Finding The Right Uc Diet For You
For those living with ulcerative colitis, choosing the right foods to eat may feel overwhelming. If you are worried you may not be getting enough of one or more nutrients, speak with your gastroenterologist. They may test your blood for nutrient levels to find out whether you are deficient. If you are deficient in any nutrient, your doctor may recommend a safe and effective dietary supplement.
You can also request a referral to a registered dietitian who can work with you to get the most out of the nutrients in the foods youre able to eat. Working with a registered dietitian or nutritionist can also help you navigate life events, such as parties, dining out, vacations, and more. Understanding what triggers your flare-ups life stress or specific foods is important information that a food journal can help you decipher.
The good news is that for people with UC who establish a healthy and safe diet plan, sticking to it often helps them feel better and manage symptoms. Feeling pretty good today, wrote one MyCrohnsAndColitisTeam member. Ive gone lactose- and gluten-free, and symptoms have reduced a lot. Also gave up caffeine. Living on avocado!
You are not alone in your path to finding a safe and healthy diet with ulcerative colitis. When you join MyCrohnsAndColitisTeam, you gain a supportive community of more than 138,000 people living with IBD.
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient. Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAPstands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
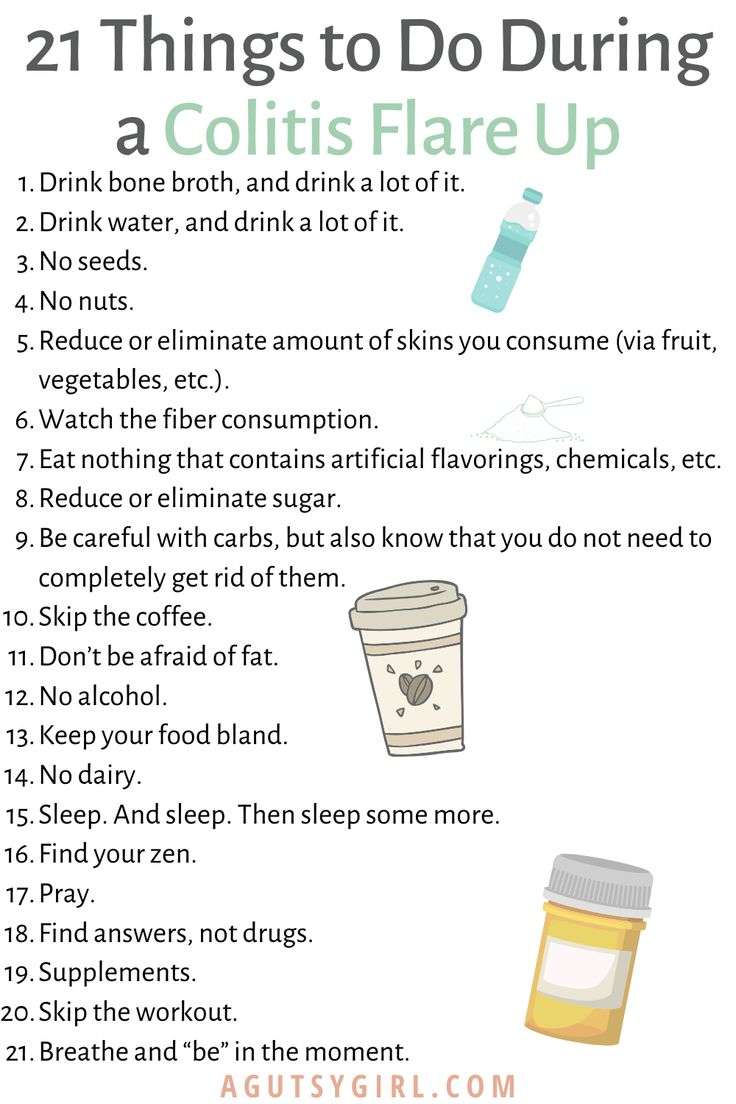
Tips For Managing Ulcerative Colitis Symptoms
- Consult your healthcare provider or dietitian before making any changes to your diet
- Eat a well-balanced nutrient rich diet
- Eat more frequently. Eat five to six smaller meals over the course of a day
- Stay hydrated by drinking water and fluids with salt like broth, tomato juice or rehydration solutions
- Drink slowly and avoid using a straw because these may cause gas due to taking in air
- Use a food diary to record the foods you eat and how these impact your symptoms
- Avoid your specific trigger foods
- Use simple cooking methods boil, steam, grill, poach, broil or saute
Recommended Reading: What To Drink With Stomach Ulcer
General Guidelines When Ulcerative Colitis Is In Remission
Some members of MyCrohnsAndColitisTeam find they can eat a wider variety of foods safely during remission periods when ulcerative colitis is not as active and symptoms are absent or mild. Still, every individual is different, and purportedly beneficial foods may trigger symptoms. Trial and tracking is the only way to know for sure.
If it is safe for you, these guidelines may help you stay your healthiest during remission:
- Get 25 grams to 35 grams of fiber per day to promote bowel regularity and reduce inflammation.
- Consume plenty of lean meats, which are a good source of B vitamins. Include fatty fish, tofu, and nut and seed butters.
- Include probiotic foods such as yogurt, tempeh, kefir, kimchi, miso, and sauerkraut.
While some members find kefir too sour for their liking, others report experiencing benefits from trying the fermented drink. Kefir has been helping me over the past week, wrote one. Been trying kefir the past few days. Will keep you posted. So far less pain, said another.
Do Grapes Trigger Ibs
Fruits contain the sugar fructose, which can cause issues for IBS sufferers. Fructose is particularly high in apples and pears, and somewhat high in watermelon, stone fruits, concentrated fruit, dried fruit and fruit juice. Fruits with lower levels of fructose include bananas, citrus, grapes and berries.
Don’t Miss: Can Stress Give You An Ulcer
The Best Foods To Eat And Avoid For Inflammatory Bowel Disease
Inflammatory bowel disease is a treatable, yet chronic and lifelong condition. IBD is a broad term that refers to the inflammation of the gastrointestinal tract and includes specific conditions such as ulcerative colitis and Crohns disease.
No plan has been proven to prevent or control IBD. But managing your diet can help manage your disease during flares and periods of remission. Be sure to talk to your physician or a registered dietitian about your nutrition needs and managing IBD.
Here are diet recommendations for managing IBD flares and remissions from UH Outpatient Nutrition Services.
What Types Of Diets Should I Consider
Both experts agree that everyones ulcerative colitis symptoms, triggers, and treatments are different, but there are certain eating styles that may be worth considering.
Talk with a health professional about whether one of these diets could be beneficial for you.
FODMAP is an acronym for types of carbohydrates that are poorly absorbed in the small intestine, specifically:
- Fermentable
- Monosaccharides
- Polyols
Because of their poor digestion, FODMAPs can cause gastrointestinal issues in some people7. Research suggests an improvement in IBD symptoms in some patients who follow a low FODMAP diet, but there is no evidence of improved inflammation8.
Some health care providers may counsel their patients to try a FODMAP elimination diet during an UC flare, followed by reintroduction of FODMAP foods once in remission.
What does that mean for actually eating food? Well, you may want to try swapping high-FODMAPs like cauliflower, mushrooms, dried fruit, cows milk, and legumes for low-FODAMPs like eggplant, carrots, grapes, potatoes, eggs, quinoa, and tofu.
The Mediterranean diet is widely considered to be one of the worlds healthiest eating patterns for people with and without chronic conditions.
While you may have heard of the paleo diet, the autoimmune protocol diet , which is considered to be similar to the paleo diet, may have some benefits for people with IBD.
Although some very small studies see the benefits of this style of eating, more research is needed10.
Also Check: What Is An Ulcer Diet
Back Up: What Is Ulcerative Colitis Exactly
Ulcerative colitis is a type of inflammatory bowel disease that causes ulcers and sores in the lower quarter to third of your digestive tract. Typically, these ulcers are found in your rectum or in the inner lining of your lower intestine . This can cause bloody diarrhea, the most common symptom of ulcerative colitis, but you might also experience things like abdominal cramping, constipation, and a general sense of fatigue. Weight loss and a loss of appetite can also crop up, per the U.S. National Library of Medicine.
Diana Whitehead, M.D., director of the Inflammatory Bowel Disease Center at the Greater Baltimore Medical Center, explains that though ulcerative colitis has a strong genetic component, symptoms are often set off by a triggering event that activates inflammation in the lower intestine. Basically, your immune system is not doing what it should do, which is to protect you, but its gone kind of into overdrive, Dr. Whitehead says. In other words, even though the exact causes of ulcerative colitis arent fully understood, experts consider it to be an autoimmune condition thats set off by this overreaction in the gut.
Vegetable And Fruit Juices
Vegetable and fruit juices are low in fiber and high in some vitamins and minerals. Manufacturers also fortify some juices.
It is best to avoid sugar during a CD flare-up, but a daily glass of diluted fruit juice that contains no added sugar can help boost a persons nutrient intake.
Vitamin C from fruit juice can also help the gut absorb iron.
Foods that are high in fat can worsen or prolong symptoms during a CD flare-up.
However, protein and other nutrients from animal products can help prevent malnutrition.
Skinless chicken and turkey are good examples of lean meats. If a person is purchasing red meat, such as pork, they should select the leanest cut available and trim any excess visible fat.
Recommended Reading: Foods To Treat Ulcerative Colitis
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
So much research still needs to be done to find the ideal combination of foods that will keep IBD in remission, but you can work with a gastroenterologist or registered dietitian to find what works for you.
That may require a lot of trial and error, so be patient with yourself.
Some of the diets experts recommend are:
Recommended Reading: Hind Gut Ulcers In Horses Symptoms
What Foods Should I Eat During An Ulcerative Colitis Flare
When you are experiencing an ulcerative colitis flare-up, experts suggest you stick to foods that are less likely to aggravate your gut. Some of these include:
- White rice, bread, and pasta
- Crackers and cereals made with refined white flour
- Cooked veggies without the skin
- Tender, soft meats and fish
- Olive and coconut oil
- Eggs
- Lots and lots of fluids, since an ulcerative colitis flare-up can lead to diarrhea and thus dehydration
These foods have been found to be easily digestible in some ulcerative colitis patients, but be cautious when adding them to your diet since they can be triggers in other patients:
- Squash
- Probiotics
- Plain instant oatmeal
When you are experiencing an ulcerative colitis flare-up, experts suggest you stick to foods that are less likely to aggravate your gut.
Also Check: What Is The Medication For Ulcerative Colitis
What Is Ulcerative Colitis
Ulcerative colitis is a chronic type of inflammatory bowel disease , like Crohns disease and microscopic colitis that affects the colon .
Recent studies estimate that IBD affects 2 million people worldwide .
Ulcerative colitis causes inflammation and sores in the inner lining of the colon. Inflammation often begins in the rectum, but it can spread throughout the large intestine.
Summary: Ulcerative colitis is a type of inflammatory bowel disease that causes inflammation and sores in the colon.
Nutrition Tips For Inflammatory Bowel Disease
Inflammatory Bowel Disease is a term used for two specific and separate diseases: Crohn’s disease and ulcerative colitis. Nutritional recommendations are different for each disease and for each individual patient. It is important to discuss the treatments that are right for you with a registered dietitian and with your doctor.
Read Also: Foam Boots For Pressure Ulcers
Cooked And Peeled Vegetables
Many vegetables are high in fiber, but as with fruit, peeling them removes a layer of insoluble fiber.
Some vegetables do not need peeling, such as asparagus tips and mushrooms, but it can help to remove the skins of potatoes, carrots, and squash.
Cooking vegetables also makes them easier to digest, and it can reduce the fiber contents.
However, avoid roasting or frying vegetables in oil or butter, because fats can irritate the digestive system and worsen symptoms of Crohns. Try boiling or steaming them instead.
List Of Foods To Eat To Keep Colitis From Flaring Up
Colitis is an inflammatory bowel disease. There are several types of colitis, depending on the location of the inflammation. Symptoms vary but commonly include abdominal cramps, bloating, constipation and diarrhea. There’s really no nutritional therapy for colitis, nor is there a cure. But learning to strike a balance between getting the nutrients you need and avoiding the foods that seem to trigger your symptoms can help you manage the condition.
Video of the Day
You May Like: Dr Reckeweg Medicine For Ulcerative Colitis
Can Elimination Diets Cure It
Up to 60% of IBD patients have tried an elimination diet to relieve ulcerative colitis symptoms .
Unfortunately, the only known cure is total surgical removal of the colon and rectum .
There is no scientific proof that any diet can cause remission on its own. However, limited evidence suggests that certain diets can greatly improve comfort and quality of life.
The impact of diet on inflammatory bowel disease. Click to enlarge. Image .
It Can Be Challenging To Differentiate Between Crohn’s And Uc
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
|
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohn’s Disease here.
You May Like: What Over The Counter Medicine For Ulcers
Should You Take Nutritional Supplements With Uc
In some cases, you may not be able to get all your nutritional needs directly from food your intestines just cant do their best nutrient-absorbing job when its dealing with ulceration. Thats where supplements come in. Again, its important to understand that theres not a set list of supplements that everyone with UC should takeit really varies from person to person.
Your GI or registered dietitian will recommend supplements based on your specific situation after looking at your symptoms and test results. And always get the green light from your doctor before adding a supplement to your routinesome may actually contain sugar alcohols, lactose, and preservatives that can actually aggravate your symptoms.
That said, here are some supplements that are commonly recommended for people with UCdont forget to take them on a full stomach, or else they could irritate your GI tract:
Keep in mind, this isnt an exhaustive list of possibilitiesyour doctor may recommend other vitamin or mineral supplements, including potentially a multivitamin, depending on your specific nutritional needs.
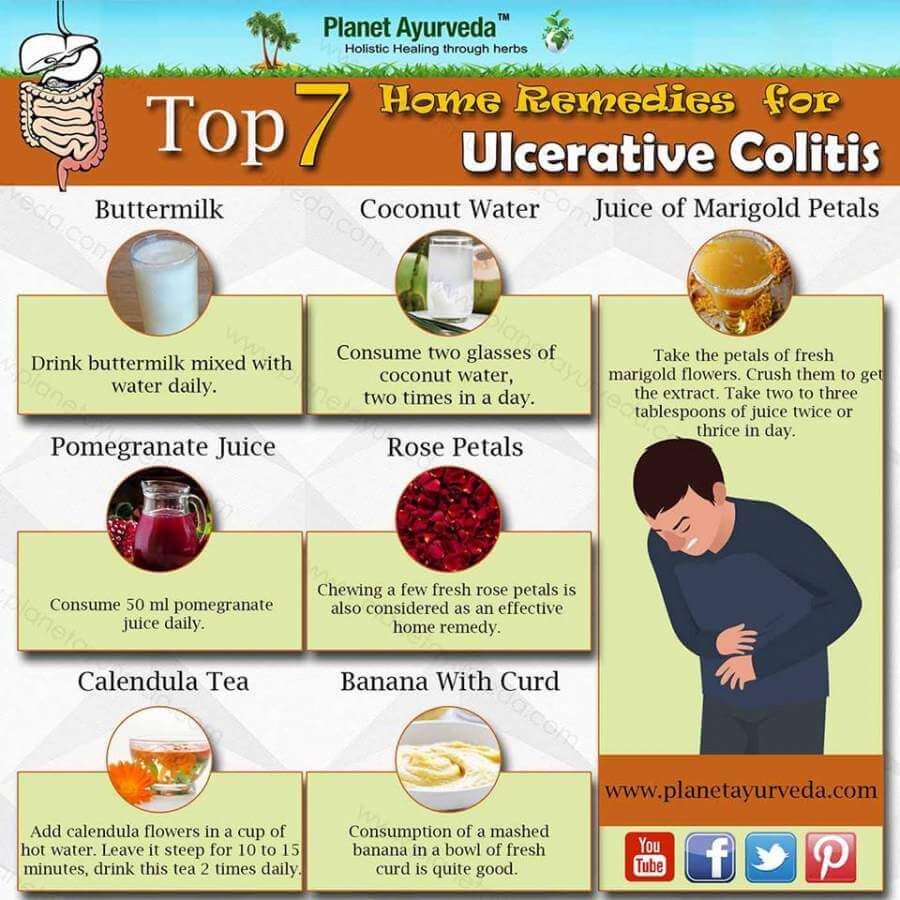
Herbal Remedies And Supplements
There are lots of supplements that claim to treat Crohns and Colitis. But there isnt enough evidence to recommend any herbal remedies or supplements. This is because its difficult to know whether the supplement is directly affecting a persons Crohns or Colitis or whether something else is causing a change in symptoms. Also, everyone is different so what helps one person may not help another.Some people find that some herbal remedies, such as aloe vera or curcumin , help them manage their symptoms when they use them together with their prescribed medicines. There have been reports of cannabidiol , an ingredient in cannabis, helping with symptoms like diarrhoea, pain and loss of appetite. But we dont know enough about how it works or how much is a safe amount to take. It isnt currently recommended and isnt available on prescription for people with Crohns or Colitis.There have been claims in the media about the benefits of kefir a fermented milk drink that contains probiotics. But there isnt any medical evidence to show that it helps people with Crohns or Colitis.If you want to take herbal remedies, its important to speak to your IBD team or dietitian first. Dont stop taking your prescribed medicine without talking to your IBD team, even if your symptoms improve.
I think it is so important to remember that the relationship with food and IBD is so different for everyone!
Tom
Read Also: Can You Donate Blood If You Have Ulcerative Colitis
Adding Foods Back After A Flare
Just because a food was eliminated during a flare, doesnt mean you have to give it up entirely. Here are some tips for adding foods back after a flare:
- Eat small, frequent meals every three to four hours.
- Take small bites and chew well.
- Slowly liberalize your diet, adding one or two items at a time. The foods to start with include cooked vegetables, peeled fruits, mild cheese and yogurt, oatmeal and barley, tofu and soymilk, and hummus.
- Raw and cruciferous vegetables should be added back last.
- Slow down and relax at meal time.