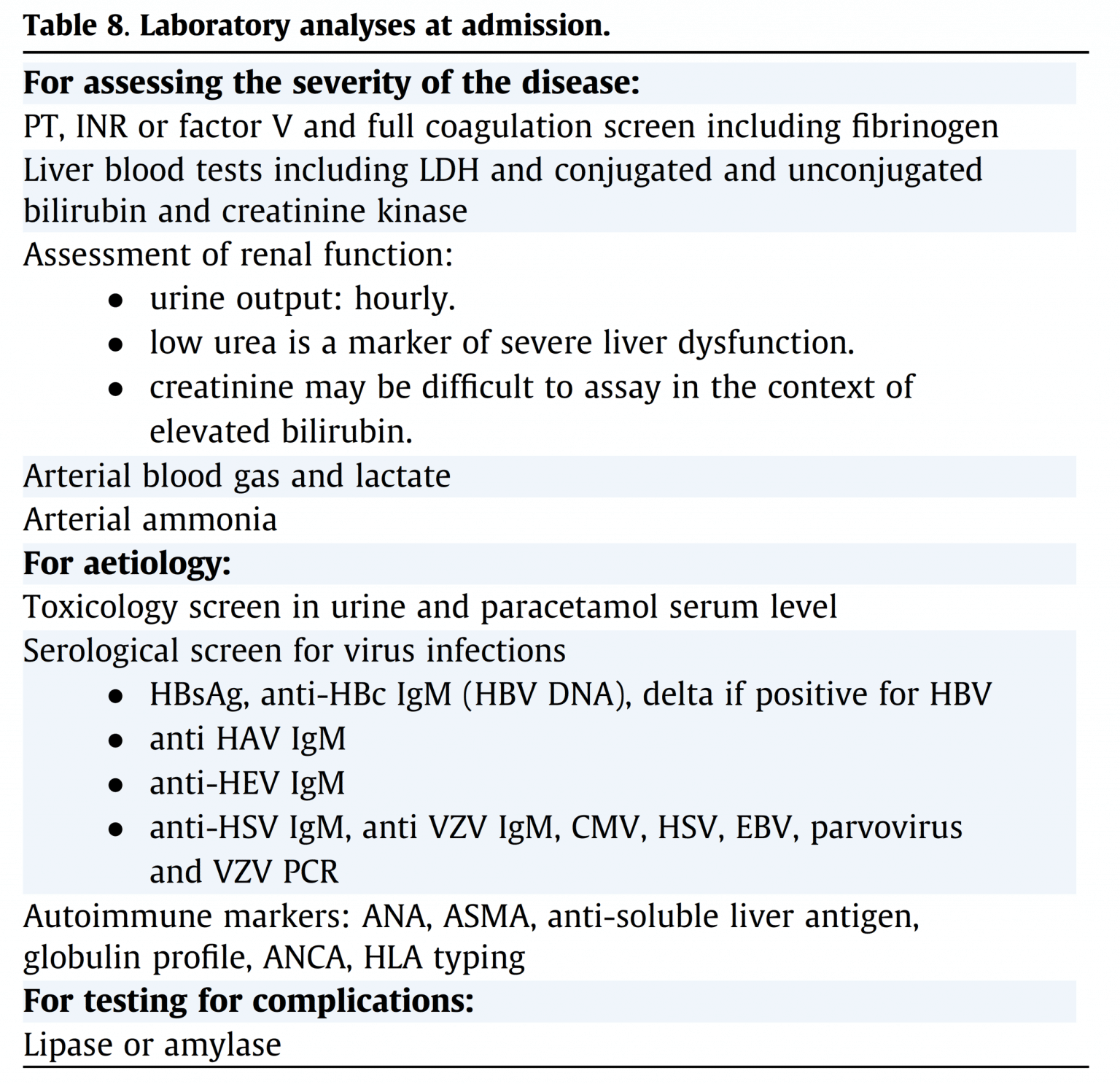
How Is Autoimmune Hepatitis Diagnosed
Your healthcare provider will look at your health history and give you a physical exam.
Some lab blood tests used to diagnose autoimmune hepatitis include:
- Liver function tests. These check for inflammation or damage to your liver.
- Complete blood count or CBC. Looks at the number and types of cells in your blood.
- Coagulation panel. This test looks at how well the clotting proteins are working.
- Electrolyte panel. Checks to see if you have an electrolyte imbalance.
- Autoimmune antibodies. These are used to see if you have autoimmune hepatitis or another liver disease with similar symptoms.
- Other liver tests. These are done to check for other possible types of liver disease.
You may also have imaging tests such as:
Similar Articles Being Viewed By Others
Carousel with three slides shown at a time. Use the Previous and Next buttons to navigate three slides at a time, or the slide dot buttons at the end to jump three slides at a time.
25 April 2019
Arun J. Sanyal
15 January 2018
Lana C. Pinto, Dimitris V. Rados, Jorge L. Gross
21 March 2018
In Cheol Hwang, Jooyoung Chang, Sang Min Park
14 September 2018
Christos Triantos, Ioanna Aggeletopoulou, Konstantinos Thomopoulos
volume 11, Article number: 19954
Recommended Reading: Medicine For Diabetic Foot Ulcer
Extraintestinal Organ Systems Involved With Ibd
- Endocrine and Metabolic
Approximately 36% of patients who have been diagnosed with IBD have at least one associated extraintestinal manifestation. Some of the most common extraintestinal manifestations of IBD are related to active colitis and may involve the joints, the skin, the eyes, or the inside lining of the mouth. Others that are more commonly associated with small bowel dysfunction are gallstones, kidney stones, and obstruction of the urinary tract. This article will focus only on those extraintestinal manifestations that are associated with IBD and liver disease.
What Ulcerative Colitis Treatments Should You Consider After A Diagnosis
We could write a whole article on treatments for ulcerative colitis , but know this: The majority of patients can get control of their disease with medical therapy, Dr. East says. About 15 out of 100 patients may need surgery by 10 years after diagnosis, but this varies by extent of inflammation. New drugs are making the need for surgery less common.
Biologics, which are powerful medications made from living things that are delivered via injection, are very effective at controlling the inflammation associated with ulcerative colitis, and are based on your own antibodies, Dr. East explains. They have the ability to bind to specific molecules involved in triggering inflammation, and have revolutionized treatment of UC and other autoimmune disorders, he says.
Dr. East says lots of patients see a change for the better in two to four weeks. In some cases, a fast-acting drugsteroids, for examplemay be used to get control quickly and then a slow-acting maintenance therapy takes over. Maintenance medications are considered safer than steroids for longer term use.
For some people, the internal J-pouch just wont work. Surgeons create an opening called a stoma in the abdomen, and an external pouch does the waste collection.
Read Also: What Are The Side Effects Of An Ulcer
Causes Of Cirrhosis Of The Liver
In people with IBD, cirrhosis could be caused by autoimmune hepatitis or primary biliary cirrhosis. Autoimmune hepatitis is associated with a dysfunctional immune system. Primary biliary cirrhosis is an inflammation of the bile ducts that can inhibit bile from leaving the liver and going to the small intestine. When the bile gets backed up it can cause further damage to liver tissues. Primary sclerosing cholangitis, which is largely associated with ulcerative colitis, can also overlap with autoimmune hepatitis .
Also Check: Can Ulcerative Colitis Cause Eye Problems
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Read Also: How To Treat Stage 4 Pressure Ulcer
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
When To Get Help For Liver Pain
Symptoms such as pain in the upper right side of the abdomen, itching, jaundice, and fever could be an alert for a potential liver complication, says David Bernstein, MD, chief of hepatology at Northwell Health in Manhasset, New York. If you experience these issues, contact your doctor for an evaluation. Blood tests can usually confirm liver disease, but additional testing using an ultrasound, X-ray, or liver biopsy may be necessary to make a specific diagnosis. Treatment may include vitamin supplementation and modifying your diet to prevent nutrient deficiencies.
Additional reporting by Agata Blaszczak-Boxe.
Read Also: Good Things To Eat With Ulcerative Colitis
Is Liver Disease Permanent
Liver damage isn’t reversible, but when liver disease is present, further damage can be prevented. Getting proper treatment, eating a healthy diet, and avoiding alcoholic beverages are all important to halting the progression of liver disease. Any complications from the liver disease must also be treated, to avoid further damage to other body systems from toxins building up in the brain and the blood. Medications might also be used to manage portal hypertensions and varices.
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Also Check: Fasting To Heal Ulcerative Colitis
Also Check: Foods Ok To Eat With Ulcer
How Liver Damage Is Diagnosed With Crohns Disease
If routine blood tests show abnormalities in your liver, your doctor may do additional screenings to find out if the liver problems are related to your Crohnâs disease or not. Knowing the cause of your liver problems can help guide your future medications and treatment.
Your doctor may ask for these additional tests:
- Endoscopic examination of the bile ducts
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Also Check: Drinking Alcohol With Ulcerative Colitis
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.