Deal With Iron Deficiencies Too
UCs painful, even gut-wrenching symptoms dont always make it fun to eat. And, people with this chronic condition may lose blood in their stool, as well as absorb dietary iron poorly due to inflammation, according to the Cleveland Clinic. Additionally, foods rich in iron, like red meat, often trigger flareups. Together, this can cause anemia, a condition characterized by a low red blood cell count. Its a common issue with the UC communityand must be controlled to battle fatigue. If you have UC and super-low energy, talk to your doctor about iron supplements.
More Tips To Ease Ulcerative Colitis Symptoms
The best way to shorten a flare, of course, is to get treated by your doctor. But there are steps you can take at home too.
When you have a flare, try to follow a low-residue diet for several weeks, Damas says. The goal is to let the colon rest by avoiding fiber. That means staying away from seeds, nuts, fresh fruit, dried fruit, raw vegetables, whole grain bread and cereal, and tough meat.
Were learning more now about the influence that diet can have on control of inflammation, Damas notes. When patients are having an acute flare, its important in the short term to have a low-fiber diet. Many times, for a short period of time, until the flare-up is controlled, we recommend whats called a low FODMAP diet. However, this diet is not recommended long term, because it has no impact on inflammation itself and only on control of symptoms.
Indeed, once youre in remission, Damas says your doctor will likely recommend reintroducing fruits and vegetables as tolerated. Its better to cook vegetables without the skin and consume no more than 2 cups of milk a day.
If youre lactose intolerant, be sure you choose lactose-free dairy products. Its also a good idea to cut down on fat during this time to prevent bulky stools. Avoid other potential triggers, too, such as spicy foods.
Additionally, we recommend patients avoid eating processed foods, as well as those high in fat and animal protein, as these have been associated with inflammation in some studies, Damas says.
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Don’t Miss: What Does A Skin Ulcer Look Like
Genetics Can Cause Ulcerative Colitis
Genes are also supposed to play a major role as almost 25 percent of the cases of ulcerative colitis have been found to be individuals having family history for ulcerative colitis. In addition, some of the ethnic groups have been seen to be more affected by this issue.
There are certain genes, which have been recognized by researchers related to the cause of ulcerative colitis, and these genes are closely related to the immune system.
What Are Ulcerative Colitis Medications
Since ulcerative colitis cannot be cured by medication, the goals of treatment with medication are to 1) induce remissions, 2) maintain remissions, 3) minimize side effects of treatment, 4) improve the quality of life, and 5) minimize risk of cancer. Treatment of ulcerative colitis with medications is similar, though not always identical, to treatment of Crohn’s disease.
Medications for treating ulcerative colitis include 1) anti-inflammatory agents such as 5-ASA compounds, systemic corticosteroids, topical corticosteroids, and 2) immunomodulators.
Anti-inflammatory medications that decrease intestinal inflammation are analogous to arthritis medications that decrease joint inflammation . The anti-inflammatory medications that are used in the treatment of ulcerative colitis are:
- Topical 5-ASA compounds such as sulfasalazine , olsalazine , and mesalamine that need direct contact with the inflamed tissue in order to be effective.
- Systemic anti-inflammatory medications such as corticosteroids that decrease inflammation throughout the body without direct contact with the inflamed tissue. Systemic corticosteroids have predictable side effects with long term use.
It has long been observed that the risk of ulcerative colitis appears to be higher in nonsmokers and in ex-smokers. In certain circumstances, patients improve when treated with nicotine.
Recommended Reading: Venous Stasis Ulcer Right Lower Leg Icd 10
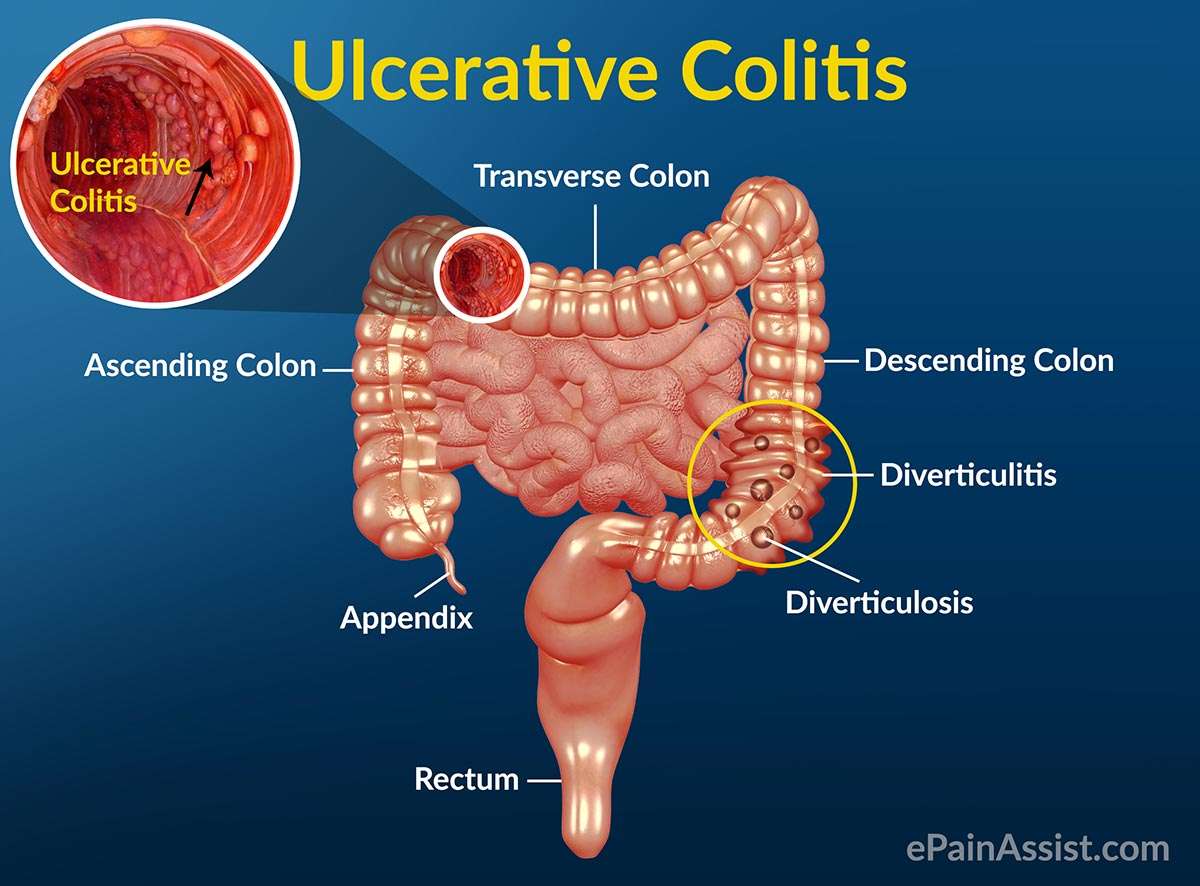
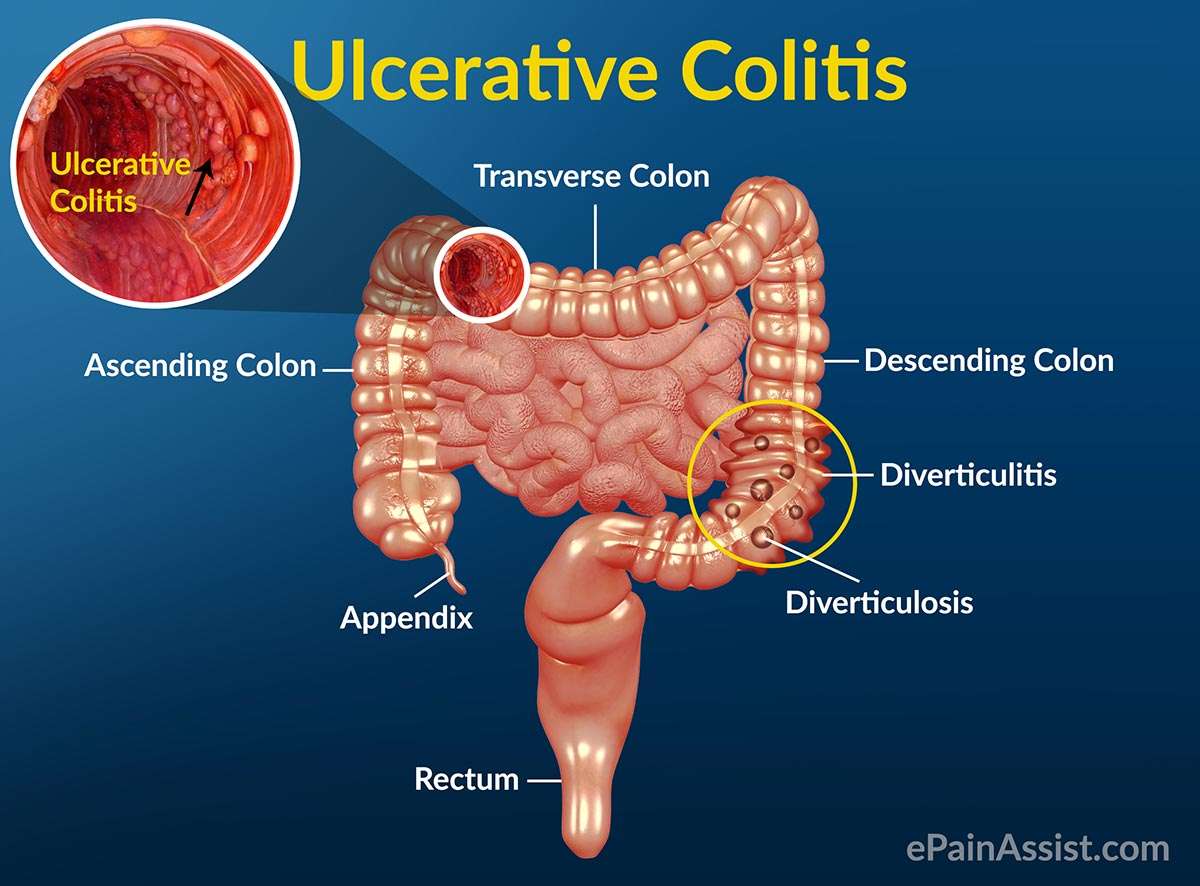
What Is Ulcerative Colitis
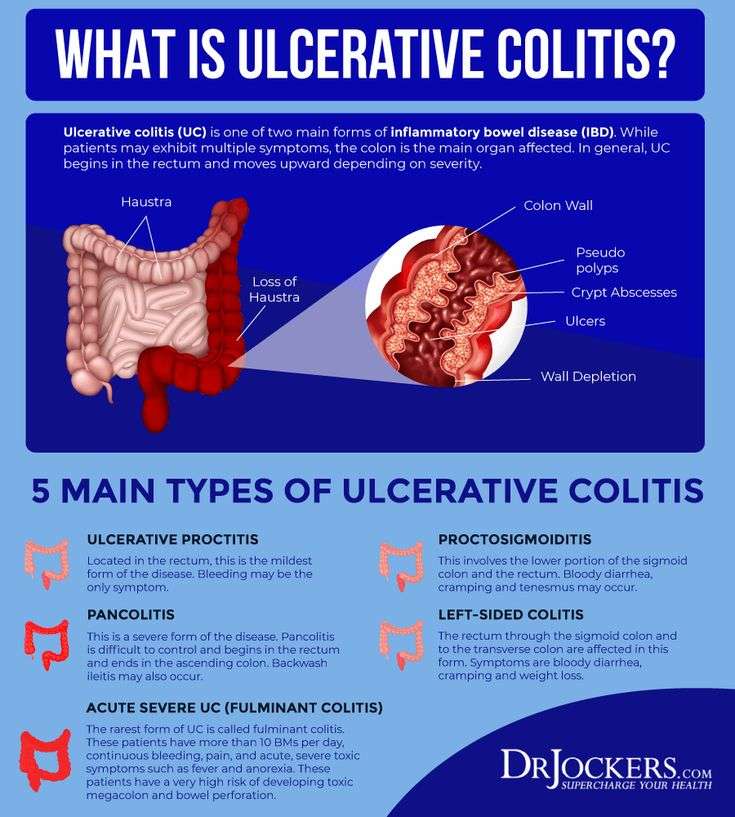
Ulcerative colitis causes irritation and ulcers in the large intestine . It belongs to a group of conditions called inflammatory bowel disease . It often causes diarrhea with blood, cramping and urgency. Sometimes these symptoms can wake a person up at night to go to the bathroom as well.
The inflammation in ulcerative colitis usually starts in the rectum, which is close to the anus . The inflammation can spread and affect a portion of, or the entire colon. When the inflammation occurs in the rectum and lower part of the colon it is called ulcerative proctitis. If the entire colon is affected it is called pancolitis. If only the left side of the colon is affected it is called limited or distal colitis.
The severity of UC depends on the amount of inflammation and the location. Everyone is a little different. You could have severe inflammation in the rectum or very mild inflammation in the entire colon .
If you have ulcerative colitis, you may notice a pattern of flare-ups , when symptoms are worse. During times of remission, you might have little to no symptoms. The goal with therapy is to remain in remission as long as possible .
What Causes Uc Cramping
Common causes of UC cramping, according to Ha, are flare-ups, lack of sufficient control of the condition , eating foods that are high in saturated fat or sugar, and adverse reactions to medication.
Cramping due to gas and bloating can also be caused by irritable bowel syndrome , a separate condition from ulcerative colitis that can cause symptoms even when your disease is in remission. IBS can be linked to certain gas-causing foods, including dairy if youre lactose intolerant.
Also Check: What Foods Should You Eat If You Have An Ulcer
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
The medication released from a suppository will travel upward and usually reach about 15 cm inside from the anus. An enema will reach farther, about 60 cm. Those with ulcerative colitis usually insert these formulations before bedtime, and this way the medication is retained as long as possible. Stool does not typically interfere with the drug, since the bowel area is typically relatively empty right before bed.
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
Recommended Reading: Natural Supplements For Ulcerative Colitis
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Don’t Miss: How Do You Cure Mouth Ulcers
Keep Up With Your Medicine
Don’t double up on doses of medication if you’re flaring. Although you really want relief, a change in your treatment can trigger flares or make them worse. Let your doctor know when you have a flare while you’re on your usual medication plan. Take medicines only as directed. The same goes for when you feel good and may be tempted to skip doses, too.
How Common Is Cramping Among Those Who Have Uc
Inflammatory bowel disease, which includes both UC and Crohns, affects about 1.6 million Americans of all ages, according to the Crohns and Colitis Foundation. More than half of those with UC experience abdominal pain.
The frequency and persistence of cramping can help determine the severity of UC, according to Faten N. Aberra, MD, MSCE, co-director of the Inflammatory Bowel Disease Center at the Joint Penn-CHOP Center and an associate professor of medicine at the Hospital of the University of Pennsylvania, in Philadelphia. Pain that comes and goes with bowel movements may indicate a moderate level of UC. Constant cramping and frequent, bloody stools, on the other hand, may indicate a more serious condition, says Dr. Aberra, such as a dilated colon.
Read Also: Ulcerated Nodular Basal Cell Carcinoma
How Is Abdominal Pain Treated
If abdominal pain is a sign of a Crohns disease or ulcerative colitis flare, the goal is to treat the underlying disease. Pain and cramps should improve within a few weeks of treatment.3 If there is no improvement, you may need further evaluation. Your provider may need to check for complications.
Pain medications can be helpful. Some health care providers recommend acetaminophen or COX-2 inhibitors instead of non-steroidal anti-inflammatory drugs .
In a high-quality study, people were randomly assigned to the COX-2 inhibitor celecoxib or fake treatment .9 There was no difference in disease flares between the 2 groups. In a different trial, people were less like to have a disease flare with acetaminophen than with an NSAID.9
An estimated 1 in 6 people with inflammatory bowel disease use opioid medications regularly for pain.5 This use of opioids is controversial. Opioids often cause problems with digestive tract function. Additionally, there is a risk of abuse.
Nevertheless, it is important for providers to recognize when there is a legitimate need for adequate pain relief.9 Patients who discuss opioid medications with their providers should not be automatically labeled as drug-seekers.
Ulcerative Colitis And Colon Cancer
Individuals with ulcerative colitis are at increased risk for colon cancer. The risk of colon cancer increases while the duration of disease and the extent of the disease in the colon increase. To prevent colon cancer, screening colonoscopy with biopsies are recommended on a regular basis in order to detect precancerous cells so that the colon can be removed surgically before cancer develops. Screening usually is begun approximately eight years after the onset of the disease, the time at which the incidence of colon cancer begins to increase.
Don’t Miss: How To Cure Tongue Ulcer
What Inflammatory Bowel Disease Pain Feels Like
Symptoms of inflammatory bowel disease can include diarrhea, blood in the stool, weight loss, and abdominal pain. The type and location of abdominal pain is different, not only between the two main forms of IBD but also within the subtypes of these diseases.
Further, pain is even more individual to each person, to the point where people with the same subtype of Crohn’s disease or ulcerative colitis may experience pain in a different way.
In fact, some people with IBD don’t have any abdominal pain at all during IBD flare-ups. In addition, abdominal pain can be related to other issues , such as appendicitis, gallstones, or gastroesophageal reflux disease .
But as abdominal pain is a common symptom of IBD, here is an overview of the types of abdominal pain that are most often experienced by people with IBD.
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Recommended Reading: Ulcerative Colitis Social Security Disability
What Are Common Non
Inflammation is not the only source of pain caused by IBD. Non-inflammatory sources of pain in the digestive tract include:1,2
- Strictures narrowing of the intestines
- Adhesions bands of scar tissue that can develop after surgery
- Small-bowel obstruction
Non-inflammatory sources of pain due to IBD that are outside the digestive tract include:1
- Kidney stones
- Gallstones
Surgery For Ulcerative Colitis
Surgery for ulcerative colitis usually involves removing the entire colon and the rectum. Removal of the colon and rectum is the only permanent cure for ulcerative colitis. This procedure also eliminates the risk of developing colon cancer. Surgery in ulcerative colitis is reserved for the following patients:
Standard surgery involves the removal of the entire colon, including the rectum. A small opening is made in the abdominal wall and the end of the small intestine is attached to the skin of the abdomen to form an ileostomy. Stool collects in a bag that is attached over the ileostomy. Recent improvements in the construction of ileostomies have allowed for continent ileostomies. A continent ileostomy is a pouch created from the intestine. The pouch serves as a reservoir similar to a rectum, and is emptied on a regular basis with a small tube. Patients with continent ileostomies do not need to wear collecting bags.
Recommended Reading: Indian Diet For Ulcerative Colitis
Five Tips For Dealing With Ulcerative Colitis Pain
There are ways to combat the pain that comes along with ulcerative colitis flare-ups. However, it is always best to get treatment from a doctor as they are most likely to efficiently and safely resolve your symptoms.
Here are five strategies you can use to help relieve symptoms and avoid a flare-up in the first place.
What Pain Relief Medicines Are Used In Inflammatory Bowel Disease
There are a variety of pain relief medicines available which can help to control pain in Crohns disease and ulcerative colitis.
Paracetamol
Paracetamol is a commonly used over-the-counter painkiller you can buy without a prescription. It can be used to help with mild to moderate pain, and can also help to control a high temperature. Paracetamol can be used by adults and children and is available in a variety of forms, including:
- Tablets, capsules and caplets
- Soluble tablets
- Oral suspension
- Suppositories
Paracetamol works by blocking the production of chemicals in your body called prostaglandins, making your body less aware of any pain. It also reduces your temperature by acting on the part of your brain responsible for controlling it.
Paracetamol is often combined with other medicines, including other types of painkillers. Always check any additional medicines are also safe for you to use.
It is generally considered safe to take paracetamol if you have inflammatory bowel disease, however if you need to take paracetamol for longer than three days, or have a new pain, you should speak to your IBD team.
Two paracetamol tablets every four hours, up to four times a day is considered a safe dose for adults. Side effects are uncommon with paracetamol.
You should read the patient information leaflet in your medicine packet to check if paracetamol is suitable for you. Do not take more than the maximum dose in a 24 hour period as an overdose of paracetamol can be very dangerous.
Don’t Miss: How Do They Check For Ulcers