Ulcerative Colitis Symptoms And Causes
Ulcerative colitis is thought to develop when a person at genetic risk is exposed to certain environmental stressors.
These environmental stressors either change the ratio of gut bacteria or alter the way the immune system responds to bacteria .
As a result, the immune system attacks the intestinal lining causing inflammation and other symptoms, including:
Low Fodmap Diet For Ulcerative Colitis
People with ulcerative colitis are often advised to follow a low-FODMAP diet as part of their management. This dietary plan limits the amount of fermentable oligosaccharides, disaccharides, monosaccharides and polyols that are consumed. These types of carbohydrates are thought to cause inflammation in the colon.
The low-FODMAP diet is not always easy to follow, but it has been shown to be helpful in managing UC. The diet includes restrictions on high-FODMAP foods, which can be challenging to identify. A list of low-FODMAP foods can be found here.
It is important to keep in mind that not all foods are low-FODMAP, and that the diet should
What Triggers Microscopic Colitis
Although a low-FODMAP diet is not very useful in treating microscopic colitis, several foods and lifestyle activities can trigger the condition, and avoiding them is useful.
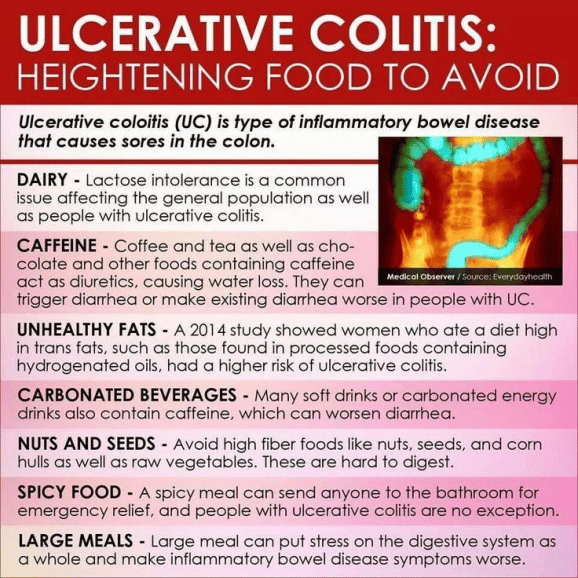
Fatty, high-fiber foods, dairy products, gluten-containing items, caffeine, sugar, inadequate hydration, spicy foods, and eating large meals can all make microscopic colitis worse. If you have the condition, consider avoiding the following items:
Many patients with microscopic colitis also have celiac disease. If you have microscopic colitis, your chances of developing celiac disease are higher than the average population. In celiac disease, your body is intolerant to a protein called gluten. Gluten is found in bread, pasta, breakfast cereal, and cakes.
If you develop abdominal symptoms after eating gluten-containing items, you may have celiac disease on top of microscopic colitis. The only treatment for celiac disease is lifelong avoidance of gluten.
Note that food sensitivities vary between patients. What worsens your symptoms might be completely fine for another patient and vice versa. Instead of eliminating everything in this list, keep a food diary.
In a food diary, you write everything you eat, the serving size, and the how you feel after eating a particular food. At the end of a month or two, you can analyze the diary and identify the foods that trigger your microscopic colitis. You can then avoid those items.
Read Also: Ozanimod Ulcerative Colitis Phase 2
What Is Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease that affects that affects the colon, or large intestine. Typically, the inflammation starts in the rectum and then extends continuously throughout the colon. It is commonly diagnosed in your thirties, and takes a flare and remission pattern where sometimes you feel okay and other times you dont.
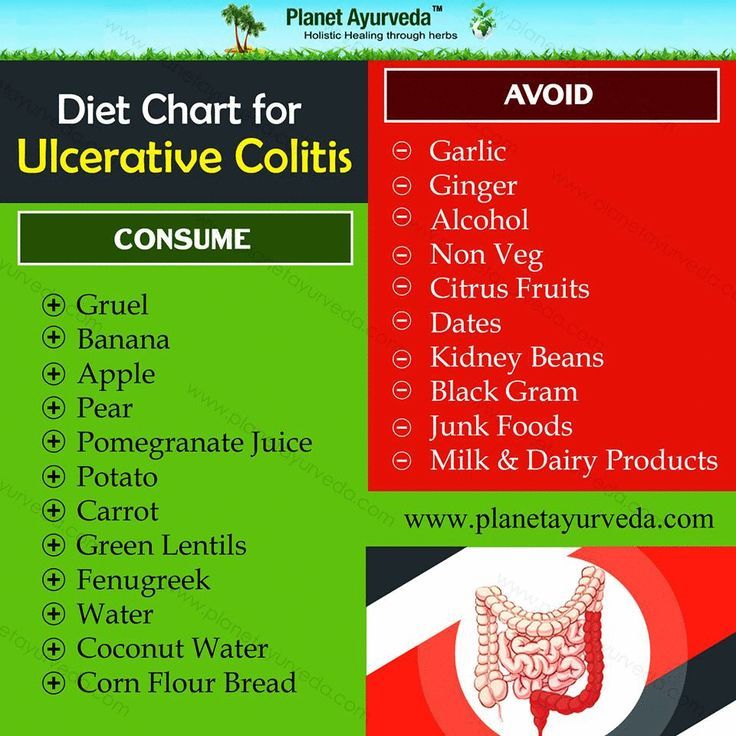
Dietary Modification In Indian Diet Plan For Ulcerative Colitis:
- Soft bland food is much accepted by the body than spicy or high fiber foods.
- To get enough vitamins and nutrients a low fiber, high-protein, high-calorie eating plan is necessary.
- Eat small meals every 2 or 4 hours.
- Drink at least 8 cups of water per day to avoid dehydration.
- Eat foods containing added probiotics and pre-biotics to encourage better gut health.
- Limit oils to 8 teaspoons a day.
- There are people who cannot tolerate milk or milk products. This is the stage where they develop different levels of lactose intolerance.
- There may be people who can tolerate curd and buttermilk but no other milk products.
- And on another side, there are few individuals, who cannot tolerate even a single milk product. At such times milk is replaced by any plant-based milk like almond, soy, or coconut milk as per tolerance.
- Certain people cannot tolerate wheat. They are categorized as gluten-sensitive individuals. They should avoid wheat, broken wheat, Rawa, rye. Rice, maize flour, and potato starch or potato flour replace wheat.
- Low fiber or low residue diet works wonders for individuals suffering from UC. It contains easy to digest the food that controls the episodes of diarrhea.
You May Like: What Are The Symptoms Of An Ulcer In A Child
Studying This Diets Effect On Ibd
An initial study, conducted in London, involved the participation of patients with IBD who were in remission but had symptoms of IBS. It was found that the patients had all experienced improvements in their symptoms after following a low FODMAP diet. However, instead of testing this analysis further, the researchers aimed to determine whether high doses of FODMAPs aggravated their symptoms. Each patient received a three-day plan, including three various types of FODMAPS. It was found that one type of FODMAP in particular, known as fructans, was associated with more severe symptoms, including stomach pain, bloating, gas, and urgency. As a result, the researchers concluded that eliminating FODMAPS in patients with IBD could prove effective in alleviating symptoms and improving quality of life.
Keeping A Food Journal
Everyones body is different, so its possible for two people who have UC to have different trigger foods.
Logging what you eat throughout the day and when digestive issues occur can help you and your doctor narrow down your personal food triggers.
A food journal can be especially helpful if youre trying a new diet.
You May Like: Ulcerative Colitis Diet Plan During Flare Up
How Can I Track Foods That Cause Flare
The Crohn’s and Colitis Foundation of America recommends people with ulcerative colitis keep a food journal to keep track of what they eat. Note what you eat and drink, and how you feel afterward, noting any symptoms that arise. Start to keep a list of any foods you suspect may trigger or aggravate your ulcerative colitis symptoms. A food diary will also help you figure out if you are getting adequate nutrition, and can help your doctor or dietician determine the right diet for you to manage your symptoms and prevent flares.
The Crohn’s and Colitis Foundation of America also has an interactive food tracking tool. It is available online or as a mobile app. www.ccfa.org/gibuddy
Indian Diet Plan For Ulcerative Colitis Foods To Avoid:
- Red meat or high-fat non-vegetarian foods.
- Deep-fried foods, junk, and fast foods.
- High fiber raw vegetables like lettuce, cruciferous vegetables like cabbage, cauliflower, broccoli, or brussels sprouts.
- Heavily spiced sauces, gravies, pickles, or chutneys.
- Foods and beverages containing caffeine and cocoa.
- Avoid alcohol as much as possible.
Don’t Miss: What’s The Difference Between Ulcerative Colitis And Crohn’s Disease
Do Inflammatory Foods Play A Role In Ulcerative Colitis
If youre searching for an ulcerative colitis treatment that starts with your diet, you are far from alone. David Schwimmer, M.D., a board-certified gastroenterologist at Florida Digestive Health Specialists in Sarasota, Florida, sees ulcerative colitis patients on a daily basis and has even lived with the condition himself since he was 18 years old. I think every patient that has a GI illness certainly thinks that what they are consuming and what theyre eating has an impact on their disease, he says.
Exclusion diets like the specific-carbohydrate diet, the semi-vegetarian diet, and the IBD-inflammatory diet continue to grow in popularity within the IBD community. But research to prove that these diets are helpful for ulcerative colitis lags behind the trend. As recently as 2019, a study published in the journal Nutrients concluded that the mechanism by which dietary interventions impact inflammation in IBD remains unknown1. Basically, theres a lot more scientists need to learn before one type of diet reigns supreme for people with IBD.
Eat In: Ulcerative Colitis Meal
When you have a gastrointestinal issue like UC, you cant rely on restaurants and takeout counters to have foods that suit your needs. Many restaurants use a lot of butter to make their food taste so good.
Thats why you may want to do more cooking at home using fresh foods if possible, not prepared stuff packed with preservatives.
Some people with UC find that eating four to six small meals instead of three large ones keeps their guts happier, which means youve got more dishes to plan than ever.
Pick up some meal-prep habits if you havent yet. Those include planning bigger meals in a slow cooker or making staples like baked chicken, starches, or roasted veggies that you can mix and match for the rest of the week.
While youre shopping for the week ahead, pick up some of the staples youll need during a flare-up, too. That way you can skip going to the store when youre under the weather.
Recommended Reading: What Causes Venous Leg Ulcers
How A Fodmap Diet May Help Ease Ibd Symptoms
In the 2019 research, scientists tracked 52 people with IBD by measuring their persistent gut symptoms, markers of inflammation, and fecal microbiome. At the end of the 4-week study, 52 percent of people who followed the low-FODMAP diet reported relief of gut symptoms after the trial, compared with just 16 percent of people who followed a control diet. Plus, those who stuck to the low-FODMAP diet scored higher on quality-of-life assessments.
While the researchers concluded that a low-FODMAP diet is safe and can help control symptoms of Crohns and UC, one of the difficulties of studying the microbiome is that everyones gut bacteria is distinct, says Shen.
Each of us has at least 5,000 different kinds of bacteria in our gut, he says. That makes drawing valid conclusions from comparisons among people difficult. Further research could focus on comparing the microbiome of the same patient before and after a low-FODMAP diet.
Ulcerative Colitis Diet: Foods To Eat And Foods To Avoid
Here in Canada, we have one of the highest rates of ulcerative colitis in the world it is thought that our environment + lifestyle weigh heavily on our risk for the disease.
Most people with ulcerative colitis report that food impacts their symptoms, so its important that nutrition is not overlooked in the management of the disease. Recent evidence suggests that intake of certain foods is associated with a higher risk of ulcerative colitis, including:
- Meat, particularly red meat
- Sugar, and sugar sweetened beverages
- Omega 6 fatty acids
We also know that the inflammation and increased bowel movements in ulcerative colitis and Crohns disease can lead to malabsorption, low food intake and nutrient deficiencies along with osteoporosis. So everyone with ulcerative colitis should be receiving adequate nutrition therapy.
Don’t Miss: Are Oranges Bad For Ulcerative Colitis
When Should You See A Doctor About Ulcerative Colitis Food Triggers
According to Dr. Schwimmer, seeing a doctor at the first sign of ulcerative colitis symptoms is your safest bet, especially if youve never been formally diagnosed. Concerning, unexplained symptoms like bloody stool, diarrhea, and abdominal cramping shouldnt be ignored, because even if its not ulcerative colitis, you might be dealing with something else that needs proper treatment.
After youve been diagnosed, your doctor might recommend making diet adjustments as a part of your ulcerative colitis treatment plan. But ultimately, FDA-approved medications, which help control the inflammation that sets off GI pain, are going to be the main course of treatment that your doctor suggests for the long haul of this chronic condition.
There is no secret treatment for inflammatory bowel disease. Everybodys looking for the secret pills. What diet can I follow? What supplement can I take? What probiotic can I take? Unfortunately, it just doesnt exist, Dr. Schwimmer says. But the medicines we have work and they work better than anything else.
Thats why doctors who specialize in IBD caution that self-treatment with diet is not enough. If you arent working within the framework of a plan that includes proven, FDA-approved medication, you are at a higher risk of complications from your ulcerative colitis, including malnutrition.
Fodmap Diet For Rheumatoid Arthritis
There is a lot of information out there about the Fodmap Diet for Rheumatoid Arthritis, so Ill try to be concise. The Fodmap Diet is a low FODMAP diet designed to help with various digestive issues, including rheumatoid arthritis. The FODMAPs are short chain carbohydrates that are poorly absorbed in the small intestine. They can cause problems such as bloating, gas, and diarrhea.
There are certain foods that are high in FODMAPs and should be avoided on the Fodmap Diet for Rheumatoid Arthritis. These include:
Fruits
The Fodmap Diet for Rheumatoid Arthritis
Don’t Miss: How To Treat Rodent Ulcers In Cats At Home
Ulcerative Colitis Vs Crohns Disease
Crohns Disease is another inflammatory bowel disease that shares similarities to ulcerative colitis, with a few key differences. The first is that Crohns disease can technically occur along the entire length of the GI tract, as opposed to ulcerative colitis occurring exclusively in the colon. Crohns disease also presents in discontinuous patches as opposed to the continuous diseased areas in ulcerative colitis. Imbalances in gut bacteria tend to be more pronounced in Crohns disease than ulcerative colitis. Finally, the inflammation in ulcerative colitis typically does not go as deeply into the gut tissue layers as in Crohns disease, but both diseases show evidence of gut barrier dysfunction, or leaky gut.
Dont Miss: Succeed For Horses With Ulcers
Specific Carbohydrate Diet For Uc
Similar to the low FODMAP diet, the SCD restricts certain carbohydrates from a personâs diet to help reduce gastrointestinal symptoms. It is a grain-free, low sugar, and low lactose diet.
It theorizes that people do not fully digest complex carbohydrates and therefore they remain in the gut. These carbohydrates cause an overgrowth of bad bacteria in the small intestine, leading to inflammation.
Studies on the SCD are still in their early stages, but anecdotes support its effectiveness. Research from a 2016 study showed 33% reported remission within 2 months after starting the SCD. Almost half of the people were in remission within 6â12 months of starting the diet.
Foods allowed in the SCD include:
- meats, or substitutes without additives
- juices with no sugar or additives
Foods to avoid include:
In addition, a person cannot eat anything processed and canned, including most processed meats. Other prohibited foods include:
- certain legumes such as chickpeas and bean sprouts
- seaweeds and their byproducts
- all milk and milk byproducts with high lactose, including sour cream, ice cream, and commercial yogurt
- candies and chocolates
Recommended Reading: Can Tylenol Cause Stomach Ulcers
Pico And Research Question
The research question of the study was: What is the effect of adopting an LFD among patients with quiescent IBD who have IBS or other functional GI symptoms? The PICO criteria were: Patients with IBD in remission experiencing FGS the Intervention was adherence to an LFD the Comparator was a standard/sham diet, placebo, or non-FODMAP elimination diet and the Outcome was a change in FGS. The protocol was registered at the Center for Open Science and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines were adhered to.
Low Fodmap Diet And Ibd
Evidence has been found to show that a low FODMAP diet helps to relieve symptoms of irritable bowel syndrome 1 but there is currently no evidence to suggest that it works for people with inflammatory bowel disease , although some people with IBD do find it helpful in controlling some of their symptoms.
References
Also Check: Low Dose Aspirin Ulcerative Colitis
Don’t Miss: Can Pregnancy Cause Ulcerative Colitis
Low Fodmap Diet For Colitis
It can be embarrassing to talk about your bowel movements. And so many people suffer from loose stools now and then, that you may not see it as a great health issue. However, if you start to see blood or pus in your stool during bowel movements, then it could be something more serious. As of 2015, about 1 in 100 adults suffer from inflammatory bowel disease , which can be either Crohns disease or colitis. Colitis is an inflammatory disease of the large intestine that can worsen over time if left untreated. Therefore, lets talk about what colitis is, how it can be treated, and if the low FODMAP diet could help.
What is colitis?
Colitis, also known as ulcerative colitis , is a condition where the large intestine becomes chronically inflamed. The most common symptom of colitis is bloody diarrhea or loose stools with pus in it. Other signs and symptoms of colitis include:
- Urgent need to have bowel movements
- Anemia, or a low level of red blood cells in the blood
Early stages of colitis may only have mild to moderate symptoms. Bu as the disease progresses, symptoms may become more severe such as frequent bloody stools, fever, and severe abdominal cramping. These more severe symptoms are only seen in about 1 in 10 of people in the early stages of colitis.
Colitis treatment
The low FODMAP diet and colitis
Take home message
-written by Staci Gulbin, MS, MEd, RD at LighttrackNutrition.com
An Ulcerative Colitis Diet: Summarizing The Evidence
Despite many reports online that certain diets or supplements can cure ulcerative colitis, the only known cure is total removal of the colon and rectum.
Those with digestive symptoms during remission may find relief from a low FODMAP diet to identify trigger foods.
A semi-vegetarian diet has also shown promise in maintaining remission in Crohns disease and may be helpful for ulcerative colitis, but we cannot make firm conclusions.
Even without following elimination diets, certain patterns have been shown to reduce symptoms:
- A diet that is rich in fruits and vegetables provides fiber and antioxidants, which are linked to lower disease risk. Reducing intake of high-fiber fruits and vegetables may increase comfort during flares.
- Limiting dietary fat, especially fatty meats, may be beneficial.
- Certain probiotics are helpful in bringing about and maintaining remission. Ask your doctor for a recommendation.
- A few herbal supplements show promise but lack sufficient scientific evidence to support their use.
- Avoid foods that irritate the gut during flares, including fatty foods, caffeine and alcohol.
A registered dietitian can help you identify foods that trigger your symptoms and design a well-balanced meal plan.
Also Check: How To Reduce Ulcer Pain