What Sets Them Apart
There are three key differences:
1. Location.
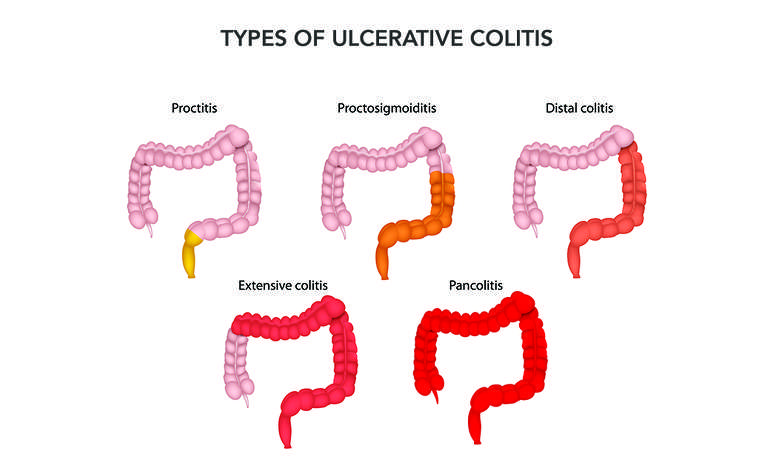
Ulcerative colitis affects only the large intestine.
But in Crohnâs disease, inflammation can appear anywhere in the digestive tract, from the mouth to the anus.
2. Continuous inflammation.
People with Crohnâs disease often have healthy areas in between inflamed spots. But with ulcerative colitis, there are no healthy areas in between inflamed spots.
3. Which layers are affected.
Because Crohnâs disease affects more of the GI tract, it can cause some problems that doctors don’t usually see in people who have ulcerative colitis. For instance:
- Mouth sores between the gums and lower lip, or along the sides or bottom of the tongue.
- Anal tears , ulcers, infections, or narrowing.
Confused About Ischemic Colitis And Colitis
Quincy AdamUC Learn
Ulcerative Colitis is the chronic irritation and swelling of the large intestine with small sores called ulcers, and usually affects younger people.2
Ischemic colitis occurs most often in people aged 60 and older and the inflammation and injury in the colon is caused by not enough blood flow to the large intestine.2 For many people, it is mild to moderate and not a medical emergency, and can be treated with antibiotics and resting the large intestine . However, when severe, it may come on suddenly and result in serious problems if left untreated.2
Learn more about the symptoms of ischemic colitis:www.mayoclinic.org
The intestines perform a variety of essential tasks in your body from absorbing nutrients from food to passing wastes from the body. These activities require oxygen and other vital substances that are supplied by your blood flow. The blood supply to the large intestine keeps it performing its important tasks and keeps the tissue alive.3 If there is a blockage, the blood supply is reduced and without oxygen from the blood, the tissues in your colon can become damaged or die quickly.3
This may lead to some very serious complications that may require surgery: 4
- gangrene
- perforation in your intestine
- bleeding
How Is Ischemic Colitis Diagnosed And Treated
Your doctor would run several diagnostic tests, and if you have a very mild case, you may just be closely monitored and take antibiotics and a liquid diet at home. If chronic and mild to moderate, you doctor may require you to be hospitalized and treated with antibiotics and IV fluids, to give the bowel a rest from food and drink.7
- Imaging such as an ultrasound or CT scan in order to see your blood vessels and intestines.
- Angiogram is another imaging test that allows your doctor to see inside your arteries and where there is blockage.
- Stool sample or colonoscopy.
- Blood tests can also check your white blood cell count when it is high it can mean you have a medical emergency that may require medications or surgery to remove a blockage or any dead tissue.
- Surgery is only necessary when the ischemic colitis is acute and severe and there is damage to the colon.
Read Also: Is Okra Good For Ulcerative Colitis
Main Difference Colitis Vs Ulcerative Colitis
Colitis and ulcerative colitis are two medical conditions which affect the colon. These two terms often used interchangeably since they share similar signs and symptoms. But, it is important to distinguish the difference between them in order to make an accurate diagnosis and treatment. The main difference between colitis and ulcerative colitis is that ulcerative colitis is one form of colitis which results in the chronic inflammation of colonic mucosa and rectum giving rise to ulceration and bleeding.
1. What is Colitis ? Causes, Signs and Symptoms, Diagnosis, and Treatment
2. What is Ulcerative Colitis? Causes, Signs and Symptoms, Diagnosis, and Treatment
3. What is the difference between Colitis and Ulcerative Colitis?
When Surgery Is Needed
If medication isn’t reducing the inflammation and IBD progresses, surgery may be needed. This is where people with ulcerative colitis tend to fare better.
If the colon gets bad enough in ulcerative colitis, its removed and replaced with an internal pouch, which functions like a colon, says Cohen. According to the Mayo Clinic, colectomy surgery whether partial or full usually requires additional procedures that reconnect the remaining portions of the digestive system so they can still rid the body of waste.
However, things are looking up. A study published in December 2019 in the Journal of Gastrointestinal Surgery found that due to advances in medicine and medical care for IBD patients over the past decade, the number of hospitalized patients with ulcerative colitis who require a colectomy decreased by nearly 50 percent between 2007 and 2016.
According to the Crohns and Colitis Foundation, proctocolectomy with ileal pouchanal anastomosis usually called J-pouch surgery is the most common surgery performed on people with UC who have not responded to medication. Surgeons remove the rectum and colon and then create a temporary opening in the abdomen, called a loop ileostomy, which will allow waste to move from the small intestine into an ostomy bag that sits outside the body while the digestive system heals from the surgery. In some cases a stoma, or permanent opening in the abdomen that funnels waste into an external bag, is required, notes the Mayo Clinic.
Don’t Miss: How Can You Cure An Ulcer
Layers Of The Bowel Wall
The walls of your bowel have layers. The inner layers take in nutrients from food. The outer layers help move food through the gut and waste out of the body.
In Colitis, theres inflammation and swelling of the inner layer of the bowel wall. This can cause bleeding. More mucus may be produced by the inner layer of the bowel wall. Ulcers develop on the inner layer as the condition gets worse, but they can also go as the condition gets better.
The inflammation in Colitis affects how your body digests food, absorbs nutrients and gets rid of waste.
Everyone experiences Colitis differently. When youre having symptoms, its known as active disease, a flare-up or relapse. Symptoms may be mild or severe and are likely to change over time.
Your symptoms may vary depending on where Colitis is active in your bowel and how severe it is. Find out more in the section Types of Colitis.
The most common symptoms are:
Andy
Living with Colitis
Whats The Difference Between Ulcerative Colitis And Crohns Disease
UC and Crohns disease are the most common forms of IBD. Both conditions are thought to be the result of an overactive immune system.
They also share many symptoms, including:
- cramps
- diarrhea
- fatigue
However, UC and Crohns disease do have distinct differences. Understanding the key differences between them can help you obtain a proper diagnosis.
Location
These two conditions affect different portions of the GI tract.
Crohns disease may affect any part of the GI tract, from the mouth to the anus. Its most often found in the small intestine. UC only affects the large intestine and rectum.
Response to treatment
Similar medications are prescribed to treat both conditions. Surgery is also a treatment option. Its a last resort for both conditions, but it can be a cure for UC, whereas its only a temporary therapy for Crohns.
Don’t Miss: Sand Beds For Pressure Ulcers
Daily Life For People With Ibd
People with IBD lead useful and productive lives, even though they need to take medications. When they are not experiencing a flare-up of their disease, they feel quite well and are often free of symptoms.People with IBD can marry, enjoy sexual activity and have children. They can hold down jobs, care for families and enjoy sport and recreational activities.Even though there is currently no cure for IBD, medical therapy has improved the health and quality of life of most people with Crohns disease and ulcerative colitis. Research underway today may lead to further improvements in medical and surgical treatment, and even a cure.
Who Gets Ulcerative Colitis And What Causes It
Colitis can develop at any age, but usually first appears in people aged 15 to 30.
Experts are not sure why UC or Crohn’s disease occurs in some people. It may be due to a combination of genetic, environmental and infectious factors that cause a fault in the immune system leading to inflammation of the bowel.
Recommended Reading: Tnf Alpha Inhibitors For Ulcerative Colitis
Crohns & Colitis Uk Local Networks
Our Local Networks of volunteers across the UK organise events and provide opportunities to get to know other people in an informal setting, as well as to get involved with educational, awareness-raising and fundraising activities. You may find just being with other people and realising that you are not alone can be reassuring. Families and relatives may also find it useful to meet other people with Crohn’s or Colitis. All events are open to members of Crohns & Colitis UK
What Causes Ulcerative Colitis
Researchers think the cause of ulcerative colitis is complex and involves many factors. They think its probably the result of an overactive immune response. The immune systems job is to protect the body from germs and other dangerous substances. But, sometimes your immune system mistakenly attacks your body, which causes inflammation and tissue damage.
Also Check: What’s The Signs Of An Ulcer
Crohns Disease Vs Ulcerative Colitis: Differences In Symptoms Causes And Treatment
Crohns disease and ulcerative colitis are part of the group of conditions known as inflammatory bowel diseases . Prior to the 20th century, before the rise of hygiene and urbanization, inflammatory bowel disease was quite rare. Currently, IBD is found in developed countries and is believed to be caused by a lack of germ resistance development although the exact cause is still unknown.
For those living with IBD, their immune system mistakes food and bacteria in the gastrointestinal tract for an allergen or foreign substance, so it sends out cells to destroy it. The result of these attacks is chronic inflammation.
Although the exact causes of Crohns disease and ulcerative colitis are unknown, genetics and environmental factors are believed to play a role. Crohns disease and ulcerative colitis are often interchanged for one another, but we will outline the differences between the two, including symptoms, causes, and treatments in order to provide you with a better understanding of either condition. Continue reading
How Can I Tell If I Have Ulcerative Colitis Or Crohns Disease
Its important that you, your healthcare provider, and a GI specialist work together closely to figure out whats causing your symptoms. This is especially important since the symptoms of Crohns disease and ulcerative colitis can be similar. Your providers may check blood work and a stool sample. To get an accurate diagnosis, your GI specialist may do a colonoscopy, where a camera is pushed into the colon. Your provider will look at the inside of the colon and take tissue samples, which are important for making the right diagnosis. Your providers might get a CT scan or an MRI of your abdomen to check for complications related to your condition.
Read Also: How To Ease An Ulcer
Actions For This Page
- Crohns disease and ulcerative colitis are collectively known as inflammatory bowel disease .
- Crohns disease can appear in any part of a persons digestive tract from mouth to anus.
- Ulcerative colitis is located only in a persons large bowel .
- Diet and food allergies do not cause IBD.
- Medications help manage the symptoms of IBD.
- People with IBD can lead useful and productive lives.
- Some dietary changes can help you manage symptoms of IBD and allow medications to work better.
- Always talk with your doctor, healthcare specialist or dietitian before changing your diet. Arrange an emergency plan of action with your doctor, including after-hours phone numbers.
Is There Such A Thing As An Ulcerative Colitis Diet Or A Crohns Disease Diet
What kind of food should I eat for ulcerative colitis? Should I follow a Crohns disease diet? These are questions that Dr. Blazora hears often from people with IBD. Diet is always a hot topic thats probably one of the first questions people ask me about after theyve been diagnosed, she says.
In short, diet mattersbut it depends on your personal triggers. If youre experiencing a Crohns or ulcerative colitis flare-up, dietary changes may help. We may tell you to take on a low-fiber diet or avoid lactose or caffeinated beverages or anything that can stimulate the bowel to produce more bowel movements, but its not going to change the course of the disease itself, Dr. Balzora says. That said, a 2021 study published in the journal Gastroenterology found that eating a Mediterranean style diet , and avoiding processed foods and foods high in sugar could be beneficial.7
However, while tweaking your diet may help you feel more comfortable, it may not get to the root of the issue. Its the medications that turn the tide, Dr. Balzora stresses. They really decrease the inflammation as opposed to diet.
Recommended Reading: Bone Broth For Stomach Ulcer
Ulcerative Colitis And Colonoscopy
Doctors can use a colonoscopy to diagnose UC or determine the severity of the condition.
Before the procedure, a doctor will likely instruct you to reduce solid foods and switch to a liquid-only diet. Then youll fast for a period of time before the procedure.
Typical colonoscopy prep involves taking a laxative the evening before the procedure, too. This helps eliminate any waste still in the colon and rectum. Doctors can examine a clean colon more easily.
During the procedure, youll lie on your side. Your doctor will give you a sedative to help you relax and prevent any discomfort.
Once the medication takes effect, the doctor will insert a colonoscope into your anus. This device is long and flexible so it can move easily through your GI tract. The colonoscope also has a camera attached so your doctor can see inside the colon.
During the exam, the doctor will look for signs of inflammation and check for precancerous growth called polyps. The doctor may also perform a biopsy. The tissue can be sent to a laboratory for further examination.
If youve been diagnosed with UC, a doctor may conduct periodic colonoscopies to monitor inflammation, damage to your intestines, and healing progress.
These symptoms are sometimes associated with UC complications.
If you havent been diagnosed with UC, see a doctor if you experience multiple symptoms of the condition. They can help determine whether you may have UC or another bowel disease.
Ulcerative Colitis In Children
According to one study of IBD in the United States, 1 in 1,299 children between ages 2 and 17 years old were affected by the condition in 2016. Crohns disease was twice as common as UC, and boys were more likely to have IBD than girls.
For children with IBD, a diagnosis is more likely after 10 years old.
UC symptoms in children are similar to symptoms in older individuals. Children may experience bloody diarrhea, abdominal pain and cramping, and fatigue.
In addition, they may experience issues compounded by the condition, such as:
- anemia due to blood loss
- malnutrition from poor eating
- unexplained weight loss
UC can have a significant effect on a childs life, especially if the condition isnt treated and managed properly. Treatments for children are more limited because of possible complications. For example, medicated enemas are rarely used as a treatment method in children.
However, children with UC may be prescribed medications that reduce inflammation and prevent immune system attacks on the colon. For some children, surgery may be necessary to manage symptoms.
If your child has been diagnosed with UC, its important that you work closely with their doctor to find treatments and lifestyle changes that can help. Check out these tips for parents and children dealing with UC.
You May Like: Stage 2 Pressure Ulcer Treatment Cream
Symptomatic Differences Between Crohns Disease And Ulcerative Colitis
There are some subtle differences in symptoms of Crohns disease and ulcerative colitis. In Crohns disease rectal bleeding is less common, whereas in ulcerative colitis, bleeding from the rectum is much more common. In Crohns disease, continuous abdominal pain is more common and perianal problems such as fistulas, anal sores and skin tags, can occur. In contrast, people living with ulcerative colitis usually have intermittent pain coinciding with bowel movements. Perianal issues are uncommon in ulcerative colitis.
Clinical Trials Updates
In My Shoes: 24 Hours With Crohns Or Colitis App
In My Shoes is an immersive experience that allows anyone to find out first-hand what its like to have Colitis.
From low energy levels to managing pain, from rushing to the toilet to juggling work and a social life, the app will allow friends, family and anyone you want, to see first-hand how the condition can affect every part of your body, and every aspect of your life.
We have information for friends and family, employers, and colleagues. Find all our information online.
We have around 50 Local Networks across the UK that bring local people affected by Crohns and Colitis together. They are run by volunteers and host a range of events, from educational talks to socials. Check our website or call our Helpline to find your nearest Local Network.
Recommended Reading: Can Diverticulitis Cause Ulcerative Colitis
How Is Microscopic Colitis Diagnosed
During a colonoscopy, a biopsy will be taken and examined. Even if the lining of the colon looks normal, it is important to remove tissue samples for a microscopic analysis. Without these diagnostic steps, it could take weeks, months, or even years to discover the reason for the chronic diarrhea.
Once the biopsy samples are examined under a microscope, various features may reveal the source of the inflammation and pinpoint the diagnosis even further. There results of the biopsy may show the following:
- In patients with collagenous colitis, a biopsy of the colon shows inflammation and thickened tissue made from a protein called collagen. The appearance of this tissue may vary, so it is important to look at several different samples.
- In those with lymphocytic colitis, a biopsy of the colon shows an increased number of special white blood cells . A thickened band of collagen band can be seen on the biopsy, as patients can often exhibit features of both collagenous and lymphocytic colitis.