Researchers At Case Western Reserve University Found The Fungus Works With Two Types Of Bacteria To Cause Symptoms Of The Disease
CLEVELAND, Sept. 21 Researchers at Case Western Reserve University identified a fungus that works with two types of bacteria to cause symptoms of Crohns disease, according to a new study.
The study is the first to find a fungus plays a role in development of the disease, and the discovery may lead to new ways of treating Crohns, according to researchers involved with the study.
Crohns disease is an inflammatory bowel disorder that causes inflammation of the digestive tract leading to abdominal pain, severe diarrhea and fatigue, and is one of the most common forms of inflammatory bowel disorder.
We already know that bacteria, in addition to genetic and dietary factors, play a major role in causing Crohns disease, Dr. Mahmoud Ghannoum, a professor and director of the Center for Medical Mycology at Case Western Reserve University and lead author of the study, said in a press release. Essentially, patients with Crohns have abnormal immune responses to these bacteria, which inhabit the intestines of all people. While most researchers focus their investigations on these bacteria, few have examined the role of fungi, which are also present in everyones intestines.
For the study, , the researchers analyzed fecal samples from 20 people with Crohns disease and 28 of their Crohns-free family members, as well as from 21 people who did not have the disease and neither did their family members.
Also Check: What Is The Medicine For Ulcer
How Do Crohns Disease And Ulcerative Colitis Interfere With Digestion
To get a better idea of how diet affects people with IBD, heres a brief explanation of the way in which the body processes the food you put into it.
The real work of the digestive system takes place in the small intestine, which lies just beyond the stomach. In the small intestine, digestive juices from both the liver and the pancreas mix with food. This mixing is powered by the churning action of the intestinal muscle wall. After digested food is broken down into small molecules, it is absorbed through the surface of the small intestine and distributed to the rest of the body by way of the bloodstream. Watery food residue and secretions that are not digested in the small intestine pass on into the large intestine . The colon reabsorbs much of the water added to food in the small intestine. This is a kind of water conservation or recycling mechanism. Solid, undigested food residue is then passed from the large intestine as a bowel movement.
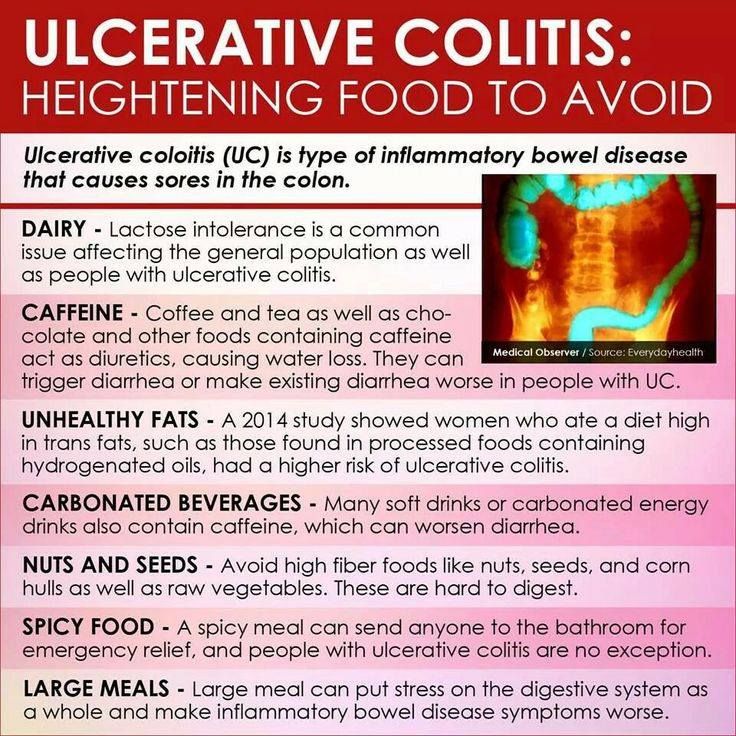
In ulcerative colitis, only the colon is inflamed the small intestine continues to worknormally. But because the inflamed colon does not recycle water properly, diarrhea can be severe.
Additional Therapies To Augment Mold Detoxification & Healing
- Movements & Exercise:Depending on your health and fitness level, try to introduce gentle physical activity you can do each day, such as a walking, stretching, using a rebounder .
- Skin & Lymphatic Support:Use infrared saunas or a restorative mineral bath such as Clear + Restore.
- Hyperbaric Oxygen Therapy:This method improves oxygenation which can accelerate the bodys ability to detox and eliminate toxins. It can be very useful if your symptoms affect your memory and brain. Oxygen is also beneficial for the healing of tissues.
Read Also: Zinc Oxide For Stage 2 Pressure Ulcer
You May Like: How To Get Rid Of Eye Ulcer
What Are The Risk Factors For Appendicitis
Theres no way to predict who will get appendicitis, but scientists have uncovered several risk factors for the condition. These include:
- Being a teenager or in your twenties most cases of appendicitis occur in this age group
- Having a long-lasting inflammatory bowel disease, such as Crohns disease or ulcerative colitis
- Studies have suggested that family history plays a role a study published in 2014 in the Western Journal of Emergency Medicine found that among adults at an emergency room who presented with appendicitis, those with a known family history were more likely to have the condition
And a study published in 2001 in the Journal of Pediatric Surgery found that heredity is a significant factor in children who have appendicitis.
Theres also a link between air pollution in particular, high levels of ozone and appendicitis. Scientists arent sure why air pollution is associated with an increased risk of appendicitis, but it may be that high levels of ozone increase intestinal inflammation or increase susceptibility to bacterial and viral infections.
Studies suggest that people get appendicitis more during the summer than at other times of the year. Its not clear why, but a review of over 40 years of research, published in February 2014 in Annals of Medical and Health Sciences Research, concludes that its likely due to a combination of increased exposure to air pollution and more GI infections during summer months.
Also Check: Can Ulcerative Colitis Go Into Remission
How I Know That Thrush Is Coming
Your spit is thick, you can clear your throat 100 times, but it wont feel clear. Thats my big uh-oh indicator to knowing thrush is coming for me. You cant swallow comfortably and everything hurts to eat.
Ill leave some foods to avoid based on previous GI recommendation and based on my own personal experience. Eating or drinking the wrong thing can actually irritate your infection more and feel like youre swallowing parts of a cactus.
Don’t Miss: Patient Education On Pressure Ulcer Prevention
Mold Increases Your Susceptibility To Gut Infections
Those who develop symptoms caused by mold often experience a variety of gastrointestinal issues, including gut infections. Mycotoxin exposure may directly increase your susceptibility to bacterial, viral, and parasitic gut infections by decreasing your intestinal immunity.
In animal studies, ochratoxin triggered viral gut infections and strengthened the virulence of intestinal parasites. In chickens, Fusarium decreases populations of CD4+ and CD8+ cells , increasing the risk of coccidiosis, an intestinal disease that easily spreads from bird to bird. Furthermore, the effectiveness of antiparasitic drugs is reduced by high levels of circulating mycotoxins, suggesting that mycotoxin exposure should be addressed first before attempting to treat parasitic infections.
A Case On Candida And Ulcerative Colitis
By | Submitted On March 17, 2010
This article will discuss about Candida and Ulcerative Colitis . This is based from someone who sent me an email. He is 24 years old from the United Kingdom. He’s suffered from candida and ulcerative colitis, although he thought candida might be the cause of his UC. He’s suffered from UC without remission for 7 years.
He’s having difficulty coming off steroids. He’d started an anti-fungal/diet program again, but every time he took anti-fungals, the yeast would come back the following day, and he would feel very tired during the morning. He thought it’s because her adrenals were having a hard time coping with the die-off. He’s currently at 1mg of prednisolone, he was wondering if he may need to increase his dose to 2.5 mg so that he can get things moving with the anti-fungals and his adrenals can cope with the die-off.
Dealing with those circumstances, a lot of sources have recommended that you do the diet for a few weeks before starting on anti-fungals to avoid the problem of a sudden, massive die-off.
Once you realize what the yeast can do, anytime you have symptoms of any kind, just continue your medicines but cut back on them and take lots of colon cleanse and distilled water. You should have a die-off and once that happens you will feel better. But beware and keep taking your medicines like before. Maybe now you can tolerate your usual dosage and you probably will have another die-off but not before you start feeling bad again.
Recommended Reading: How Can You Prevent Pressure Ulcers
Treating Ulcerative Colitis With A Candida Cleanse
I think the Candida cleanse is an excellent idea for somebody who has ulcerative colitis . Just like it is for somebody with irritable bowel syndrome.
UC is a type of inflammatory bowel disease . Crohns disease is another form of IBD. Ulcerative colitis is a little bit different from Crohns disease in that Crohns is more damaging. Crohns disease affects deeper layers of the gut mucosa compared to UC. Its a nasty disease. I like to use the analogy of meeting people. Youll meet some really nice people. Youll meet some people that are not so nice, and youll meet some bad people. Then, occasionally youll meet a horrible, nasty person. Thats Crohns disease.
UC is definitely controllable. Ive worked with several hundred UC patients over the years, and Ive had excellent outcomes in most cases. Colitis responds well to the Candida cleanse because of the diet change. Were taking all the crap out the diet. Were cleaning the diet right up. Were going to clean up the microbial component of the gut, which is very important with ulcerative colitis.
Further readings:
Once youve determined whats in your gut, the Candida cleanse can be tailored to suit your UC. You can get a great outcome with colitis by testing, analyzing, treating, re-testing, and fine-tuning the Candida Crusher program to suit yourself.
Are There Ways To Prevent This
While an unhealthy gut can be the result of genetics or underlying disease, there are some things you can do to help keep your intestines healthy. These include:
- Only take antibiotics when necessary. In addition to killing whatever is making you sick, antibiotics can reduce the levels of good bacteria in your gut. This can allow Candida to grow. Sometimes its necessary to take antibiotics, but make sure you only take them in those cases.
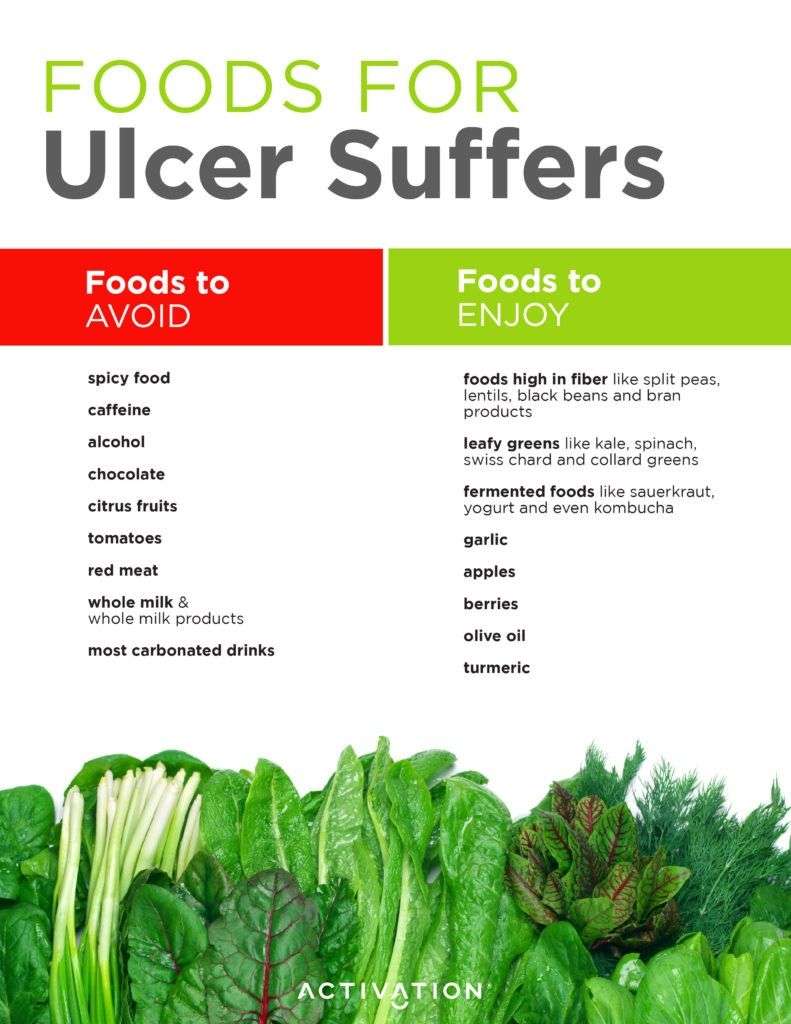
- Eat a healthy diet. A healthy diet that includes whole grains and foods with lots of fiber, such as beans and apples, will help keep your gut healthy. Increasing the diversity of bacteria in your gut is another way to make sure your intestinal environment stays healthy. You can do this by eating a wide variety of healthy foods.
- Take probiotics.Probiotics are supplements made up of live microorganisms, usually bacteria. Theres mixed evidence for them, but some research suggests that taking probiotics can help the bacteria in your gut stay balanced. Talk to your doctor about adding a probiotic to your daily routine.
- Eat fermented foods.Fermented foods, such as sauerkraut, kimchi, and yogurt, are foods that have been altered by bacteria or yeasts. Therefore, they contain a lot of bacteria that can help keep your gut healthy.
- Eat prebiotic food. Prebiotic foods promote the development of good bacteria in your gut. Foods with lots of fiber or complex carbs are your best sources of prebiotics. These include fruits, vegetables, and whole grains.
Read Also: Pediatric Ulcerative Colitis Activity Index
What Are The Symptoms Of Candida In The Gut 6 Causes
Candida is a type of fungus that is commonly found on the skin and in the gut and is usually harmless until an overgrowth occurs. An overgrowth of Candida in the gut can cause flare-ups of existing gastrointestinal diseases such as ulcerative colitis and Crohns disease.
Signs and symptoms vary depending on the part of the body involved. Symptoms of Candida in the gut may include:
Some practitioners of complementary and alternative medicine claim that an overgrowth of Candida in the gut can also cause yeast syndrome, which is characterized by symptoms such as fatigue, migraines, headache, and poor memory. They often advise a Candida cleanse for this condition, which is a diet that eliminates sugar, white flour, yeast, and cheese.
Although there is little evidence that dietary changes can stop yeast overgrowth in the gut, adopting healthy diet habits can definitely keep your gut bacteria healthy.
Symptoms Of Oral Thrush
Thrush can cause a wide variety of symptoms in patients like pain and irritation while swallowing, feeling like you have phlegm in the back of your throat but you just can’t get rid of it, and many more symptoms like fatigue, headache, and fever. Usually, mine show up with fevers, which cause me severe fatigue.
Your doctor may prescribe some magic mouthwash for you as well, which is very helpful. If you struggle with thrush often, I highly suggest you ask your doctor for the medicated kind, or you can make your own at home with just a few simple over the counter medications.
You May Like: What Helps Ulcers In Your Mouth
Is The Gut A Source For C Albicans Systemic Infections
Different studies suggested that the gut is the main reservoir from which C. albicans can translocate through the intestinal barrier causing blood stream infections . Immunocompromised animals or those with disrupted intestinal barriers can develop BSI leading to dissemination, colonization of vital organs, and death. Molecular typing studies have demonstrated that systemic infections originate from the gastrointestinal tract . Genetic similarity between C. albicans blood isolates and the corresponding strains isolated from stools was found in systemically infected patients . A comparative analysis of the mycobiota in fecal and blood samples from allogenic hematopoietic cell transplant patients has revealed an expansion of the intestinal Candida species prior to dissemination . In fact, the majority of intensive care unit patients, a major risk group for systemic Candida infections, seem to show increased sizes of certain Candida populations in the gut . Therefore, microbial dysbiosis and Candida overgrowth in the gut can be considered a risk and a source for systemic candidiasis, besides catheter-derived nosocomial candidemia.
Things That Can Help With Thrush:
- Yogurt drinks – Chobani has some delicious yogurt drinks in many different flavors and I cant stress enough how much I live on these during the weeks I have thrush. Sometimes its all Im able to get into my body.
- There is also a very helpful resourceful diet that helps many patients who deal with chronic thrush called the candida diet.3
You dont have to go through the pain of thrush alone. So often many of us on steroids and inhalers deal with it, and it doesnt get easier until you know what you should be avoiding and what you should be putting into your body to make your mouth and throat feel better. It took my years to learn that soda and natural sugars were making my mouth completely worse and so much more painful than it had to be.
If you struggle with thrush, talk to your doctor to discuss your symptoms and how often youre getting it. Consider getting rid of the substances youre putting into your body that may be making the thrush worse.
You May Like: Foods To Stay Away From With Ulcers
Vitamin And Mineral Supplements For Ibd
A person with IBD who eats a healthy, varied diet does not usually need to take vitamin supplements. But if they have a dietary deficiency, they may need tablets or occasional vitamin B12 injections. For example, a person on a low-fibre diet may need extra vitamin C and folic acid because they dont eat enough fruit and vegetables.A person with Crohns disease who experiences steatorrhoea may need calcium and magnesium supplements. Most children with IBD should take supplements to help them grow and develop normally.
Read Also: Is Kimchi Good For Ulcerative Colitis
Menstrual Periods May Aggravate Your Uc
More than half of women say their IBD symptoms get worse when theyre on their period, according to a study of more than 1,000 females published in January 2018 in the journal Inflammatory Bowel Diseases.
These symptoms may include increased frequency of bowel movements, more gas or bloating, or increased abdominal pain, says Emanuelle A. Bellaguarda, MD, an assistant professor at the Feinberg School of Medicine at Northwestern University in Chicago.
Experts arent exactly sure why women experience more symptoms during menstruation, but the Inflammatory Bowel Diseases research suggests it may be caused by hormonal changes. During menstruation, women produce more hormone-like compounds called prostaglandins, which cause increased contractions of the smooth muscles in the colon. This may cause gastrointestinal problems such as diarrhea and abdominal cramps.
The good news is that these symptoms dont necessarily lead to a flare or increased inflammation, says Dr. Bellaguarda, and they should subside after your monthly period. I reassure my patients that theyre not experiencing a flare every month, she says.
Read Also: Ulcerative Colitis Joint Pain Treatment
Why Do I Often Get Thrush
Those most vulnerable to thrush: patients with compromised immune systems, older populations, infants as well.1Prednisone may also be a factor in thrush, as well as weakened immunity, vaginal yeast infections, some medications, and dentures.
You can help prevent oral thrush by maintaining good oral health and washing/swishing your mouth out VERY well after using inhalers if you use them for another medical condition.2
Helping Gut Health Naturally
1. Removal of problematic foodsIgG food intolerancesulcerative colitisceliac diseaseThe Specific Carbohydrate Diet2. Manage inflammation.side effects3. Protect and restore the intestinal barrier.4. Remove pathogens.Candidaoregano oilnonilactoferrincranberry extractgymnema sylvestrecinnamonshark liver oil5. Restore healthy gut flora. C-section deliveries
Don’t Miss: Can I Live A Normal Life With Ulcerative Colitis
Causes Of Candida Overgrowth In The Gut
Typically, Candida overgrowth is prevented by a healthy immune system and balanced bacterial flora in the gut. When these two factors are affected, Candida can build up in the gut and cause infection:
- Gut inflammation: Diseases such as ulcerative colitis and Crohns disease predispose a person to Candida overgrowth because there are already lesions in the gut that can be easily infected by fungi.
- Diabetes: Diabetes increases blood sugar levels, which creates a favorable environment for fungal buildup.
- Proton pump inhibitor use: PPI is used in the treatment of acid reflux. The decrease in acid production increases the risk of bacterial and fungal buildup.
- Antibiotics: Antibiotics, especially the broad-spectrum ones, kill a lot of good bacteria in the gut that are used to fight against the Candida.
- Steroid use: Long-term use of steroids can affect the immune system and increases the risk of bacterial infection in the body.
- Immunosuppressive drugs: Anticancer drugs affect immune cells and increase the risk of bacterial buildup.