Disease Course Therapeutic Strategies And Complications
The use of mesalamine as a therapy for induction of remission was similar in the two groups , as well as steroid therapy and surgery . .
Table 2 UC therapeutic strategies, disease course and complications
Globally, surgery was performed more frequently in the elderly , with a mean time between diagnosis and surgery of 18.4months in the elderly and 24.87months in younger patients .
The type of surgery most frequently performed was partial colic resection , followed by perianal disease , colectomy and resection for cancer in the elderly colectomy and perianal disease in adults.
As maintenance therapy, there was no difference between the two groups in the use of mesalamine and immunosuppressant while biologic agents were much less used in the elderly .
During follow up, 57% of patients had at least one disease exacerbation, with a similar median time to first relapse . p 0.5615.
Extraintestinal manifestations were less common in the elderly , . Intestinal complications were more frequent in the elderly . In particular, stenosis was the most frequent complication in both groups. The other ones were toxic megacolon, intestinal perforation and haemoperitoneum.
Moreover, major infections were more common in the elderly . The most frequent infection was pneumonia in both groups . The other ones were sepsis , C. difficile infection for the elderly and CMV infection for the adults . Herpes Zoster infection and systemic candidiasis were also reported.
What Causes Ulcerative Colitis In A Child
Healthcare providers don’t know what causes this condition. It may be triggered by a virus or bacteria. This interacts with your childs immune system and causes an inflammatory reaction in the intestinal wall.
Children with ulcerative colitis often have problems with their immune system. But healthcare providers don’t know if these issues are a cause or a result of the disease.
Theres no cure for this condition, except to take out your childs colon with surgery. However, the symptoms can be managed medically.
What Are The Mortality Rates For Ulcerative Colitis
The various forms of IBD, including ulcerative colitis, are not usually considered to be fatal.
However, the life span of a person with ulcerative colitis or another form of IBD may be slightly shorter than for those who dont live with one of these diseases. This is believed to result from the ongoing inflammation, which puts people at risk for heart disease, cancer, and other conditions.
Also Check: Is Keto Good For Ulcerative Colitis
How Is Ulcerative Colitis Diagnosed In Children
Diagnosing ulcerative colitis begins with an examination and a detailed medical history. Your childs clinician will rule out other possible causes and may recommend one or more of the following tests:
Drug therapy can reduce inflammation and control symptoms. Ulcerative colitis medications may include:
- anti-inflammatory drugs, such as steroids, to bring the disease under control
- immune system suppressants that can reduce swelling
- antibiotics to treat related complications, such as abscesses or fistulas
- antiulcer/H2 blockers to treat related ulcers and irritation
Causes Of Ulcerative Colitis
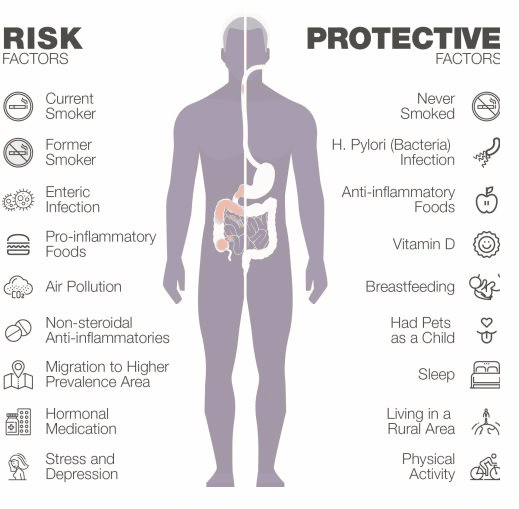
Ulcerative colitis is the result of several factors that are not yet well understood. Abnormal immune response, genetics, microbiome, and environmental factors all contribute to ulcerative colitis.
Research suggests that ulcerative colitis could be triggered by an interaction between a virus or bacterial infection in the colon and the bodys immune response.
-
Typically, the cells and proteins that make up your immune system protect you from infection.
-
A normal immune response would cause temporary inflammation to combat an illness or infection. The inflammation would then go away once you are healthy and free of the illness.
-
In ulcerative colitis patients, the inflammation persists long after the immune system should have finished its job. The body continues to send white blood cells into the lining of the intestines, where they produce chronic inflammation and ulcers.
Recommended Reading: What Doctor Treats Ulcerative Colitis
Why Are Cases Of Uc Increasing In Older Populations
There are several factors that could explain why the incidence of UC is increasing in the older population.
Cases may be increasing because doctors are better able to diagnose UC. Cases of UC in older populations are increasing at a faster rate in higher-income urbanized environments, so better access to healthcare can partially explain this phenomenon.
However, people who live in cities and densely populated towns also tend to eat a more westernized diet, which is high in saturated fat and refined carbohydrates. When people routinely eat these types of foods, they disturb their microbiota and increase their risk of UC.
Other environmental factors that can increase a persons UC risk include air pollution, lack of sleep and exercise, and high stress levels.
Crohns Disease And Ulcerative Colitis And Diet
Diet and food allergies do not cause IBD, and long-term special diets are not effective in treating IBD. However, adjusting your diet can help manage some of your symptoms, and can help IBD medications work better. A person with IBD has to pay close attention to their diet, since they may have malnutrition.
Recommended Reading: Can Peptic Ulcer Be Cured
Skin Joint Or Eye Problems
When you have UC, the lining of your large intestine gets inflamed and sets off your symptoms. For some people, this inflammation also shows up in other body parts during a flare. Experts arent sure why.
You could have symptoms like:
Let your doctor know whenever you get new UC symptoms. That way, they can change your treatment plan if needed.
Is Ulcerative Colitis Genetic
One of the single biggest risk factors for UC and Crohnâs disease is a family history of the disease.
About 10% to 25% of people diagnosed with UC have a parent or sibling with IBD. Youâre four to eight times more likely to develop some type of IBD if you have a close relative with the condition.
Researchers have found changes, or variants, in several genes that they think are linked to UC. They theorize that these variants might cause your immune system to overreact to normal bacteria in your gut, or affect the protective barrier in the lining of your intestine.
Don’t Miss: How Can You Tell If You Have An Ulcer
How Is Inflammatory Bowel Disease Diagnosed
Your doctor will give you a physical exam and listen to you describe your symptoms. To help diagnose the problem your doctor may order a number of tests, including blood tests and stool samples. Your doctor may also order one or more procedures to help them view your colon. Lower GI endoscopy procedures include colonoscopy and flexible sigmoidoscopy. During these procedures, your doctor uses a narrow, flexible tube to look directly inside your large intestine. Upper GI endoscopy allows a look at your stomach and small intestine for ulcers. For this type of endoscopy, you may swallow a small camera . If not, your doctor inserts a scope into your GI tract through your mouth.
Your doctor may also order other imaging tests such as X-rays, a CT scan, or an MRI.
Also Check: Can Ulcers Cause Chest Pain And Shortness Of Breath
The Connection Between Ibd And Aging
Inflammatory bowel disease has long been thought of as an ailment of middle, or even young, adulthood. The chronic illnesswhich includes Crohns disease and ulcerative colitis, and can cause abdominal pain, diarrhea, bleeding, and decreased quality of lifeimpacts about 3.1 million people in the U.S. However, it is far from a disease only of the young and middle-aged. More than a quarter of people with IBD are elderly, a figure that is projected to climb to 30% by 2030, according to a 2021 Gastroenterology & Hepatology article.
Even more underappreciated is the growing population of people who are diagnosed with the disease after they turn 60. Whereas IBD was once taught as a disease with two spikes in onset20s to 30s, and 40s to 50sdoctors are learning there is a third spike that begins later in life. Now we know you can be 75 and get IBD, says Dr. Simon Hong, a gastroenterologist and IBD specialist at NYU Langone Health.
Regardless of when the disease starts, however, understandingand treatingIBD in older adults comes with its own set of challenges and intricacies.
Recommended Reading: How To Heal Mouth Ulcers
Ibd Looks Different In Older Adults
Hundreds of thousands of people whose IBD was diagnosed earlier in their lives are now living with the disease in older age. For many that means living with the damage the disease has done to their intestinal tract, and sometimes with the altering impacts of surgery done to manage it, such as ostomy pouches or increased incontinence. Not to mention continued flare-ups.
It used to be commonly thought that disease activity tapered off in older age, and some people do find their IBD becomes inactive later in life. But that isnt always the case, says Cleveland Clinic gastroenterologist Dr. Jessica Philpott. I certainly see some patients who develop more aggressive disease as they advance in age, she says.
For individuals who get IBD after they turn 60, the disease can look somewhat different than for those who have had it for decades. Whereas younger Crohns patients can have damage in any part of their intestinal tract, in older-onset cases it more often primarily affects the colon.
And because older adults have often already faced more health issues, they might not seek medical help as promptly. Crohns in particular can be trickier to pinpoint than ulcerative colitis, as it might present as intermittent abdominal pain and weight loss, which arent uncommon in older adults generally. These factors can sometimes delay proper diagnosis, and thus effective treatment, by years.
Ulcerative Colitis: Treatment And Therapy
The cause of the inflammatory bowel disease ulcerative colitis is not yet known. Therefore, the goal of treatment is to alleviate the symptoms as well as to prolong the symptom-free phases.
Various drugs are used for this purpose: 5-aminosalicylic acid is an anti-inflammatory agent that is prescribed in the form of the precursor mesalazine as tablets, suppositories, foams or enemas. Corticosteroids also have an anti-inflammatory effect and are used either as suppositories, enemas or tablets. Both medications containing the active ingredient mesalazine and cortisone can cause severe side effects. Cortisone in particular can cause long-term side effects.
In severe cases or when cortisone is not effective, some patients receive immunosuppressants . This can have a positive effect on the course of the disease. However, TNF antibodies , which inhibit the inflammatory messenger TNF, can also be considered. When taking immunosuppressants and TNF antibodies, severe side effects such as susceptibility to infections can also occur, and poisoning is also possible.
Which drugs are used in treatment always depends on various factors, such as the extent of the symptoms and how far the inflammation has spread in the intestine, among other factors.
In addition to drug therapy, it is important for those affected to ensure a varied and balanced diet and to avoid hard-to-digest food components and hot spices during an acute episode.
Also Check: Natural Way To Cure Ulcer
Recommended Reading: Do Ulcers Cause Acid Reflux
Complications Caused By Nutritional Deficiencies
Some of the complications of malnutrition include:
- Dehydration diarrhoea causes your body to lose fluid, which can lead to dehydration. Severe dehydration can damage your kidneys.
- Anaemia reduced iron in the diet combined with losing blood from the bowel can lead to anaemia .
- Weight loss reduced appetite and poor absorption of food nutrients can cause weight loss.
- Reduced growth inadequate nutrition during childhood and adolescence can impair a childs growth and physical development.
How We Care For Ulcerative Colitis
At the Boston Childrens Inflammatory Bowel Disease Center, our team believes that, with proper management, all children and teens with ulcerative colitis can live comfortably. We partner with you and your child to effectively manage IBD and provide support through all life stages, from school and relationships to work.
Don’t Miss: Can You Heal A Stomach Ulcer
Extraintestinal Manifestations And Complications
UC is characterized by immune dysregulation and systemic inflammation, which may result in symptoms and complications outside the colon. Commonly affected organs include: eyes, joints, skin, and liver. The frequency of such extraintestinal manifestations has been reported as between 6 and 47%.
UC may affect the mouth. About 8% of individuals with UC develop oral manifestations. The two most common oral manifestations are aphthous stomatitis and angular cheilitis. Aphthous stomatitis is characterized by ulcers in the mouth, which are benign, noncontagious and often recurrent. Angular chelitis is characterized by redness at the corners of the mouth, which may include painful sores or breaks in the skin. Very rarely, benign pustules may occur in the mouth .
UC may affect the eyes. Inflammation may occur in the interior portion of the eye, leading to uveitis and iritis. Uveitis can cause blurred vision and eye pain, especially when exposed to light . Untreated, uveitis can lead to permanent vision loss. Inflammation may also involve the white part of the eye or the overlying connective tissue , causing conditions called scleritis and episcleritis. Uveitis and iritis are more commonly associated with ulcerative colitis, whereas episcleritis is more commonly associated with Crohns disease.
Little Girl Visited By Gary Neville At Childrens Hospital Ends Up Working For Footy Legend 15 Years Lateryour Browser Indicates If Youve Visited This Link
A woman who was visited in hospital by Gary Neville 15 years ago has shared the inspirational story of how she now works alongside the football legend. Jenny Byrne, 21, from Stockport, was rushed into hospital at the age of six and was later diagnosed with UlcerativeColitis an inflammatory bowel disease.
Manchester Evening News on MSN.com
Don’t Miss: What Are The Signs Of Having A Stomach Ulcer
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Will Ulcerative Colitis Affect Me Over Time
The effects of ulcerative colitis vary considerably from person to person, based on the nature and severity of their disease. In many cases, the condition does not have much impact on daily life, the ability to work or to enjoy an active social life but does take some getting used to. When it is at an active stage, symptoms such as diarrhoea and abdominal pain often require time away from work, college etc. and can make it difficult to cope going out or even being at home. However, treatment usually makes the symptoms better within days or weeks so normal quality of life can be restored quite quickly. Some severe cases of ulcerative colitis, however, can have a significant impact on peoples lives. This can be due to a weak response to treatment which makes symptom-free remission difficult to achieve and can involve frequent flare ups.
Read Also: How To Prevent Hospital Acquired Pressure Ulcers
Do Patients With Ulcerative Colitis Diagnosed At A Young Age Have More Severe Disease Activity Than Patients Diagnosed When Older
Log in to MyKarger to check if you already have access to this content.
Buy a Karger Article Bundle and profit from a discount!
If you would like to redeem your KAB credit, please log in.
Save over 20%
- Unlimited fulltext viewing Of this article
- Organize, annotate And mark up articles
- Printing And downloading restrictions apply
- Access to all articles of the subscribed year guaranteed for 5 years
- Unlimited re-access via Subscriber Login or MyKarger
- Unrestricted printing, no saving restrictions for personal use
The final prices may differ from the prices shown due to specifics of VAT rules.
Ulcerative Colitis Is A Type Of Ibd
There are two main types ofinflammatory bowel diseases ulcerative colitis andCrohns disease. Ulcerative colitis is more common worldwide than Crohns disease.
It causes inflammation and sores in the large intestine and may affect part or all of the large intestine.
Ulcerative colitis can happen at any age, but it is more likely to develop in people between the ages of 15 and 30, or older than 60 years of age.
Ulcerative colitis needs to be diagnosed by a health care provider. While there are no cures, there are treatments.
Don’t Miss: Ulcerative Colitis Abdominal Pain Relief
What Is The Outlook
With modern medical and surgical treatment, there is just a slight increase in the risk of death in the first two years after diagnosis, compared with the general population. After this there is little difference in life expectancy from that of the general population. However, a severe flare-up of ulcerative colitis is still a potentially life-threatening illness and needs expert medical attention.
As mentioned, if you do not take medication to prevent flare-ups, about half of people with ulcerative colitis have a relapse on average once a year. This is much reduced by taking regular medication. However, even in those who take regular medication, some people have frequent flare-ups and about a quarter of people with ulcerative colitis eventually have an operation to remove their colon.
A year from diagnosis, about 9 in 10 people with ulcerative colitis are fully capable of work. So, this means that, in the majority of cases, with the help of treatment, the disease is manageable enough to maintain a near-normal life. However, the condition can cause significant employment problems for a minority.
Treatment for ulcerative colitis is an evolving field. Various new medicines are under investigation. These may change the treatment options over the next ten years or so and improve the outlook .
Dont Miss: How Long Does Prednisolone Take To Work For Ulcerative Colitis