How Do Doctors Treat Ulcerative Colitis
Doctors treat ulcerative colitis with medicines and surgery. Each person experiences ulcerative colitis differently, and doctors recommend treatments based on how severe ulcerative colitis is and how much of the large intestine is affected. Doctors most often treat severe and fulminant ulcerative colitis in a hospital.
With Many Options Available It’s Important To Work With Your Doctor To Try New Treatments
Inflammatory bowel disease , which includes Crohns disease and ulcerative colitis , is a condition that involves inflammation of the digestive tract. In recent years, treatment options for IBD have rapidly expanded. The goal of these newer treatments is to improve control of inflammation in the gut, which can greatly improve patients quality of life.
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Don’t Miss: What Cream Is Good For Leg Ulcers
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
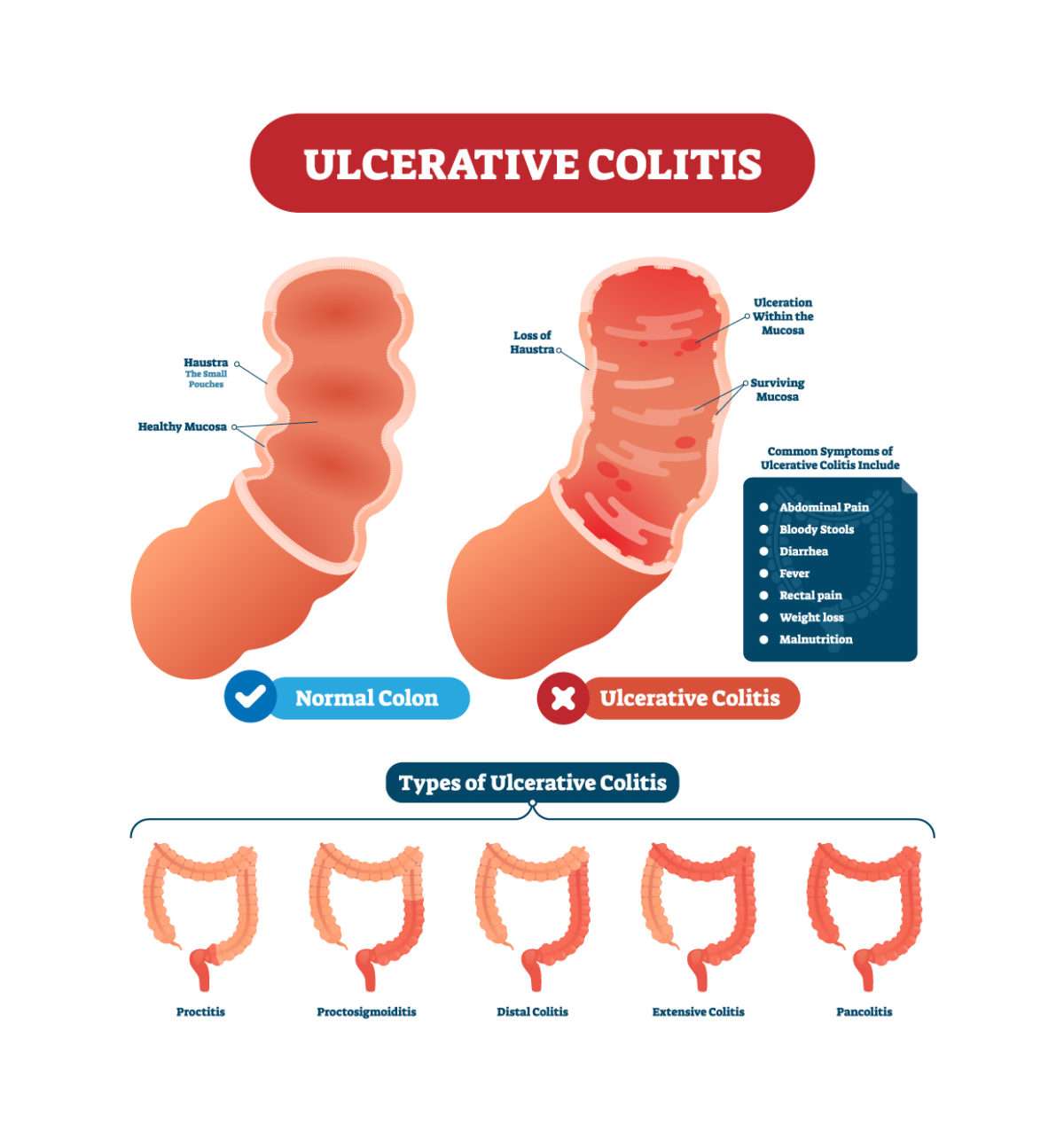
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Evidence For Antibiotics In Ulcerative Colitis
Induction of remission in active ulcerative colitis
A number or RCT and uncontrolled studies have been reported on antibiotics for induction of remission in chronically active and acute severe colitis . Multiple different antibiotic combinations were trialed with very different outcomes reported, ranging from dramatic induction of complete remission, through to no response.
Two meta-analyses demonstrate overall higher remission rates with antibiotics compared to placebo . Considering the diverse range of antibiotics trialed, different methods of administration and course length, and the vastly divergent responses, interpretation of the data is limited, and recommendations for clinical practice is difficult to formulate. Indeed it is unclear whether it is appropriate to pool studies with a diverse assortment of antibiotics.
Interestingly, upon independent analysis of the trials a striking contrast is revealed. Those trials in which antibiotics were administered orally seemed to have a greater response than those in which they were administered intravenously. It may be that the effect of the antibiotics is by way of a local luminal effect, possibly effecting beneficial change on the microbiome, or as has been suggested, by direct effect on a particular pathogen .
You May Like: Best Antibiotic For Resistant Uti
Recommended Reading: How To Get Rid Of Peptic Ulcer
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
You May Like: How To Calm An Ulcer
The Role Of The Microbiome In Ibd
Gut flora comprises an enormously complex microenvironment, with the microbial genome outnumbering the human genome by at least an order of magnitude . The majority of gut microbiota has never been cultured, and the advancement in our understanding of its complex role has only begun to flourish with the development of newer culture-independent technologies. Adding to the complexity of this microenvironment is the uncertain role of other members of this microbial community including fungi and bacteriophages.
Indirect support for the role of gut flora in IBD pathogenesis is provided by fecal stream diversion improving disease activity in CD, with restoration of fecal stream inducing recurrence. This does not occur, however, when ileostomy effluent is filtered to remove bacteria prior to reintroduction . Ileal microflora undergoes significant expansion on restoration of contiguity with colonic remnant, however the microbial pattern in patients with CD varies significantly from that of patients without CD upon restoration of fecal flow, with significantly higher counts of E coli and bacteroides in patients with CD, as compared to higher counts of bifidobacteria and ruminococci amongst controls .
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Recommended Reading: Best Antibiotic For Nasal Infection
You May Like: Ulcer On White Of Eye
Some Ingredients In Supplements
Some supplements are very beneficial for people with UC. These include calcium, folic acid, and iron. However, some ingredients in supplements may worsen the symptoms of UC.
According to the Crohns and Colitis Foundation, people should avoid supplements that contain:
All of these may aggravate a persons UC symptoms, particularly during a flare-up.
The Crohns and Colitis Foundation also adds that people should avoid taking any supplements on an empty stomach.
A person should check with a medical professional before taking any supplements, including herbal supplements, over-the-counter medications, and complementary therapies.
Recommended Reading: Antibiotics For Colitis Flare Up
What Is Pseudomembranous Colitis
Pseudomembranous colitis is inflammation of the large intestine. In many cases, it occurs after taking antibiotics. Using antibiotics can cause the bacterium Clostridium difficile to grow and infect the lining of the intestine, which produces the inflammation. Certain antibiotics, like penicillin, clindamycin , the cephalosporins and the fluoroquinolones, make C. diff overgrowth more likely.
You May Like: Early Symptoms Of Stomach Ulcer
Antibiotics To Avoid When You Have Crohns Disease
If you have Crohns disease, your doctor may prescribe antibiotics for abscesses and fistulas. The most common prescriptions for these complications are metronidazole and ciprofloxacin, which both have side effects to watch out for.
- Ciprofloxacin can lead to light sensitivity, tendonitis, tendon tears, oral thrush, QT prolongation
- Metronidazole can cause GI issues, nausea, appetite loss, nerve damage
- Rifaximin side effects are rare but may involve joint pain and muscle tension
- Vancomycin can cause itching and redness in the upper body, neck, and face.
Clinical Response And Remission

The overall flow of patients up to 1year is displayed in Figure 2. When the regimen was completed, AFM induced a clinical response in 80.8% of the participants and remission in 63.5% however, 13.5% did not experience a radical change, and 5.8% had markedly increased scores . At 3months, 73.1% were in clinical response and 65.4% remained in remission. A total of 1.9% of the patients maintained a score similar to that at baseline, 20.2% relapsed, and five patients did not show up for the follow-up outpatient clinic visit. At the 12-month follow-up, 39.4% still showed a response and remained in remission, whereas 24.0% relapsed during this follow-up period. Oral steroids were successfully withdrawn in 21 of 27 patients who had been under treatment at baseline. Twelve participants dropped out and could not be followed. For endoscopic evaluation, 74 patients underwent endoscopy at 3months. 56.8% of the patients scored 0 or 1 on endoscopic Mayo score. Similarly, 46 patients took endoscopic investigation at the 12-month follow-up, with 71.7% of the patients scoring 0 or 1.
AFM, amoxicillin, fosfomycin and metronidazole.
Focusing on the extent of the disease, the effectiveness of AFM in reaching a clinical response or remission was not significantly different among those with extensive colitis, left-sided colitis or proctitis at completion, at 3months or at 12months .
Recommended Reading: Whats A Stomach Ulcer Feel Like
Tap Into Good Bacteria
Antibiotics can trigger flares. If your UC gets worse while you take them, tell your doctor. Some scientists think antibiotics cause issues because they kill good bacteria in your gut that aid digestion. Although research is limited, there is some evidence that probiotics, which contain these bacteria, along with other medications may be helpful, but this has not been proved.
Some flare symptoms are very serious. Get medical help right away if you have:
- Constant, heavy diarrhea
- New or more blood in your stool, or any blood clots
Also get help if you feel like youre going to faint or you vomit over and over.
Also Check: Can I Buy Antibiotics At The Store
How Can I Treat Colitis At Home
The primary goal of treating colitis at home is to replace fluids and electrolytes lost because of diarrhea. Drink fluids throughout the day and include electrolyte-rich foods such as broths or soups. If the colitis is caused by an infection, get plenty of rest to help the body carry on the fight against the pathogen.
Recommended Reading: Low Carb Diet For Ulcerative Colitis
Prednisone Prednisolone And Methylprednisolone
Prednisone is taken by mouth and is available as:
- an immediate-release tablet
Its available as a generic drug and as the brand-name drugs Prednisone Intensol and Rayos .
The forms of prednisolone that are FDA approved for UC are:
- immediate-release tablet
- liquid solution
You can take any of these forms by mouth. Prednisolone is available as a generic drug and as the brand-name drugs Millipred and Prelone .
Methylprednisolone comes in two forms:
Its available as a generic drug and as the brand-name drugs Medrol and Depo-Medrol .
Side effects, complications, and interactions
When given in high doses, the side effects of these drugs are practically indistinguishable. The more common side effects can include:
- increased blood sugar levels
Immunomodulators are drugs that decrease the bodys response to its own immune system. The result is lowered inflammation throughout your body.
Immunomodulators may reduce the number of UC flare-ups you have and help you stay symptom-free longer.
Theyre generally prescribed to people whose symptoms havent been managed with 5-ASA drugs and corticosteroids. However, these drugs may take several months to start working.
The Food and Drug Administration hasnt approved immunomodulators for the treatment of UC.
However, theyre well supported in medical literature as useful options, and your doctor may still prescribe them. This is known as off-label drug use.
You May Like: Bacterial Vaginosis Caused By Antibiotics
Changes To Over The Counter Medications: What Will It Mean For You
18 September 2018
Recently published guidance by NHS England is advising bodies responsible for local health services to restrict the prescription of over the counter medications used in the treatment of minor or self-limiting conditions by GPs.
The restrictions outlined by NHS England apply to medicines such as painkillers, indigestion remedies and anti-diarrhoea medications, which are available without a prescription, and can be purchased in supermarkets, petrol stations and convenience stores.
The new guidelines will lead to a number of patients who were previously exempted from prescription charges such as older people, pregnant women and certain long-term health conditions being charged. Plus, the costs of items purchased over the counter will be in addition to the pre-payment certificate.
However, the NHS England guidance contains a number of exemptions, including for people with long-term conditions. However, that doesnt mean that if you have a long-term condition you will be automatically prescribed an OTC medication by your GP. The exemption applies in situations where the prescription is for treating or managing the long-term condition.
It isalso worth keeping in mind that the new guidance is not mandatory, and CCGs have the discretion to apply the guidance how they see fit . This will mean that local prescribing policies will vary across England.
Dont Miss: Can Ulcerative Proctitis Be Cured
Also Check: Besivance Dosage For Corneal Ulcer
Can A Chemotherapy Drug Cause Pseudomembranous Colitis
While almost any antibiotic can cause pseudomembranous colitis, some antibiotics are more commonly linked to pseudomembranous colitis than others, including: Other medications besides antibiotics can sometimes cause pseudomembranous colitis. Chemotherapy drugs that are used to treat cancer may disrupt the normal balance of bacteria in the colon.
Prevention Of Post Operative Recurrence
Endoscopic and clinical recurrence of CD is a common occurrence after surgical resection. Luminal bacteria might play a potential role in increasing the likelihood of recurrence, as one study found that recurrent disease developed only when the mucosa was re-exposed to luminal contents. Prevention of post operative recurrence of CD with antibiotics was assessed in a few clinical trials. One trial showed that the combination of metronidazole and azathioprine was associated with lower recurrence rates than receiving metronidazole alone. Other studies found that metronidazole, compared to placebo, decreases the recurrence of CD post operatively.
Don’t Miss: Is Peanut Butter Bad For Ulcerative Colitis
Check In Check Up: Ulcerative Colitis
You dont have to settle for good enough ulcerative colitis care. Take this series of assessments to evaluate how well your treatment is working.
Prednisone, hydrocortisone, and methylprednisolone work by suppressing the entire immune system, rather than targeting specific inflammatory pathways.
If you take corticosteroids orally or by injection, you may have significant side effects. Local steroids which are applied just to the area that needs treatment are generally the preferred option.
Steroids are ineffective as maintenance therapy to keep ulcerative colitis in remission.
According to Mayo Clinic, possible side effects of steroids include:
Before you begin a course of treatment using an immunomodulator, its important to have a recent complete blood count and continue periodic monitoring of your blood levels and chemistry while taking the drug.
Active Fistulizing Perianal Cd

Active fistulizing perianal CD is likely the most frequent indication for antibiotics in IBD management. Oral ciprofloxacin with or without metronidazole can be used as an adjunct to immunosuppressant therapy, usually anti-TNF. This is usually continued for 3 weeks with extension of the antibiotic course as required.
Read Also: Venous Stasis Ulcer Right Lower Leg Icd 10
More Drugs That Work On Your Immune System
Other types of medicines for ulcerative colitis target your immune system, too. Your doctor may call these immunomodulators. They may be good options if 5-ASAs and corticosteroids havenât worked well for you.
The most common ones are azathioprine , mercaptopurine , and cyclosporine . Due to the risk of side effects, doctors usually save cyclosporine for people who donât have success with other meds. They may also try methotrexate paired with folic acid.
Ozanimod is an oral medication and is the first sphingosine 1-phosphate receptor modulator approved for patients with moderately to severely active UC.
The goal is to lower inflammation in your colon.
These drugs can have side effects. They can damage your liver and make you more likely to get skin cancers, lymphoma, and infections. If you take them, your doctor will test your blood and check you for skin cancer regularly.
Cyclosporine is especially strong, but it works fast. Your doctor might prescribe it to get a severe flare under control, and then give you 6-MP or azathioprine afterward. The drug may cause kidney problems, gout, infections, and high blood pressure.
It can take several months for some of these drugs to work. So your doctor may give you a faster-acting medicine, like a low dose of a corticosteroid, to help in the meantime.
Donât Miss: What Desserts Can I Eat With Ulcerative Colitis
Understanding Ulcerative Colitis Flare
A flare-up is the reappearance of disease symptoms. And for people living with ulcerative colitis , an inflammatory bowel disease , flare-ups can be unpredictable, lasting hours, days, or weeks.
- Frequent and/or urgent bowel movements
- Lack of appetite
- Joint and body aches
Because these symptoms may also be caused by something other than UC, it can sometimes be difficult to tell whether youre experiencing a flare-up. Below, we look at factors that might affect a UC flare-up, and what can help if you are experiencing a UC flare-up.
Recommended Reading: Fodmap Diet Plan For Ulcerative Colitis
Probiotics: An Option Similar To Antibiotics
As an alternative to antibiotics, probiotics microorganisms derived from food sources such as cultured milk products like yogurt are also potential Crohns treatments. They work similarly to antibiotics by altering the balance of good and bad bacteria in the gut. Probiotics are relatively safe and carry few side effects, so it probably cant hurt to add yogurt to your daily diet. But a review of the few small studies done on probiotics for Crohns are inconclusive, according to research published in the Cochrane Database of Systematic Reviews.
There is some evidence that probiotics may work in inflammatory bowel disease, but at this point, there is more evidence for probiotics in ulcerative colitis than for Crohns, says Ausk. More research is needed before probiotics become a mainstay for Crohns treatments.