Complications Of Pressure Ulcers
If not appropriately treated, the ulcers can become infected. This is called a Stage 3 ulcer. It will appear redder in color, feel hot and tender to the touch. Additionally, some patients may experience nausea, vomiting, fever, chills, increased pain, and diminished or smaller amounts of urine output. Stage 3 pressure ulcers are potentially life-threatening because they can cause sepsis and gangrene.
Summary Of Main Results
The proportion of new pressure ulcers of any grade, stage or category
The main aim of this systematic review was to present and appraise all existing evidence regarding the relative effectiveness of repositioning on the prevention of PUs in adults. There is limited evidence, with only three small trials and data from a total of 502 participants contributing to this analysis. Moreover the three trials were at high risk of bias.
The results of the review are that we have insufficient evidence to draw a reliable conclusion of whether more frequent repositioning or different positions are more effective in reducing pressure damage. The lack of statistical power means we cannot say there is no benefit associated with more frequent repositioning since in each comparison the proportion of people developing pressure ulcers was lower in the groups receiving more frequent changes of position but the differenced did not reach conventional levels of statistical significance and so may be chance rather than “real” differences. There was a statistically significant reduction in pressure ulcers of Category 2 and above with 4hourly repositioning compared with 6hourly however we did not prespecify this outcome and this finding is exploratory.
Pressure Ulcers: Prevention Evaluation And Management
DANIEL BLUESTEIN, MD, MS, Eastern Virginia Medical School, Norfolk, Virginia
ASHKAN JAVAHERI, MD, Stanford University School of Medicine, Stanford, California, and Veterans Affairs Palo, Alto Health Care System, Palo Alto, California
Am Fam Physician. 2008 Nov 15 78:1186-1194.
Pressure ulcers, also called decubitus ulcers, bedsores, or pressure sores, range in severity from reddening of the skin to severe, deep craters with exposed muscle or bone. Pressure ulcers significantly threaten the well-being of patients with limited mobility. Although 70 percent of ulcers occur in persons older than 65 years,1 younger patients with neurologic impairment or severe illness are also susceptible. Prevalence rates range from 4.7 to 32.1 percent in hospital settings2 and from 8.5 to 22 percent in nursing homes.3
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Compared with standard hospital mattresses, pressure-reducing devices decrease the incidence of pressure ulcers.
| Clinical recommendation | |
|---|---|
|
There is no evidence to support the routine use of nutritional supplementation and a high-protein diet to promote the healing of pressure ulcers. |
|
|
Heel ulcers with stable, dry eschar do not need debridement if there is no edema, erythema, fluctuance, or drainage. |
|
|
Ulcer wounds should not be cleaned with skin cleansers or antiseptic agents because they destroy granulation tissue. |
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Recommended Reading: Symptoms Of A Bleeding Ulcer In Your Stomach
What Are The Best Practices In Pressure Ulcer Prevention That We Want To Use
Once you have determined that you are ready for change, the Implementation Team and Unit-Based Teams should demonstrate a clear understanding of where they are headed in terms of implementing best practices. People involved in the quality improvement effort need to agree on what it is that they are trying to do. Consensus should be reached on the following questions:
In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources.
In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. Some of the factors that make pressure ulcer prevention so difficult include:
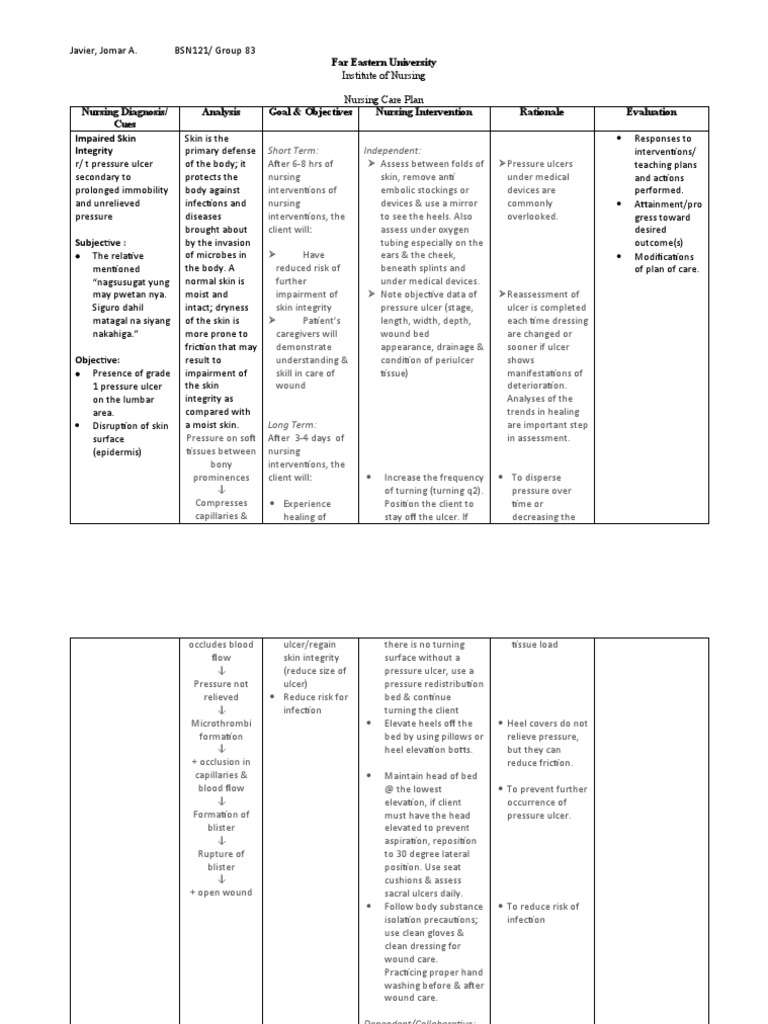
Nursing Care Plans For Pressure Ulcers
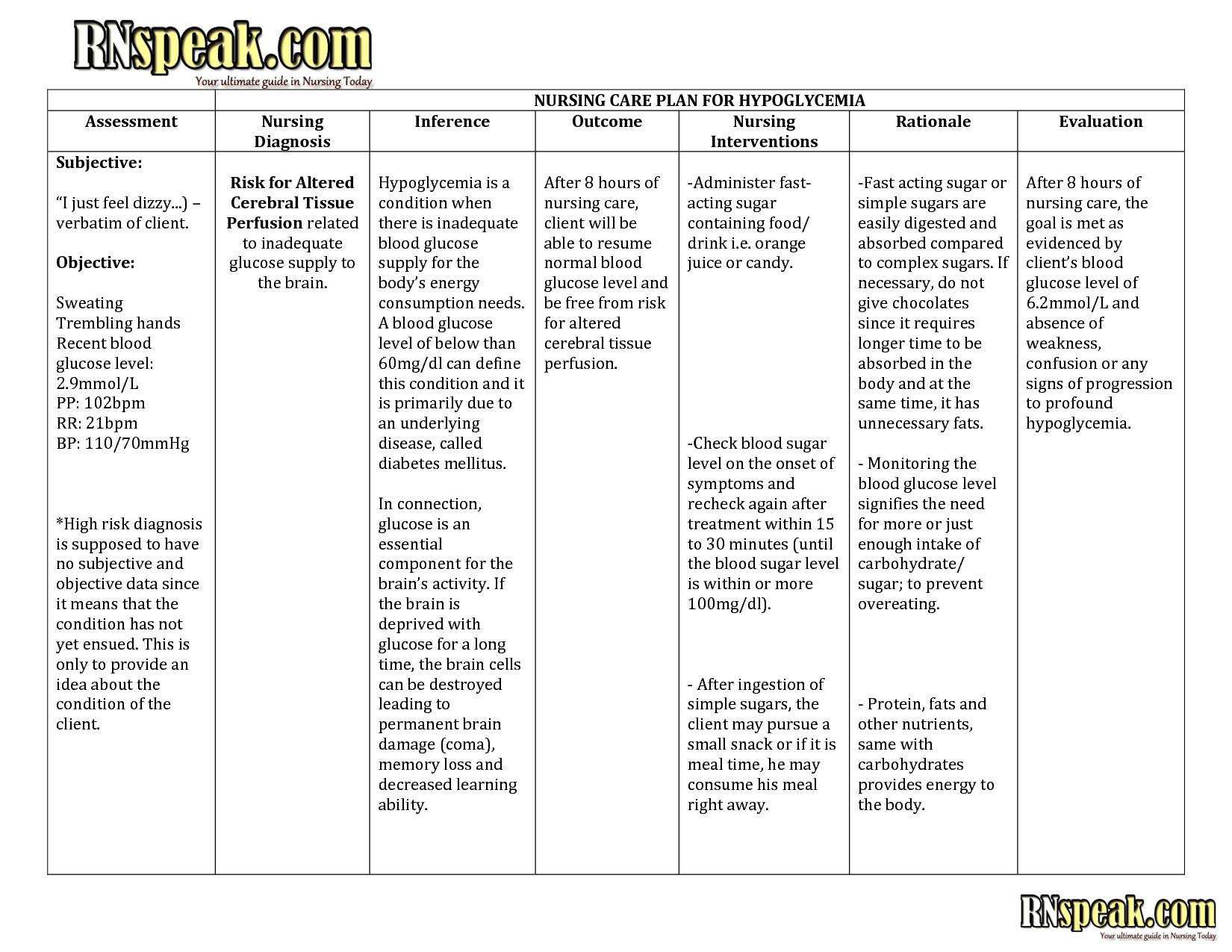
The nursing care plan should include a summary of the following factors:
-Patient Assessment: This part of the plan includes reviewing the patients history, medications, and other pertinent information. This allows the nurse to establish goals related to their needs, assess for potential complications, and determine expected outcomes and whether or not they are appropriate for that particular patient.
-Diagnoses: Is the wound created by pressure and friction, or is it a puncture, burn, abrasion, etc.? Each wound responds differently to treatment and will require different treatments depending on its location and severity.
-Goal: This part of the plan states what we hope to achieve to help the patient return to their baseline state. It also includes an objective to evaluate the patients progress and individualized goals that align with overall treatment plans.
Objective: This part aims to list any nursing interventions that will lead to meeting the established goal for that patient. If there are patient-specific care objectives, then those should be included in this part of the plan.
-Evidence: This section is based on current evidence and best practice. It explains how the treatment will achieve specific outcomes that are important to patient care.
Recommended Reading: How Do You Get A Peptic Ulcer
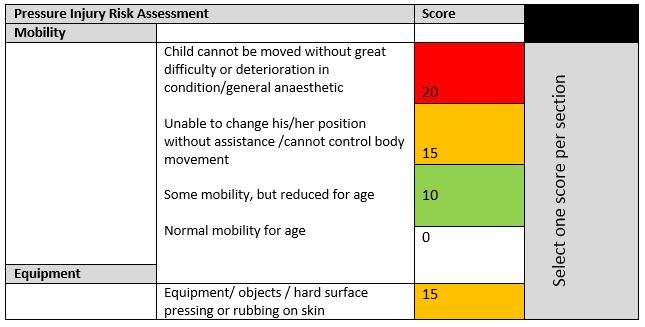
Neonates Infants Children And Young People: Risk Assessment
-
Carry out and document an assessment of pressure ulcer risk for neonates, infants, children and young people:
-
being admitted to secondary care or tertiary care or
-
receiving NHS care in other settings if they have a risk factor, for example:
-
significantly limited mobility
-
significant loss of sensation
-
a previous or current pressure ulcer
-
nutritional deficiency
-
the inability to reposition themselves
-
significant cognitive impairment.
What Items Should Be In Our Bundle
The sections above have outlined best practices in pressure ulcer prevention that we recommend for use in your bundle. However, your bundle may need to be individualized to your unique setting and situation. Think about which items you may want to include. You may want to include additional items in the bundle. Some of these items can be identified through the use of additional guidelines .
Action Steps
Identify your bundle of best practices.
3.5.1 How do we customize the bundle for specific work units?
Patient acuity and specific individual circumstances will require customization of the skin and pressure ulcer risk assessment protocol. It is imperative to identify what is unique to the unit that is beyond standard care needs. These special units are often the ones that have patients whose needs fluctuate rapidly. These include the operating room, recovery room, intensive care unit, emergency room, or other units in your hospital that have critically ill patients. In addition, infant and pediatric patients have special assessment tools, as discussed in section 3.3.5.
Action Steps
- Identify the units that will require customization of the skin and risk assessment protocols.
- Modify the bundle, the assignment of roles, and the details of the unit to meet these special features.
Additional Information
Don’t Miss: Ulcerative Colitis Social Security Disability
Interventions For Pu Prevention And Treatment
A wide range of interventions is used in the prevention and treatment of PUs. Key preventative interventions include those which aim to redistribute pressure at the interface between the skin and the support surface . Key treatment interventions include support surfaces and also wound dressings. The UK National Institute for Health and Care Excellence commissioned the National Clinical Guideline Centre to produce a detailed clinical guideline for the prevention and management of PUs in primary and secondary care, which contains a list of interventions used in clinical practice . The main types of intervention are summarised in Box .
The Burden Of Pressure Ulcers
The burden of pressure ulcers on those living with them, on those engaged in efforts to prevent and treat them, and on healthcare resources, is enormous. Pressure ulcer prevention and reduction is a high priority for the NHS . Commissioning for Quality and Innovation suggests that, based on the NHS Safety Thermometer Pilot, pressure ulcer incidence can be halved in one year, and the tools they cite for achieving this include high quality evidence . The NICE guideline on Pressure ulcers: prevention and management draws on the best available evidence but in relation to many core elements of care this is not high quality. Decisions about care need to be informed by reliable evidence of effectiveness and safety, but primary research is lagging behind.
Read Also: How To Prevent Skin Ulcers
Aetiology And Prevalence Of Pressure Ulcers
Pressure ulcers , sometimes known as pressure injuries, decubitus ulcers or bed sores, are wounds that involve the skin or underlying tissue, or both. They are localised areas of injury occurring most often over bony prominences, such as at the sacrum or heel, where prolonged pressure and sheer forces act to damage tissues and reduce perfusion, causing changes in the tissue and ultimately leading to the wound . PUs are graded according to a number of systems, one widely recognised system being that of the National Pressure Ulcer Advisory Panel . These wounds have a range of serious negative consequences and can severely impair quality of life .
This article aims to provide an overview of the evidence relating to PU prevention and treatment, in particular drawing on Cochrane systematic reviews since they are widely regarded as rigorous and comprehensive summaries of research . It also aims to assess the degree to which people with SCI have been included as participants in trials of PU interventions.
Agreements And Disagreements With Other Studies Or Reviews
Our results are consistent with others’ assessment of the evidence for repositioning. The systematic review by , was published before one of our included trials, , was undertaken. The results of the review by suggested that the evidence around repositioning remains somewhat inconclusive, and the methodology for PUP trials sub optimal.
Read Also: Signs Of Having An Ulcer
What This Paper Adds
- A pressure ulcer prevention bundle for nursing homes is acceptable and has the potential to improve care.
- Nursing home staff believed their care became more comprehensive when using the bundle and they felt accountable for the care provided due to the inclusion of staff signatures on the bundle documentation sheet.
- We identified the following issues to be addressed by future studies: recruitment and retention collection of care and outcome data staff adherence.
Purpose Of Systematic Review
Knowledge is translated from research into clinical practice based on the evidence reported by systematic reviews . Yet, there has not been a systematic review of the intensive care literature published since 2002 for HAPU prevention strategies incorporating the Braden scale , and none focused on care bundles. The purpose of this systematic review was to evaluate the effectiveness of care bundles incorporating the Braden scale for risk assessment in reducing the HAPU prevalence in older adults hospitalized in the ICU.
Recommended Reading: Crohn’s Versus Ulcerative Colitis Pathology
Priorities In Pressure Ulcer Research
Not only do we need research to be designed, implemented and reported in ways that ensure it is useful, but to address the most important aspects of pressure ulcer prevention and treatment.
One of the objectives of the Wounds Research for Patient Benefit Programme Grant was to research priorities for people with complex wounds from the perspectives of patients, carers and healthcare professionals. Pressure ulcers were selected as the focus for the first National Institute for Health Research James Lind Alliance Priority Setting Partnership on complex wounds and with this came the particular challenges of involving people with pressure ulcers in research associated with their age, multiple morbidities and social isolation. Indeed the service users who participated in this research prioritization exercise were generally younger and fitter than those most at risk of pressure ulcers, nevertheless the PSP succeeded in identifying research priorities which capture the views of patients, carers and healthcare professionals . Of the top 10 priorities, which were extended to 12 during the PSP prioritization exercise, the first five concern pressure ulcer prevention.
Service users have helped identify priorities in pressure ulcer research
Management Of The Residents Possessions On The Beds
It was not at all easy to manage the clutter on the residents beds. Due to insufficient space, it was impossible to give additional bedside cabinets to each resident. The in-charge of each nursing home explained to the family members how these belongings, which occupied much of the bed, affected the care provided to the residents. The family members were strongly advised to avoid buying unnecessary items for the residents. In the meantime, the PCWs cleared and tidied the beds every day and the existing bedside cabinets at least once a week in order to create more space to store as many of the belongings that had been placed on the beds as possible.
Read Also: Imodium Ulcerative Colitis Toxic Megacolon
Description Of The Condition
A pressure ulcer is “a localised injury to skin or underlying tissue usually over a bony prominence as a result of pressure or pressure in combination with shear” . PUs occur when the soft tissue is compressed between a bony prominence and an external surface for a prolonged period of time.
PU classification systems provide an accurate and consistent means by which the severity and level of tissue injury of a PU can be described and documented .The words ‘stage’ , ‘grade’, and ‘category’ are used interchangeably to describe the levels of softtissue injury. The original staging system includes Stages 1 to 4. Stage 1 reflects persistent nonblanching erythema of the skin . Stage 2 involves partialthickness skin loss . Stage 3 reflects fullthickness skin loss involving damage, or necrosis, of subcutaneous tissue, whereas in Stage 4 the damage extends to the underlying bone, tendon or joint capsule. However, more recently, two additional classifications have been identified, namely: ‘unclassified/unstageable’ and ‘deep tissue injury’ . PUs are associated with pain, an increased risk of infection and sepsis, longer hospital stays, higher hospitalisation costs and mortality .
Evidence Is Lacking In All Areas Of Pressure Ulcer Prevention And Treatment
There is insufficient evidence to inform practice on nutritional interventions to prevent pressure ulcers or aid healing
Other Cochrane reviews found insufficient evidence to inform practice on the use of nutritional interventions to prevent or promote pressure ulcer healing on topical agents and massage as preventive measures and on treatment with pressure-relieving devices for heel pressure ulcers , ultrasound antibiotics and antiseptics , phototherapy reconstructive surgery electromagnetic therapy and bed rest for wheelchair users with pressure ulcers .
There is no good evidence to support any particular wound cleansing agent or technique for pressure ulcers . There was no evidence from randomized studies on the impact of wound-care teams for pressure ulcer prevention and management . Nor has the use of structured risk assessment tools been shown to be effective in reducing pressure ulcer incidence .
The review on support surfaces found that standard foam mattresses were consistently out-performed by higher specification foam mattresses, and that medical grade sheepskins are associated with a lower incidence of pressure ulcers, but more, better, research is needed in this area too. For managing existing pressure ulcers, there is no conclusive evidence on the superiority of any support surface .
Read Also: Holistic Cure For Ulcerative Colitis
Signs And Symptoms Of Decubitus Ulcer
The general clinical manifestations of decubitus ulcers include:
- Unusual skin color or texture discrepancies
- Erythema or redness
- Edema or swelling in the affected area or limb
- Discharges foul in odor, can be fluid or pus-filled
- Warm or cold to touch An area of the affected region that feels different to touch than surrounding areas
- Tenderness and pain on site
Negative Pressure Wound Therapy
This is an invaluable tool in the management of pressure sores and involves the application of sub-atmospheric pressure to a wound using a computerised unit to intermittently or continuously convey negative pressure to promote wound healing. NPWT, is effective for deep, cavitating, infected and copiously discharging pressure ulcers, particularly with exposed bone. With growing clinical experience it can be said with certainty that it assists wound healing, and its benefits can be summarised thus:
-
Assists granulation.
-
Applies controlled, localised negative pressure to help uniformly draw wounds closed.
-
Helps remove interstitial fluid allowing tissue decompression.
-
Helps remove infectious materials and quantifies exudates loss.
-
Provides a closed, moist wound healing environment
-
Promotes flap and graft survival.
-
Both hospital and domiciliary use.
-
Reduces hospital/dressings/nursing cost .
Don’t Miss: Prednisone For Ulcerative Colitis Reviews
Adherence With The Clinical Interventions
The reported all-or-none adherence to the bundle was 16%, although this varied throughout the 9 weeks . The reported adherence to the individual elements also varied: adherence was 75% to the repositioning element 22% to the support surfaces element and 21% to the skin inspection element. The reasons for non-completion were rarely documented.
Figure 1
Systematic Reviews Of Interventions For The Prevention And Treatment Of Pus: Search Of The Cochrane Library
A range of Cochrane systematic reviews has been undertaken to summarise the current evidence from RCTs of interventions for the prevention and treatment of PUs. A search of The Cochrane Library up to July 2017 revealed 50 results , 27 of which are relevant to this review . Of these, 23 reviews evaluate interventions specifically relating to PUs, and 4 relate to several types of chronic or complex wound including PUs. Twenty-one reviews found trials, which were eligible for inclusion, whilst five were empty reviews and another, whilst including various types of wound, did not include any patients with PUs. Of the 50 retrieved results from the search, 23 reviews were not relevant to this overview .
Fig. 1
Don’t Miss: How Do They Check For Ulcers