Who Should I Contact If I Think Ive A Pressure Ulcer
If youre at all worried, think you may be/have developed a pressure ulcer or may be at risk of developing one due to your circumstances and would like to take preventative measures then your first port of call should be to contact your GP or healthcare professional as soon as possible.
The quicker a pressure ulcer is identified, the easier it is to prevent or treat.
Reference: Kent Community Health NHS Foundation Trust
Position Changes To Prevent Pressure Sores
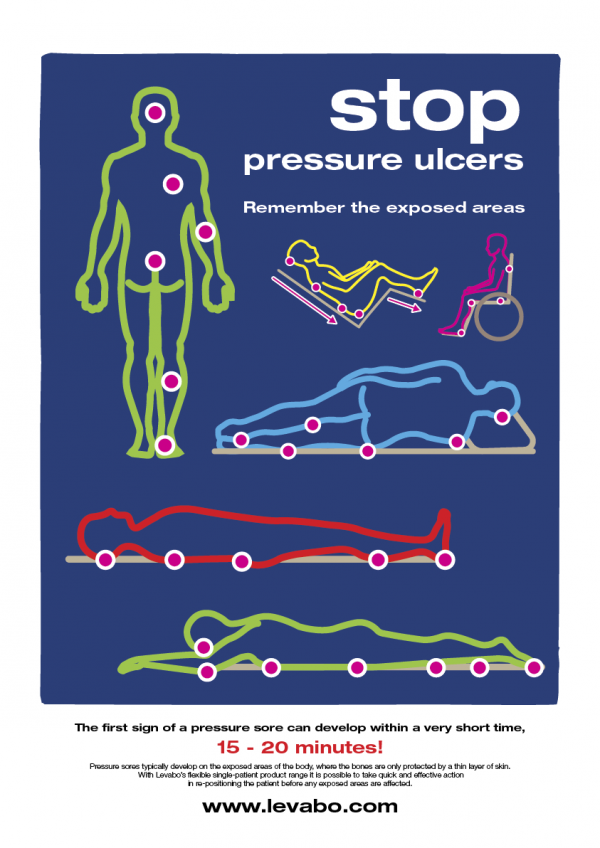
If you use a wheelchair shift position within your chair about every 15 minutes. If you spend most of their time in bed change position at least once every two hours, even during the night and avoid lying directly on your hipbones.
Pillows may be used as soft buffers between your skin and the bed or chair. The head-of-bed elevation should be maintained at/or below 30 degrees. Or depending on the your medical condition, the bed should at least be elevated to the lowest degree to prevent injury. When lying on your side, a 30 degrees position should be used.
The Case For Prevention
Pressure ulcer prevention entails two major steps: identifying patients at risk and reliably implementing prevention strategies for all patients identified as at risk. Prevention strategies include six key elements : conduct a pressure ulcer admission assessment for all patients, reassess risk for all patients daily, inspect skin daily, manage moisture, optimize nutrition and hydration, and minimize pressure. Facilities may wish to form a multidisciplinary team to develop a pressure ulcer prevention program.
Don’t Miss: How Do You Check For A Stomach Ulcer
Key Points About Bed Sores
- Bedsores are ulcers that happen on areas of the skin that are under pressure from lying in bed, sitting in a wheelchair, and/or wearing a cast for a prolonged period.
- Bedsores can happen when a person is bedridden, unconscious, unable to sense pain, or immobile.
- Bedsores can be prevented by inspecting the skin for areas of redness every day with particular attention to bony areas.
Turn Everyone And Move Study
The Turn Everyone And Move study13 was a 12-month paired facility 2-arm randomized intervention trial that tested the effectiveness of musical cues reminding LTC nursing and ancillary staff to help residents to move or reposition all residents, regardless of identified risk level, every 2 hours in 10 US LTC facilities. Staff and visiting family members received education on both PrU prevention and the intervention. Musical selections based on facility preferences were played over the facility public address system every 2 hours for the 12-hour daytime period. Intervention facility residents were 45% less likely than comparison facility residents to develop a new PrU. The researchers concluded that a broad approach involving customized musical cues that prompt multidisciplinary staff teams to encourage or enable all residents to move holds promise for reducing facility-acquired PrUs in LTC settings.13,26
Also Check: How Do You Get Mouth Ulcers
When You Are In Bed
Use a foam mattress or one that is filled with gel or air. Place pads under your bottom to absorb wetness to help keep your skin dry.
Use a soft pillow or a piece of soft foam between parts of your body that press against each other or against your mattress.
When you are lying on your side, put a pillow or foam between your knees and ankles.
When you are lying on your back, put a pillow or foam:
- Under your heels. Or, place a pillow under your calves to lift up your heels, another way to relieve pressure on your heels.
- Under your tailbone area.
- Under your shoulders and shoulder blades.
- Under your elbows.
Other tips are:
- DO NOT put pillows under your knees. It puts pressure on your heels.
- Never drag yourself to change your position or get in or out of bed. Dragging causes skin breakdown. Get help if you need moving in bed or getting in or out of bed.
- If someone else moves you, they should lift you or use a draw sheet to move you.
- Change your position every 1 to 2 hours to keep the pressure off any one spot.
- Sheets and clothing should be dry and smooth, with no wrinkles.
- Remove any objects such as pins, pencils or pens, or coins from your bed.
- DO NOT raise the head of your bed to more than a 30 degree angle. Being flatter keeps your body from sliding down. Sliding may harm your skin.
- Check your skin often for any areas of skin breakdown.
Take Care Of Your Skin
Taking care of your skin and doing regular skin checks are important in preventing pressure sores. Check your skin at least once a day for redness, changes in colour, blisters, bruises, cracked, scraped or dry skin. Closely inspect areas that are at especially high risk for pressure sores. The highest risk is where your bones are close to the surface and your skin is directly over bone. Use a mirror to inspect skin in hard-to-see areas or ask your caregiver to help you. If you notice a discolored area, stay off the area until it returns to normal skin colour.Keep your skin at the right moisture level, as damage is more likely to occur if your skin is either too dry or too moist. Use moisturising products to keep your skin supple and prevent dryness, but avoid massaging bony areas where the skin is too delicate. Immediately wash and dry skin and change clothing after any leakage of stool or urine . Avoid harsh soaps, skin agents with alcohol and antibacterial or antimicrobial soaps.
Don’t Miss: What Do You Do For A Bleeding Ulcer
How Can Pressure Injuries Be Prevented
The development of pressure injuries can be prevented through careful observation of the skin and frequent repositioning in those who canât turn themselves. Tips to prevent pressure injuries include:
- Keeping the skin clean and clear of bodily fluids.
- Moving and repositioning the body frequently to avoid constant pressure on bony parts of the body.
- Using foam wedges and pillows to help relieve pressure on bony parts of the body when turned in bed.
- Maintaining a healthy diet to avoid malnutrition and to assist in wound healing.
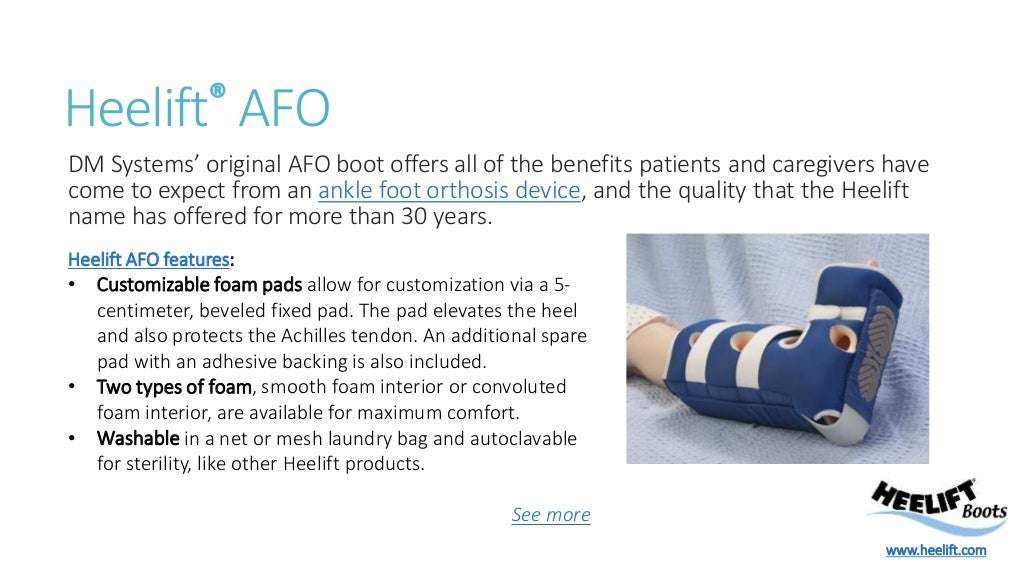
Reduce Friction And Shear
Friction is the rubbing of skin on an external surface, usually bed sheets. Friction to the most commonly affected areas can be reduced with protective devices. Heel and elbow cradles are typically made of egg-crate material and Velcro on.
Skin protecting dressings, such as films and thin hydrocolloid bandages can protect the skin from repeated friction but wont help reduce pressure.
The most important thing you can do to prevent injury from the friction is to make sure you dont create any yourself when youre repositioning your loved one. Use a draw sheet to help you lift your loved one off the bed when you lift and reposition.
Shear is created when the deeper fatty tissues and blood vessels are damaged by a combination of friction and gravity. The best way to avoid this type of injury is to avoid a semi-Fowler and upright position in bed. A semi-fowler position is where the head is raised less than 30 degrees and upright positions more than 30 degrees.
Now, you obviously cant avoid these positions all of the time. Many patients need to be semi-Fowler to help ease shortness of breath or prevent gastric reflux and all patients need to be in an upright position to eat safely.
To minimize the risk of shear injury in a semi-Fowler or upright position, take precautions to prevent your loved one from sliding down in bed. You can do this by raising the foot of the bed and propping the knees up with pillows.
Read Also: How Do You Cure Mouth Ulcers
How Can Friends And Family Help
Caregivers might sometimes provide too much help. For instance, they might turn someone over in bed although the person is actually still capable of turning over in bed themselves, perhaps with just a little assistance. It is better to only help as much as needed, so the person stays as independent as possible, helping to prevent pressure ulcers.
If you are caring for a family member at home or go to visit them in the hospital or at a nursing home, you can help them move short distances, for instance when taking a few steps to the table to sit down and eat.
If someone needs to lie in bed for a long time, a nursing care plan is usually made together with nursing professionals. This may include information such as how many times a day a person needs to be repositioned. It is important for everyone to make sure that the plan is followed properly. This also includes regularly changing diapers or incontinence pads.
You should tell the nurses or doctors immediately about any red or sore areas of skin. They can then take a closer look at the affected area. It is always important to take pressure off that part of your body.
Special Devices That Can Help You
In addition to turning and repositioning frequently, using a special surface to reduce or relieve pressure can help a great deal. The simplest of these is an egg crate mattress. Many hospice and home health agencies provide these free of charge but they are relatively inexpensive at your local department store.
If your loved one is spending a lot of time up in a chair, egg crate chair pads are also available. An egg crate surface helps distribute pressure more evenly, helping minimize the amount of pressure on one area.
A step up from the egg crate mattress is an air mattress overlay. This type of surface is placed on top of a mattress and typically alternates air pressure in various columns. When using an egg crate mattress or an air mattress overlay, its still important to maintain the turning schedule. These devices dont replace frequent repositioning.
The big guns of pressure-relieving devices are the fluidized air mattresses. These special mattresses contain silicone-coated glass beads that become fluid when the air is pumped through them. These mattresses do a wonderful job of relieving pressure but they have their downside.
The frame of the mattress makes transferring to and from bed difficult. And if the person wants to sit up in bed, a foam wedge would probably need to be used to help support their back. This mattress is really best suited for palliative care patients who are fully bed-bound, have severe pressure ulcers, and are in a lot of pain.
Recommended Reading: What To Avoid Eating With Ulcerative Colitis
What Causes Pressure Ulcers
There are two main causes for a pressure ulcer to develop. Either Pressure, caused by a concentration of body weight on one particular area over a period of time or something called Shearing. Shearing is caused by the skin being pulled in different/wrong/unusual directions. Actions that can cause this include
- Sliding or slumping down in a chair or bed
- Sitting in a chair thats the wrong size for you
- Sliding down the bed and then pushing yourself back up
- Rubbing and or massaging certain areas
- Badly fitting clothes or shoes
Leverage Our Entire Pressure Injury Prevention Portfolio:
Learn more about our comprehensive solution the perfect fit for pressure injury prevention.
Helping you get CLOSER TO ZERO pressure injury incidence.2
Leaf Healthcare, Inc. was acquired by Smith+Nephew in 2019. About Smith+Nephew.
Use of this Web site is governed by the Terms of Use, Copyright and Disclaimer and Privacy Policy. This website is intended for health care professionals in the United States only. Not all products referred to may be approved for use or available in all markets. Please consult your local Smith & Nephew representative for further details on products available in your market. The information provided is for informational purposes only and is not intended to be medical advice. It does not replace the professional training, experience, and knowledge of the healthcare provider responsible for patient care, who must base treatment upon the unique characteristics of each patient. Every patients case is unique and each patient should follow his or her doctors specific instructions.
For detailed product information, including indications for use, containdications, effects, precautions and warnings, please consult each products Instructions for Use prior to use.
Also Check: How To Reduce Bloating With Ulcerative Colitis
Sitting In A Chair Or Wheelchair
Most people shift around naturally when they are sitting down. But in the later stages of dementia, people are more likely to stay in one position for a long time. This can lead to pressure ulcers developing.
-
Encourage the person to change their position in the chair every 15-30 minutes while they’re sitting.
- Help them stand up and walk around at least every couple of hours if they are able.
- Ask the community nurse about pressure-relieving seat cushions.
- Ask about being referred to an occupational therapist, especially if the person needs a wheelchair or specialist seating.
Check The Skin For Signs Of Developing Pressure Sores Often
The skin should be checked frequently for the signs of developing pressure sores. A pressure sore may develop in less than a few hours.
For example, have you ever experienced increased soreness and redness on your buttocks while driving for more than an hour or two? If so, you developed a Stage I pressure sore, but your ability to move allowed you to recognize the pain and adjust your position to prevent it from progressing.
For some seniors, you must be the one to check and recognize the signs of a pressure sores development when performing perineal care, providing showers or performing other assessments of skin integrity. All such checks should be documented as well.
Also Check: What Are The Best Foods To Eat With An Ulcer
Grades Of Pressure Sores
If youve been bedridden for long enough, the areas of skin that are constantly in contact with the mattress or chair will start to discolour. This shows that the skin is in danger of ulcerating.
Pressure sores are graded to four levels, including:
- grade I skin discolouration, usually red, blue, purple or black
- grade II some skin loss or damage involving the top-most skin layers
- grade III necrosis or damage to the skin patch, limited to the skin layers
- grade IV necrosis or damage to the skin patch and underlying structures, such as tendon, joint or bone.
Myths About Turning And Repositioning
Beware of the half truth. You may have gotten hold of the wrong half
We dont call them Pressure Injuries for nothing. Complex as they can be in both etiology and treatment, one element is common to all of them: Pressure. Turning and Repositioning is the linchpin to any and all effective pressure injury prevention programs. But as important as it is, there are many common misconceptions about Turning and Repositioning that have become entrenched in healthcare. These misconceptions encumber our ability to sustain effective prevention policies and programs for pressure injury prevention. A more clear understanding of this critical intervention can have a profound influence to the success of any facilities pressure injury prevention efforts.
As a wound care and bedside nurse, I have studied Turning and Repositioning of the bedbound patient exhaustively. From patients body mechanics to the nursing process to equipment design and usage, I have come to understand that there are many aspects of Turning and Repositioning that are often overlooked or misunderstood.The reader might identify and agree with my assessments, or maybe feel a little provoked to dispute my assertions. Either way, I hope this commentary will challenge all who share similar aspirations to stop pressure injuries to pause, reflect and step out of the proverbial preconceived notions box to think about how we may better approach this most important nursing intervention:
Myth #4. Turning is easy
REFERENCES
Read Also: Does Turmeric Help With Ulcerative Colitis
What Are The 4 Stages Of Pressure Ulcers
You might hear medical staff refer to pressure ulcers in stages. Stage 1 is less severe, while an ulcer can progressively increase in severity to stage 4.
The 4 stages of pressure ulcers are:
|
Stage 1 |
The skin is red, but not broken. When you press the skin, it does not turn white. |
|
|
Stage 2 |
There is some damage to the outer layer of skin. The pressure ulcer looks like a shallow, open wound with a redish-pink centre. It can also look like a blister that may or may not have opened. |
|
|
Stage 3 |
There is full loss or damage of the skin. The wound looks quite deep but is still limited to the skin layers. |
|
|
Stage 4 |
There is full loss or damage of the skin it is deep and goes all the way to the underlying bone, tendon or muscle. |
Pep Prevention Emergency Project Preventive Measures For Pressure Ulcers
PEP was a patient care innovation project, which has developed a new process to effectively prevent pressure ulcers among patients in the risk zone. When initiatives are already implemented in the emergency room the entire hospital is affected since patients are often admitted from there to the various hospital wards. This also applies to other care services, such as assisted living facilities. The process is now implemented atthe hospital.
The emergency department at Karolinska University Hospital, Huddinge, run the project in collaboration with Mölnlycke. The process involves most services at the hospital, as well as five ambulance companies.
Project manager: Jenny Delin.
Also Check: Difference Between Ulcerative Colitis And Hemorrhoids
Don’t Miss: Food For Ulcer Patient In Nigeria
Causes And Prevention Of Pressure Sores
Pressure sores are wounds that develop when constant pressure or friction on one area of the body damages the skin. Constant pressure on an area of skin stops blood flowing normally, so the cells die and the skin breaks down.
Other names for pressure sores are bedsores, pressure ulcers and decubitus ulcers.