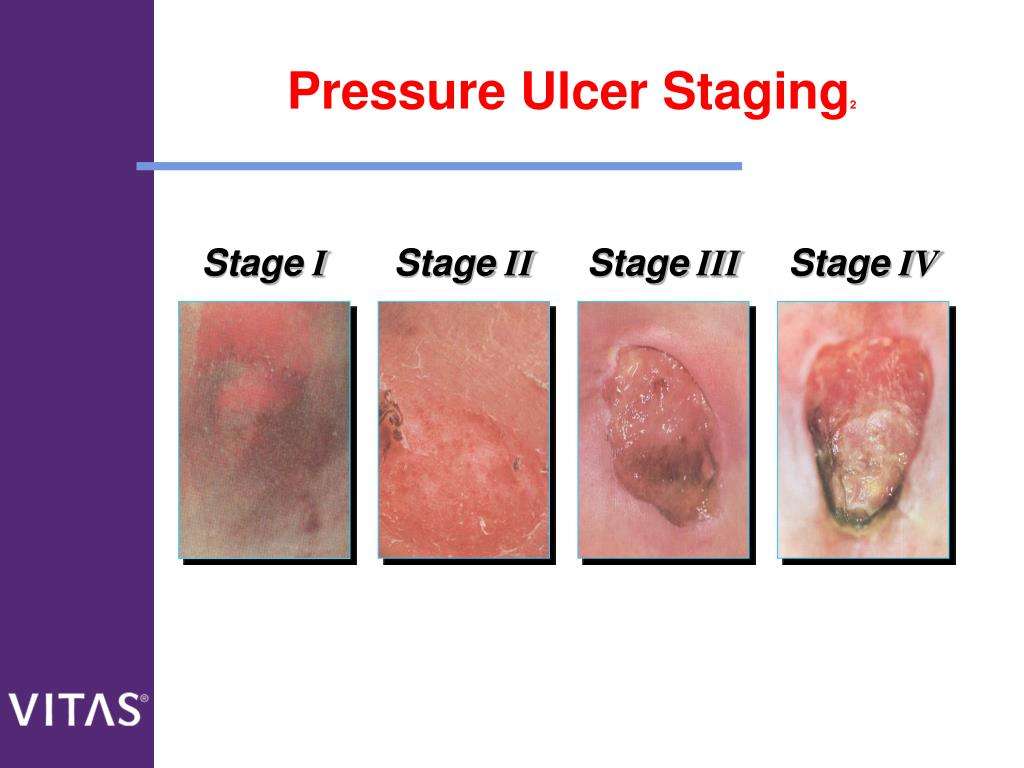
Stages Of Pressure Ulcer
Pressure ulcer wound is a concentrated area where the soft tissues of the body is damaged due to the compression of a bony surface and an external surface for a prolonged period of time.
Source: HealthSaver
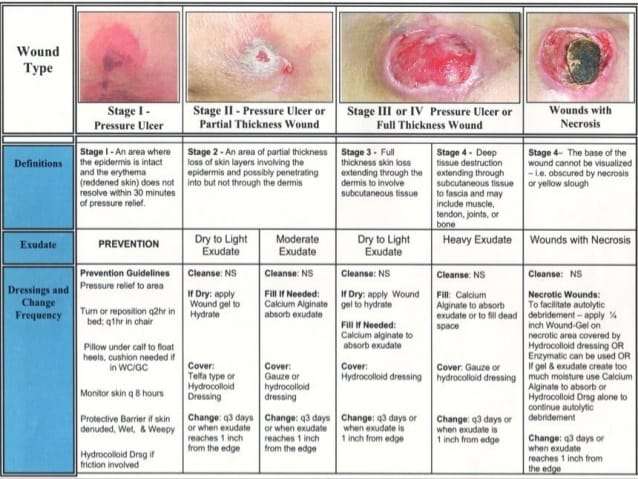
Stage 1 | Redness
There is a concentrated area of redness on a pigmented/discoloured skin. The skin might appear as blue or black.
Stage 2 | Partial Thickness Skin Loss
There is partial skin loss on the surface of the wound usually involves the epidermis layer . The ulcer is considered as superficial and looks like a abrasion, crater or blister type of wound.
Stage 3 | Full Thickness Skin Loss
Full thickness skin loss usually consists of damage to the subcutaneous tissues . The subcutaneous tissues act as a protective layer for our muscles and bones.
Stage 4 | Cavity
At this stage, patient will suffer from full thickness skin loss with tissue necrosis to the underlying bone, tendons and joint capsules.
The Available Reconstructive Options Are
Split thickness skin grafting
When the ulcer is superficial and vital tissues such as bone, vessels, nerves or tendons are not exposed, and the ulcer is not copiously discharging, skin grafting is the first option for surgical treatment. The slimy layer over the surface of ulcer is sharply debrided to get a healthy vascular bed for skin grafting.
Local flaps
Variety of local flaps can be used to reconstruct the defect created by excision of pressure ulcers. Local transposition, rotation, limberg flap are the available options .3]. Biceps femoris V-Y advancement for ischial pressure sore and perforator based V-Y advancement is another good options if the anatomy permits .
Sacral pressure sore , debridement and cover by local perforator based V-Y advancement flaps , 1-month post-operative , recurrence on the flap after 11 years due to loss of family support and subsequent improper care. Another patient with the same flap after 16-year of follow-up with a proper weight shifting and care showing stable coverage
Regional flaps
Medial planter flap for heel sore: A long-standing deep trophic ulcer of heel . The islanded medial planter flap was transposed to the defect and the resultant donor site was covered by split thickness skin graft . The 1-week and 3-month post-operative pictures showing stable coverage. Patient allowed full weight bearing from 6th week along with silicone footpad protection
Microvascular free flaps
Diagnosing A Stage 4 Bedsore
A doctor determines the by its appearance. In the case of a stage 4 bedsore, the large wound has passed the bodys fatty tissue layer, exposing muscles, ligaments, or even bone.
In some cases, however, health care professionals may not be able to immediately diagnose a late-stage bedsore by examining it.
A stage 4 bedsore may be initially diagnosed as:
- UnstageableWhen a doctor cannot see the bottom of an open sore, they must clean it out to properly stage it.
- Suspected Deep Tissue Injury This diagnosis happens when the surface of a patients skin looks like a stage 1 or 2 sore, but it is actually affecting deeper tissues underneath.
Also Check: Can Ulcerative Proctitis Be Cured
Negative Pressure Wound Therapy
This is an invaluable tool in the management of pressure sores and involves the application of sub-atmospheric pressure to a wound using a computerised unit to intermittently or continuously convey negative pressure to promote wound healing. NPWT, is effective for deep, cavitating, infected and copiously discharging pressure ulcers, particularly with exposed bone. With growing clinical experience it can be said with certainty that it assists wound healing, and its benefits can be summarised thus:
-
Assists granulation.
-
Applies controlled, localised negative pressure to help uniformly draw wounds closed.
-
Helps remove interstitial fluid allowing tissue decompression.
-
Helps remove infectious materials and quantifies exudates loss.
-
Provides a closed, moist wound healing environment
-
Promotes flap and graft survival.
-
Both hospital and domiciliary use.
-
Reduces hospital/dressings/nursing cost .
Can Pressure Sores Be Prevented Or Avoided
The best way to prevent pressure sores is to avoid spending long periods of time in a chair, wheelchair, or bed. If youre unable to move on your own, make arrangements for somebodysuch as a family member, friend, or caregiverto help you move.
If you must spend a lot of time in a chair, wheelchair, or bed, check your entire body daily. Look for spots, color changes, or other signs of sores. Pay attention to the pressure points where sores are most likely to occur. Again, if youre unable to look on your own, ask someone to help you.
Another way to avoid pressure sores is to keep your skin healthy. This includes keeping it clean and dry. Wash it with mild soap and warm water. Dont use hot water. Apply lotion often.
Even small amounts of exercise can help prevent pressure sores. Thats because exercise improves blood flow, strengthens your muscles, and improves your overall health. Talk to your doctor if physical activity is difficult. They can suggest certain exercises. Your doctor also may refer you to a physical therapist. They can show you how to do exercises that fit with your current health condition.
Lastly, if you smoke, quit. Smoking increases your risk of pressure sores.
Recommended Reading: Bone Broth And Ulcerative Colitis
Wound Care: Pressure Ulcer Best Practices
Pressure ulcers, otherwise known as decubitus ulcers, comprise a significant portion of wounds requiring specialized care and presenting additional costs, so prevention is critically important. A pressure ulcer is any lesion caused by unrelieved pressure resulting in damage of underlying tissue. Pressure ulcers usually occur over bony prominences and are graded or staged to classify the degree of tissue damage observed. Stage 1 pressure ulcers are defined as nonblanchable erythema of intact skin the heralding lesion of skin ulceration. Stage 2 is defined as partial thickness skin loss involving epidermis and/or dermis Stage 3 as full thickness skin loss involving damage or necrosis of subcutaneous tissue that may extend down to, but not through, underlying fascia and Stage 4 as full thickness skin loss with extensive destruction, tissue necrosis or damage to muscle, bone or supporting structures.
The Wound, Ostomy and Continence Nurses Society says that pressure ulcer prevention is best accomplished by identifying patients who are at risk for the development of pressure ulcers and initiating early preventive measures. According to the WOCN, This requires an understanding of risk factors, the utilization of research-based risk assessment tools, knowledge of appropriate preventive strategies and access to essential medical equipment such as therapeutic support surfaces.
Related Content:
Living With Pressure Sores
Living with pressure sores requires a plan to move and turn frequently. Good hygiene will always be required. Pressure sores should be kept covered with a bandage or dressing. Sometimes gauze is used. The gauze must be changed once a day. Newer materials include a see-through film and a hydrocolloid dressing. A hydrocolloid dressing is a bandage made of a gel. It molds to the pressure sore and promotes healing and skin growth. These dressings can stay on for several days at a time.
Dead tissue in the sore can interfere with healing and lead to infection. Dead tissue looks like a scab. To remove dead tissue, rinse the sore every time you change the bandage. Special dressings can help your body dissolve the dead tissue on its own. The dressing must be left in place for several days. Another way to remove dead tissue is to put wet gauze bandages on the sore. Allow them to dry. The dead tissue sticks to the gauze until it is removed. For severe pressure sores, dead tissue must be removed surgically by your doctor.
Removing dead tissue and cleaning the sore can hurt. Your doctor can suggest a pain medicine. Take it 30 to 60 minutes before changing the dressing.
Healthy eating helps sores heal. Make sure youre eating the proper number of calories and protein every day. Nutrients are important too, including vitamin C and zinc. Ask your doctor for advice on a healthy diet. Be sure to tell them if youve lost or gained weight recently.
Also Check: What Should You Eat When You Have Ulcerative Colitis
Positioning And Support Surfaces
Preamble: Pressure and compression to soft tissue play a role in the etiology of pressure ulcers. Patient positioning and methods to reduce pressure-related tissue damage are recognized as important treatment components. While there are limited definitive studies, the best current evidence and expert opinion suggest the following guidelines.
Guideline #1.1: Establish a repositioning schedule and avoid positioning patients on a pressure ulcer.
Principle: Pressure ulcers are thought to result from compression of soft tissues against a bony prominence. It is reasonable to assume that pressure on an ulcer can result in delayed healing. Patients should be repositioned to relieve pressure over bony prominences. The exact turning interval is not known and is derived empirically. Reductions in pressure incidence have been achieved, but positioning is not universally effective.
Evidence:
- 1
Clark M. Repositioning to prevent pressure soreswhat is the evidence? Nurs Standard 1998 13: 5664.
- 2
Defloor T. Less frequent turning intervals and yet less pressure ulcers. Tijdschrift voor Gerontologie en Geriatrie 2001 32: 1747.
- 3
Knox DM, Anderson TM, Anderson PS. Effects of different turn intervals on skin of healthy older adults. Adv Wound Care 1994 7: 4856.
- 4
Thomas DR. Are all pressure ulcers avoidable? J Am Med Directors Assoc 2001 2: 297301.
Evidence:
- 1
Thomas DR. Management of pressure ulcers. J Am Med Directors Assoc 2006 7: 4659.
Evidence:
Evidence:
Evidence:
Evidence:
How Can I Tell If I Have A Pressure Sore
- First signs. One of the first signs of a possible skin sore is a reddened, discolored or darkened area . It may feel hard and warm to the touch.
- A pressure sore has begun if you remove pressure from the reddened area for 10 to 30 minutes and the skin color does not return to normal after that time. Stay off the area and follow instructions under Stage 1, below. Find and correct the cause immediately.
- Test your skin with the blanching test: Press on the red, pink or darkened area with your finger. The area should go white remove the pressure and the area should return to red, pink or darkened color within a few seconds, indicating good blood flow. If the area stays white, then blood flow has been impaired and damage has begun.
- Dark skin may not have visible blanching even when healthy, so it is important to look for other signs of damage like color changes or hardness compared to surrounding areas.
- Warning: What you see at the skins surface is often the smallest part of the sore, and this can fool you into thinking you only have a little problem. But skin damage from pressure doesn’t start at the skin surface. Pressure usually results from the blood vessels being squeezed between the skin surface and bone, so the muscles and the tissues under the skin near the bone suffer the greatest damage. Every pressure sore seen on the skin, no matter how small, should be regarded as serious because of the probable damage below the skin surface.
Also Check: How To Know You Have A Ulcer
Selecting The Right Medical Tape For Sacral Pressure Ulcers Management
While substantial guidance is available for dressing selection, most clinical guidelines fail to discuss the importance of medical tape in sacral ulcer management. Sacral ulcers pose unique challenges in wound management, and the medical tape must be up to the task. Sacral ulcers are often subjected to excessive moisture and soiling from perspiration, urine, and fecal matter. The sacral area is subject to substantial friction and shear forces, as well. Each time the patient repositions themselves , the sacral area takes the brunt of this movement. Lastly, the sacral region is not uniform in shape. And sacral ulcers also tend have irregular borders. Dressings must be cut to fit the wounds, and tape must be able to provide a secure border on all sides.
If you care for someone who has or is at risk for sacral pressure ulcer, contact Hy-Tape for free sample.
References
1. Therattil PJ, Pastor C, Granick MS. Sacral pressure ulcer. Eplasty. 2013 13:ic18-ic18.
2. Bryant R, Nix D. Acute and chronic wounds: Current management concepts. Elsevier Health Sciences 2015.
Symptoms Of Pressure Sores
Pressure sores go through 4 stages.
- Stage 1. During this stage, the area of the sore looks red. It may feel warm to the touch. It may burn, hurt, or itch. The pressure sore may look blue or purple in people who have dark skin.
- Stage 2. During this stage, the area is more damaged. The sore may be open. It may look like a cut or blister. The skin around the sore may be discolored. The sore is painful.
- Stage 3. During this stage, the sore will have a crater-like look. This is due to increased damage below the surface. This makes the wound deeper.
- Stage 4. This is the most serious stage. Skin and tissue are severely damaged. The sore becomes a large wound. Infection is possible. Youre likely able to see muscle, bones, tendons, and joints.
Infected pressure sores take a long time to heal. Also, the infection can spread to the rest of your body. Signs of infection at the site include:
- Thick, yellow, or green pus
- A bad smell coming from the sore
- Redness or skin that is warm to the touch
- Swelling around the sore
Signs that the infection has spread include:
- Fever
- Weakness
Also Check: What To Eat If You Have Peptic Ulcer
Identifying A Stage 2 Bedsore
Stage 2 bedsores can be identified as an intact blister or shallow open sore. These sores are often red or pink and surrounded by red and irritated skin. These sores may also be moist if pus or fluid is present.
Human skin is made up of layers. The topmost level is called the epidermis. A stage 2 sore has broken the epidermis to create an open wound. The second layer of skin, the dermis, is visible in stage 2. In some cases, the dermis is broken.
Stage 2 bedsores have broken the skin but have not broken past the dermis to fat. The deeper a sore goes, the more difficult it will be to treat and the longer it will take to heal. People who are at risk of developing bedsores should receive regular skin checks to identify bedsores before they progress past stage 2.
Signs of a stage 2 bedsore include:
- Intact or ruptured blister
- Pus or fluid
- Redness or discoloration
Identifying a stage 2 sore as soon as possible is imperative. Complications can occur when bedsores go unnoticed and untreated. In serious situations, bedsores can become life-threatening or lead to amputation. If a sore becomes infected, the infection can spread to the blood, heart, or bones.
Notify a doctor or other healthcare provider if you or a loved one has developed a stage 2 bedsore. A health professional can decide the best plan of action to treat the bedsore properly.
Stage 4 Bedsore Prevention
The best way to prevent a stage 4 bedsore is by being proactive. If your loved one is at risk for bedsores, you can help them take the following precautions.
To prevent stage 4 bedsores, you can:
- Avoid buttons on clothes and wrinkles in bedding
- Avoid doughnut cushions, as they can add pressure to surrounding areas
- Change bedding and clothing on a regular basis
- Check skin daily
Also Check: How To Get Remission In Ulcerative Colitis
You May Like: Ulcerative Colitis Surgery Recovery Time
Assessing Sacral Pressure Ulcers
Pressure-induced skin and soft tissue injuries are often classified using the National Pressure Ulcer Advisory Panel staging system . Under this rubric, the wound should be staged to its deepest extent. This means selecting the highest number stage that accurately describes any part of the wound.
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
- Non-blanchable is redness that stays despite applying pressure. This means the erythema is not caused by blood within capillaries . Purple or maroon discoloration is not part of stage 1, but rather indicates a deep tissue pressure injury.
Severity Of Pressure Ulcers
Healthcare professionals use several grading systems to describe the severity of pressure ulcers most common is the EPUAP grading system. Pressure sores are categorised into four stages corresponding to the depth of damage. It must however be emphasised that when an eschar is present, accurate staging is not possible.
Don’t Miss: What Causes A Bleeding Ulcer In Stomach
How Can Pressure Injuries Be Prevented
The development of pressure injuries can be prevented through careful observation of the skin and frequent repositioning in those who canât turn themselves. Tips to prevent pressure injuries include:
- Keeping the skin clean and clear of bodily fluids.
- Moving and repositioning the body frequently to avoid constant pressure on bony parts of the body.
- Using foam wedges and pillows to help relieve pressure on bony parts of the body when turned in bed.
- Maintaining a healthy diet to avoid malnutrition and to assist in wound healing.
Treatment Of Stage 3 And Stage 4 Pressure Ulcers
The goal of treatment for stage 3 and 4 pressure ulcers, is to properly debride and dress the wound cavity, create or maintain moisture for optimal healing, and protect the wound from infection. The goal of properly unloading pressure from the area still applies. At these pressure ulcer stages, more emphasis should be placed on proper nutrition and hydration to support wound healing. If the extent of the pressure ulcer or other factors prohibit it from healing properly, surgery may be necessary to close the wound.
The following precautions can help minimize the risk of developing pressure ulcers in at-risk patients and to minimize complications in patients already exhibiting symptoms:
- Patient should be repositioned with consideration to the individualâs level of activity, mobility and ability to independently reposition. Q2 hour turning is the standard in many facilities, but some patients may require more or less frequent repositioning, depending on the previous list.
- Keep the skin clean and dry.
- Avoid massaging bony prominences.
Recommended Reading: Herbal Medicine For Ulcerative Colitis
Recommended Reading: Things To Eat When You Have An Ulcer