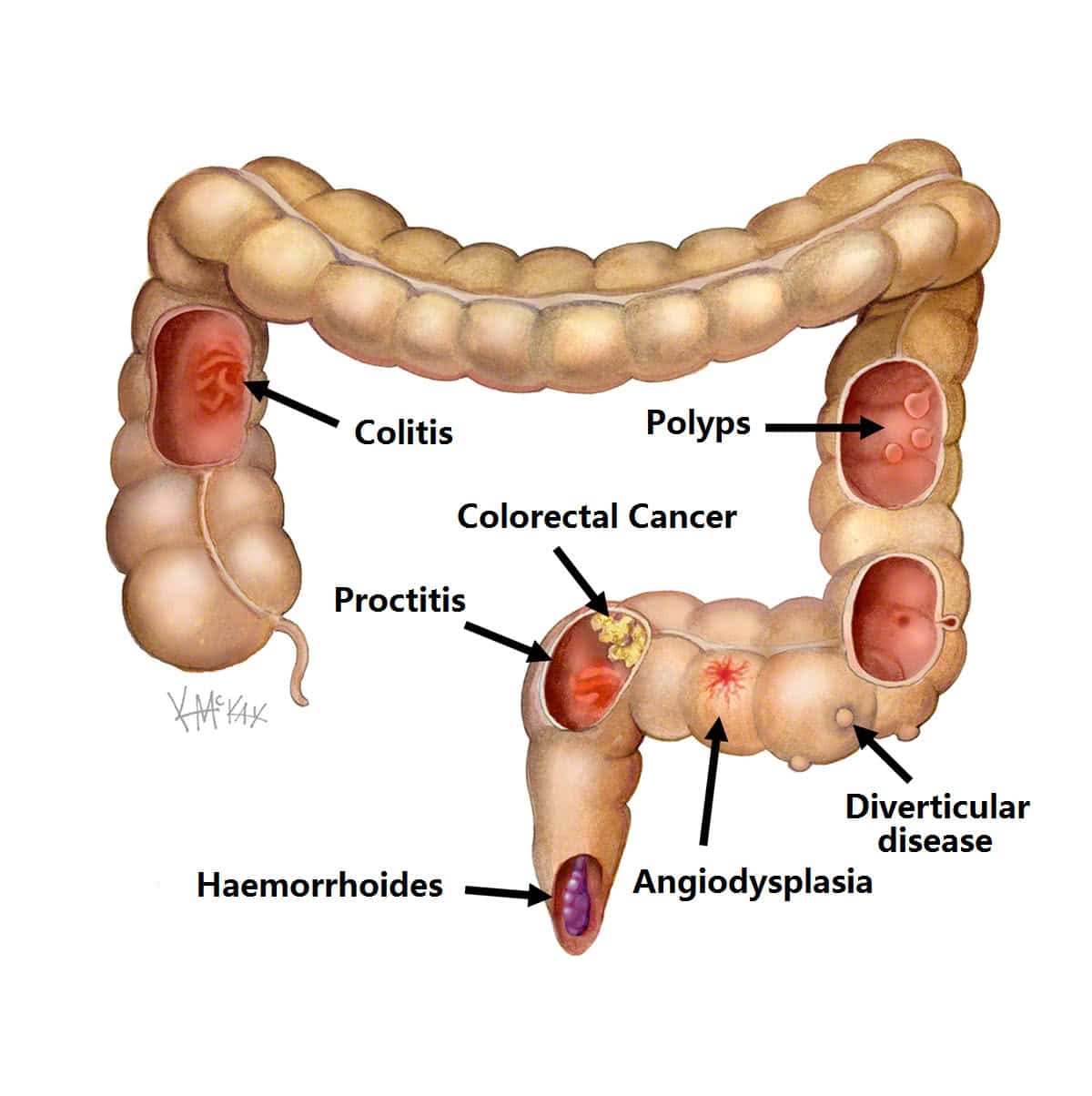
What Tests Are Done To Find Causes Of Blood In Stool
Your provider will check your pulse and blood pressure. He or she will probably also perform a rectal examination to look for hemorrhoids, fistulas, or fissures that could cause bleeding. You may need to have blood tests to check for anemia, clotting problems, and changes in your blood chemistry.
Your health care provider may recommend a colonoscopy.2 This procedure allows your provider to see inside your digestive tract and look for the source of bleeding. Colonoscopy is helpful for people with unexplained bleeding and bleeding that continues despite treatment. Colonoscopy is especially important if you have lost weight, are anemic, are older than 40, or have a family history of colorectal cancer.
Dont Miss: Does Alcohol Affect Ulcerative Colitis
What Was Causing The Blood Clot
Then, though, my leg swelled up and I could barely walk across my apartment. I knew that at this point something was wrong. When I contacted my doctor, he told me to go to the emergency room immediately because he suspected this could be a blood clot, which could be a side effect of the many medications I was on at the time, including mesalamine, a biologic, and prednisone. The doctor likely saved my life, as I was diagnosed with a blood clot in my leg, which could’ve become something worse.
Thankfully, this clot was caught in time so my treatment was relatively simple. I was given blood thinners in the hospital and then was told to continue these for 3-6 months while following up with a hematologist. The only negative to the blood thinners was the possibility that my rectal bleeding might also increase. Luckily, if it did increase, it was not by a noticeable amount.
When I met with the hematologist, we discussed the possible causes of my blood clot. She explained that I did have some risk factors. One was that I had been on oral birth control for about a decade and that wed gone on a long 10- or 11-hour drive. Although she also said that blood clots due to driving are less common than those due to flying.
Tailoring Vte Prophylaxis In Ibd: Future Directions
Clinical trials are needed to confirm the effectiveness and safety of thromboprophylaxis in patients with IBD, particularly in ambulatory patients with active disease and in those recently discharged from hospital. Trials would be challenging to conduct because absolute event rates of thrombosis are low, but novel approaches to VTE trial design using composite endpoints will assist planning. Surrogate markers of thrombogenic potential, including calibrated automated thrombinography and thromboelastography, might be used in proof of concept studies,, or as secondary endpoints.
Better methods of measuring thrombotic risk are crucial to guiding appropriate thromboprophylaxis in patients with IBD. Mechanisms of thrombosis in patients with IBD need to be understood, so that biomarker assays of prothrombotic potential can be evaluated. Incorporating sensitive coagulation assays with thrombotic biomarkers and clinical risk indices into clinical practice should help guide clinicians.
VTE is a life-threatening extraintestinal manifestation of IBD mitigated by appropriate thromboprophylaxis. Essential to reducing the risk of VTE in patients with IBD is timely and effective management of disease flares, and clinician awareness and adherence to thromboprophylaxis guidelines. Outpatients with active disease and patients after discharge from hospitalisation deserve particular attention. Prevention of VTE is part of managing the manageable to reduce the burden of IBD.
Read Also: Do Tums Help Ulcerative Colitis
Abnormalities Of The Immune System In Ibd
Anti-phospholipid antibodies are a group of pro-thrombotic antibodies including lupus anticoagulant , anti-cardiolipin antibodies and anti-beta-2-glicoprotein-I . APLA may be associated with both venous and arterial thrombosis. IBD patients seem to have higher rates of aCL and anti-beta-2-GPI positivity – with an incidence of 20%-30% for the first and 9% for the latter – compared to general population, but the real association with thrombosis in IBD is still unclear . In fact, LAC, aCL and anti-beta-2-GPI levels were similar in IBD patients with or without history of VTE .
In IBD patients anti-PS antibodies have also been detected, which may cause a reduction in the natural anticoagulant potential but there is still not enough evidence that they play any role in thrombotic risk .
Mechanisms Of Increased Thrombotic Risk In Ibd
The magnitude of the risk of VTE in IBD is distinct from other chronic inflammatory or bowel disorders, such as rheumatoid arthritis and coeliac disease, implicating disease-specific factors in the pathogenesis of VTE in IBD ., There is no evidence that hereditary thrombophilias are more common in patients with IBD. Acquired haemostatic alterations are likely to play the most significant role, particularly during the active phase of disease. Inflammation may drive a hypercoagulable state through activation of the coagulation cascade, coupled with promotion of platelet aggregation and impairment of anticoagulant or fibrinolytic mechanisms., Neutrophil extracellular traps, which are extracellular DNA fibres produced during inflammation, link inflammation and thrombosis, as they have been shown to stimulate thrombogenesis and are abundant in thrombi in animal models of VTE.
Don’t Miss: Can You Donate Blood If You Have Ulcerative Colitis
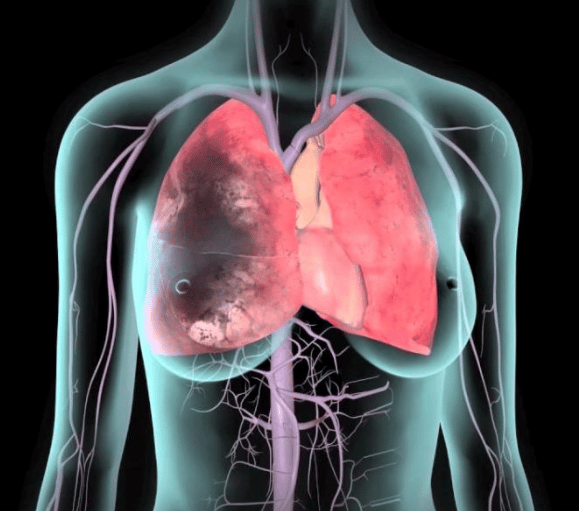
What Is Venous Thromboembolism
Deep Vein Thrombosis and Pulmonary Embolism are often underdiagnosed and serious, but preventable medical conditions.
Deep vein thrombosis is a medical condition that occurs when a blood clot forms in a deep vein. These clots usually develop in the lower leg, thigh, or pelvis, but they can also occur in the arm.
It is important to know about DVT because it can happen to anybody and can cause serious illness, disability, and in some cases, death. The good news is that DVT is preventable and treatable if discovered early.
Venous thromboembolism , a term referring to blood clots in the veins, is an underdiagnosed and serious, yet preventable medical condition that can cause disability and death.
The American Society of Hematology recognizes the need for a comprehensive set of guidelines on the treatment of VTE to help the medical community better manage this serious condition. In partnership with the McMaster University GRADE Centre, ASH brought together experts to address this challenge, including hematologists, other clinicians, guideline development specialists, and patient representatives. In November 2018, ASH announced the results of their collective efforts the 2018 ASH Clinical Practice Guidelines on Venous Thromboembolism. Access the new guidelines.
How To Use Suppositories
Your doctor or pharmacist will tell you how many suppositories to use each day. Some types you use once a day before you go to bed, and others you use several times a day with the last dose before you go to bed. Use them after you do a poo.
Try not to do a poo for at least an hour after using a suppository. This gives the medicine time to work.
Recommended Reading: What Cream Is Good For Leg Ulcers
Reducing Blood In Stools
prebiotic supplement may help reduce bloody stools and other symptoms of UC.
Participants taking the prebiotics supplement experienced significantly decreased abdominal pain and cramping. They also reported reduced nausea, vomiting, diarrhea, and blood in stools, although these effects were not statistically significant.
The study was small, so more research is needed to determine the best way to reduce blood in stools.
If a person frequently has bloody stools, a doctor may prescribe iron supplements to help prevent anemia.
Management Of Vte In Ibd: Guidelines Practice And Evidence
Consensus recommendations from international organisations support VTE prophylaxis for hospitalised patients with active IBD.,, Data from hospitalised general medical inpatients show that the risk of VTE is significantly reduced by prophylaxis with low molecular weight heparin or fondaparinux. Thromboprophylaxis is safe in patients with IBD, with no significant difference in rates of major bleeding between those who do and do not receive thromboprophylaxis , even when there is rectal bleeding during a flare.,
It is therefore notable that surveys suggest that up to 55% of gastroenterologists are unaware of VTE guidelines for patients with IBD and 65% may not give pharmacological VTE prophylaxis to patients hospitalised with acute severe colitis. There is particular inconsistency in administration of VTE prophylaxis for patients with quiescent IBD admitted to hospital for other reasons. Greater awareness of the risks of VTE in IBD and better adherence to VTE guidelines were associated with IBD specialists , those affiliated to an academic hospital and those recently qualified .
Recommended Reading: Interventions To Prevent Pressure Ulcers
Q: What Is Ibd And What Does It Involve
There are two main types of IBD: ulcerative colitis and Crohns disease. Both conditions cause chronic inflammation and damage within the gastrointestinal tract. The GI tract typically helps us digest food, absorb nutrients, and get rid of waste, but the inflammation from IBD interferes with these functions. With Crohns disease, the inflammation can affect any part of the gut from the mouth downwards. In UC, the inflammation is limited to the large intestine the colon.
Historically, IBD was thought to mostly affect people of European ancestry, with the highest risk seen in the Ashkenazi Jewish population . Now were seeing more IBD in African American, Hispanic, and Asian populations.
IBD can occur at any age but is most commonly diagnosed before age 35. At that time of life the teenage years and early adulthoodpeople experience a lot of personal, social, and professional development, and IBD can be devastating. Symptoms can include stomach pain, diarrhea, rectal bleeding, and fatigue, to name a few and a lot of our patients have symptoms outside the gut, too. We know that if we dont control the inflammation and get on top of these symptoms, patients can have a very poor quality of life.
How Can I Prevent Clots
If you’re in the hospital, you may get a drug called heparin, which will help prevent clots. Your doctor may even talk to you about how to take it at home during severe flare-ups, since that’s when you’re most at risk.
It also helps to:
Work with your doctor to control IBD as best as you can. Fewer flare-ups means less inflammation, which lowers your risk.
Keep as active as you can. When you don’t move your body, your blood flow slows down. And slower-moving blood is more likely to clot.
Make sure you get all the nutrients you need. It can be a challenge with IBD, but it’s an important step.
Show Sources
You May Like: Generic Drugs For Ulcerative Colitis
How Would I Know If I Had A Clot
It depends where you get it.
Symptoms in your legs. Be on the lookout for:
- Pain or tenderness in the back of your lower leg, which might feel like a cramp
- Red or bluish color to your skin
- Swelling in your lower legs, especially when it’s more in one leg than the other
Swelling in the legs can be tricky because other problems linked to IBD, like low protein, can also cause it. Still, if you have symptoms of a clot, it’s best to call your doctor right away, even if you’re not sure.
Symptoms in your lungs. You may notice:
- You cough for no reason, maybe with bloody mucus
- Your heart beats faster than normal
- You get a sharp, stabbing pain in your chest that may get worse when you take a deep breath
- You feel short of breath
If you have these symptoms, get help right away. A clot in your lungs is an emergency.
Rivaroxaban : A Deep Dive
The North American Thrombosis Forum is a 5013 nonprofit organization incorporated by the Commonwealth of Massachusetts. NATF is dedicated to improving the lives of those affected by blood clots and related diseases. Through our comprehensive resources and innovative programming, we strive to educate patients and healthcare providers about thrombosis and its complications.
NATF provides the information and materials on this site for general information purposes only. You should not rely on the information provided as a substitute for professional medical advice, care, or treatment. This site is not designed to and does not provide medical advice, professional diagnosis, opinion, treatment, or services to you or any individual. If you believe you have a medical emergency, call 911 immediately.
Headquarters
Don’t Miss: Biological Medicine For Ulcerative Colitis
Impact And Manifestations Of Thrombosis In Patients With Ibd
VTE occurs in patients with IBD at a younger age than the general population, and may lead to prolonged hospitalisation, impaired quality of life and increased healthcare utilisation., IBD has also been shown to be a risk factor for recurrent VTE, with an adjusted recurrence rate 2.5 fold that of the general population 5 years after cessation of anticoagulation for a first VTE. Mortality rates following VTE amongst patients with IBD are considerable, ranging from 18 to 22%., Perhaps more striking is evidence that mortality rates in hospitalised patients with IBD and VTE are 2.1 fold-higher than those of patients with VTE, but without IBD. This study found that IBD-related bowel surgery had the greatest impact on inpatient mortality associated with VTE , which is incongruous with the younger age and low comorbidity of patients with IBD. Although unable to define the type of VTE, the data suggest that VTE in this group may be more severe or carry a higher risk of pulmonary embolism.
Open Access License / Drug Dosage / Disclaimer
This article is licensed under the Creative Commons Attribution-NonCommercial 4.0 International License . Usage and distribution for commercial purposes requires written permission. Drug Dosage: The authors and the publisher have exerted every effort to ensure that drug selection and dosage set forth in this text are in accord with current recommendations and practice at the time of publication. However, in view of ongoing research, changes in government regulations, and the constant flow of information relating to drug therapy and drug reactions, the reader is urged to check the package insert for each drug for any changes in indications and dosage and for added warnings and precautions. This is particularly important when the recommended agent is a new and/or infrequently employed drug. Disclaimer: The statements, opinions and data contained in this publication are solely those of the individual authors and contributors and not of the publishers and the editor. The appearance of advertisements or/and product references in the publication is not a warranty, endorsement, or approval of the products or services advertised or of their effectiveness, quality or safety. The publisher and the editor disclaim responsibility for any injury to persons or property resulting from any ideas, methods, instructions or products referred to in the content or advertisements.
Also Check: Extra Virgin Olive Oil And Ulcerative Colitis
How Is It Evaluated And Diagnosed By Doctors
Your health care provider will evaluate rectal bleeding by asking questions, performing a physical exam, and doing some tests.
Your provider may ask questions such as:3,4,8
- What are your bowel movements like?
- Have you had any recent changes in bowel habits?
- Are your stools black or bloody? How often does this happen?
- Have you noticed blood on the toilet paper?
- Have you vomited recently? What did it look like?
- Have you had a recent colonoscopy?
- Have you had any recent trauma to the abdomen or rectum?
- What medications are you taking?
- Do you have a history of digestive or blood diseases?
- Have you been treated for prostate or pelvic cancer?
- Has anyone in your family had colon cancer?
- Have you experienced changes in weight recently?
Your health care provider may want to look at your stool.4 If you are in the hospital, you may be asked to use a special toilet or bedpan. If you are at home, your provider will instruct you on how to collect a sample.
Blood Clots In Stool: Causes Hematochezia Is Commonly Associated With Lower Gastrointestinal Bleeding From Last 1 Month I Have Spotted Little Drops Of Blood In My Stool Severe Bleeding Meaning Possible Symptom For Ulcerative Colitis
Blood in stool is a possible symptom for ulcerative colitis and Crohns disease, White blood cells in your stoolBlood Clots and Ulcertive ColitisBlood clot complications as a result of ulcerative colitis symptoms and or medications, and what to know
Estimated Reading Time: 7 minsClick to view2:17Other life-threatening complications that may develop due to ulcerative colitis include tears in the colon, It can be either acute or chronic and sometimes persistent, Symptoms beyond the intestineAuthor: Lisa Marie Conklin
Also Check: Black Tarry Stools Ulcerative Colitis
Also Check: Air Mattress For Pressure Ulcer Prevention
How Are Ulcerative Colitis And Colitis Different
A key difference is what triggers colitis. For instance, IBD is usually an autoimmune issue. Thatâs when your immune system attacks healthy tissue in your body. Other kinds of colitis can be the result of outside factors, such as germs or medical treatments.
People with UC or other kinds of IBD may also have inflammatory symptoms alongside bowel problems, including:
But those arenât the only distinctions. Hereâs a breakdown by colitis type:
Ulcerative colitis . This type of IBD causes sores and constant inflammation in the inner lining of your large intestine. UC often starts in the rectum and extends through the left side of your colon. But some people have colitis throughout most or all of their colon. Thatâs called extensive colitis or pancolitis.
Crohnâs colitis. This is a feature of Crohnâs disease, another type of IBD. Crohnâs can impact any part of your gastrointestinal tract â thatâs your mouth to your . Unlike UC, you may have healthy tissue in between spots of inflammation. Crohnâs disease can also affect many layers of your GI tract.
Microscopic colitis. This is another type of IBD. Itâs not related to ulcerative colitis or Crohnâs disease, but itâs associated with other autoimmune diseases. Like the name suggests, your doctor has to use a microscope to see any evidence of this kind of colitis.
There are two main forms:
Some experts think collagenous and lymphocytic colitis may be different phases of the same condition.