When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
Wound And Pressure Ulcer Management
Introduction
Education of patients, families, caregivers and healthcare providers is the key to a proactive program of prevention and timely, appropriate interventions . Wound management involves a comprehensive care plan with consideration of all factors contributing to and affecting the wound and the patient. No single discipline can meet all the needs of a patient with a wound. The best outcomes are generated by dedicated, well educated personnel from multiple disciplines working together for the common goal of holistic patient care .
Significance of the problem:
Prevention
Anatomy of Normal Skin
What is a Pressure Ulcer?
There are many contributing factors.
Which Other Interventions May Help When Treating Pressure Ulcers
Relieving the source of pressure, repositioning the patient, and using air-fluidized beds are recommended to treat pressure ulcers.4,22Moderate-strength evidence supports the use of radiant heat dressings and electrical stimulation.4,22Alternating-pressure surfaces, platelet-derived growth factor, and light therapy may also help.4,22Surgical consultation should be considered for advanced ulcers not responding to standard therapy.
You May Like: Stomach Ulcer And Chest Pain
What Is The Best Way To Cleanse And Dress A Pressure Ulcer
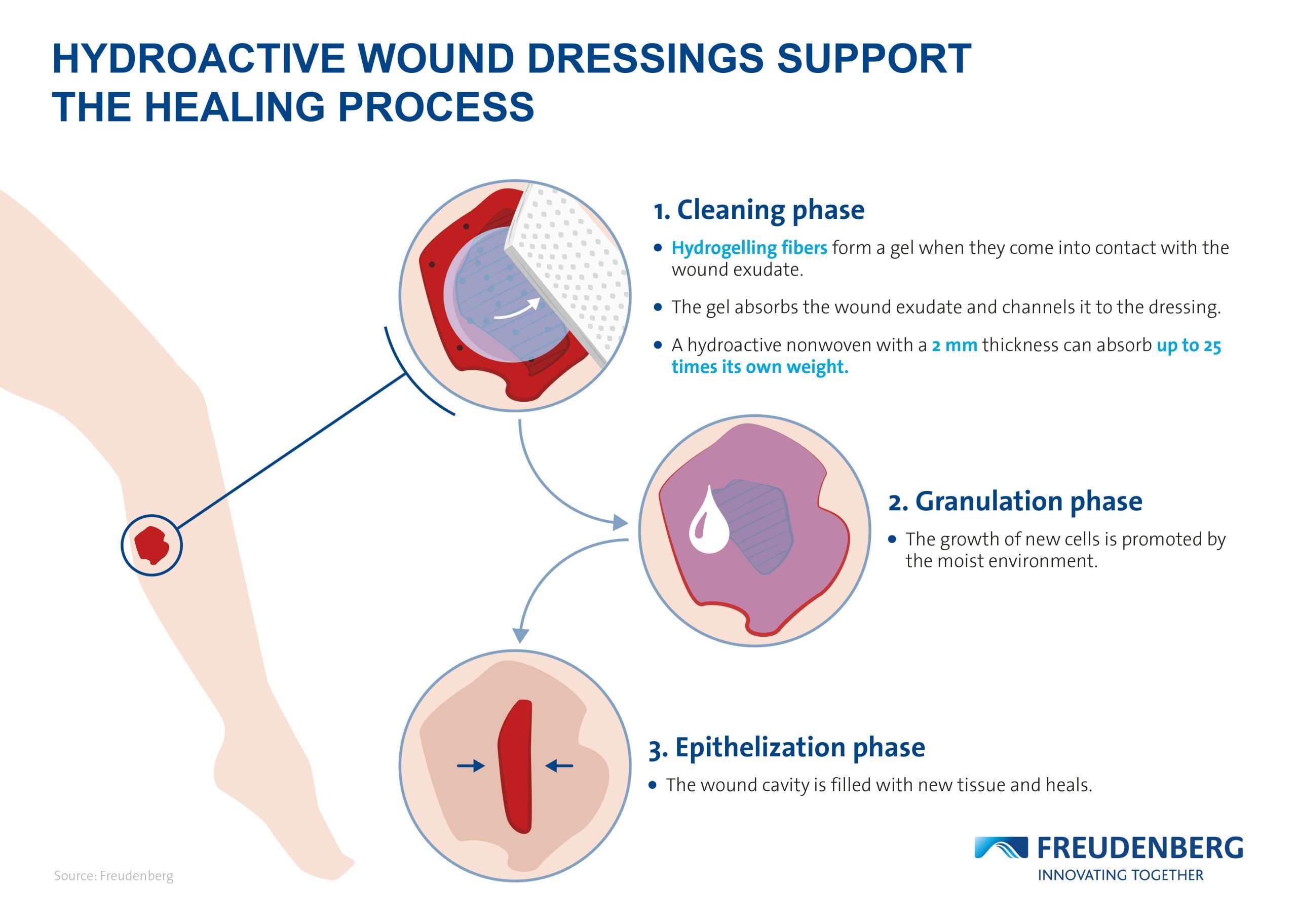
Pressure ulcers should be cleansed with saline or tap water.1,20,21They should be debrided of slough and necrotic tissue. A hydrocolloid, foam, or other nonadherent dressing that promotes a moist wound environment should be used.4,22Wet-to-dry dressings, povidone-iodine solution, and Dakin’s solution should be avoided.23,24Pain associated with cleansing or dressing pressure ulcers should be treated appropriately.
Polyacrylate Moist Wound And Debridement Dressings
This activated absorbent polyacrylate polymer core dressing absorbs large protein molecules while irrigating with Ringer’s solution, a physiological fluid, creating a rinsing effect . The interactive dressing supports both moist wound healing and autolytic debridement, gently removing dead tissue from the wound bed while creating an ideal healing environment. Polyacrylates debride at a mean rate of 38%.34 Research has shown that polyacrylate gel absorbents debride just as well as collagenase does.36 Recent research has also shown that the product may be effective in reducing wound bioburden by interfering with biofilm as well as absorbing planktonic or free-floating bacteria.35
Also Check: Yea Sacc For Horses With Ulcers
What Types Of Wound Dressing Can Be Used On Bed Sores
By Nursing Home Law Center
In order for bed sores to heal, attention must be paid to the removing dead tissue and protecting the wound from infection causing bacteria. Dressings are usually applied to help the body heal itself. The type of dressing and the frequency with which it is to be changed is ordered by a physician with the application and changes carried out by nurses.
Many patients with bed sores suffer additional harm when the staff responsible for caring for them fails to follow medical orders with respect to the frequency with which dressings are to be changed. If dressings are not changed according to orders set forth by a physician, the healing of the bed sores may be delayed and perhaps become infected.
The most commonly used dressings used to treat bed sores include:
Absorptive Dressings: These dressings are either applied directly to the wound or on top of other primary dressings. Absorptive dressings are intended to remove the drainage from the bed sore that may impede healing. Most absorptive dressings are changed on a daily basis. However, excessive drainage from a bed sore may require more frequent dressing changes.
Common types of Absorptive dressings include: Medipore, Silon Dual Dress, Aquacel Hyrofiber Combiderm, Absorbtive Border, Multipad Soforb, Iodoflex, Tielle, Telefamax, Tendersorb, Mepore and Exu-dry.
Call Toll-Free for a No Obligation ConsultationCall Toll-Free for a No Obligation Consultation
Related Information
How Can Pressure Injuries Be Prevented
The development of pressure injuries can be prevented through careful observation of the skin and frequent repositioning in those who canât turn themselves. Tips to prevent pressure injuries include:
- Keeping the skin clean and clear of bodily fluids.
- Moving and repositioning the body frequently to avoid constant pressure on bony parts of the body.
- Using foam wedges and pillows to help relieve pressure on bony parts of the body when turned in bed.
- Maintaining a healthy diet to avoid malnutrition and to assist in wound healing.
Recommended Reading: What Are The Best Foods To Eat With An Ulcer
Positioning And Support Surfaces
Preamble: Pressure and compression to soft tissue play a role in the etiology of pressure ulcers. Patient positioning and methods to reduce pressure-related tissue damage are recognized as important treatment components. While there are limited definitive studies, the best current evidence and expert opinion suggest the following guidelines.
Guideline #1.1: Establish a repositioning schedule and avoid positioning patients on a pressure ulcer.
Principle: Pressure ulcers are thought to result from compression of soft tissues against a bony prominence. It is reasonable to assume that pressure on an ulcer can result in delayed healing. Patients should be repositioned to relieve pressure over bony prominences. The exact turning interval is not known and is derived empirically. Reductions in pressure incidence have been achieved, but positioning is not universally effective.
Evidence:
- 1
Clark M. Repositioning to prevent pressure soreswhat is the evidence? Nurs Standard 1998 13: 5664.
- 2
Defloor T. Less frequent turning intervals and yet less pressure ulcers. Tijdschrift voor Gerontologie en Geriatrie 2001 32: 1747.
- 3
Knox DM, Anderson TM, Anderson PS. Effects of different turn intervals on skin of healthy older adults. Adv Wound Care 1994 7: 4856.
- 4
Thomas DR. Are all pressure ulcers avoidable? J Am Med Directors Assoc 2001 2: 297301.
Evidence:
- 1
Thomas DR. Management of pressure ulcers. J Am Med Directors Assoc 2006 7: 4659.
Evidence:
Evidence:
Evidence:
Evidence:
Pressure Ulcers: Debridement And Dressings
- Charles F von Gunten MD
- Frank Ferris MD
Background Fast Fact #40 discussed the staging and prevention of pressure ulcers this Fast Fact discusses their management. The first step in deciding how to manage pressure ulcers is an assessment of whether the wound is likely to heal. If the patient has a prognosis of months to years, adequate nutrition, and blood flow to the tissue, then healing is possible. If the patient has a prognosis of days to weeks, anorexia/cachexia, and/or the wound has inadequate perfusion, then symptom control alone is appropriate and uncomfortable/burdensome treatments are not appropriate.
Debridement Always provide adequate analgesia! Necrotic tissue must be removed for ulcer healing surgical debridement is the fastest and most effective method when there is healthy surrounding tissue. Note: If the patient is close to dying, and/or the wound will never heal, then debridement should not be attempted. Debridement gels are applied onto an ulcer under an occlusive dressing , are available for ulcers that do not require surgery or when surgical debridement is incomplete. These products come with or without enzymes to encourage autolytic or enzymatic debridement. For minimally necrotic ulcers, occlusive dressings such as DuoDerm, changed weekly, promote autolysis.
References
Read Also: How To Treat Mouth Ulcers
How Should Pressure Ulcers Be Assessed
Clinicians should take a medical and pressure-ulcer history, including assessment of pain. They should examine and measure the length, width, and depth of ulcers. The presence of exudate, necrotic tissue, eschar, slough, undermining, and tunneling or sinus tracts should be documented. The presence of healing tissue should be noted. The wound should be staged using the National Pressure Ulcer Advisory Panel’s 1 to 4 staging system.18
Nursing Home Abuse & Neglect Resources
Common Cases:
Client Reviews
Nursing Home Law Center, LLC is not a law firm. It is an organization that concentrates solely on helping provide nursing home patients and their families the legal help they need. NHLC LLC has a network of recognized attorneys located across the country who have experience representing clients in all types of nursing home injury cases. References to “NHLC attorneys” or “our attorneys” are references to attorneys within NHLC’s network, and not employees, agents, or partners of NHLC. Please consult the disclaimer page for further information concerning NHLC. All information on this site shall be considered ‘attorney advertising’ and not construed as legal advice. Prior case results should not be relied on when retaining a lawyer.
Also Check: Home Remedies For Stomach Ulcer In Tamil
How Are Pressure Injuries Treated
Pressure injuries can be treated in many ways depending on the stage. Once the stage and severity of the wound is determined, it must be cleaned, usually with a saline solution. After the wound is cleaned, it needs to be kept clean, moist, and covered with an appropriate bandage. There are several different types of bandages your doctor may use to dress the wound. These include:
- Water-based gel with a dry dressing
- Foam dressing
- Hydrocolloid dressing
- Alginate dressing
Sometimes debridement is needed. This is a process of ridding the wound of dead tissue. Debridement is an important part of the healing process. It changes the wound from a long-lasting one to a short-term wound. There are several types of debridement. These methods include:
- Ultrasound: Using sound waves to remove the dead tissue.
- Irrigation: Using fluid to wash away dead tissue.
- Laser: Using focused light beams to remove the dead tissue.
- Biosurgery: Using maggots to eliminate bacteria from the wound.
- Surgery: Using surgery to remove the dead tissue and close the wound.
- Topical: Medical-grade honey or enzyme ointments.
Assessment Of Nutritional Needs
Undernutrition is common among patients with pressure injuries and is a risk factor for delayed healing. Markers of undernutrition include albumin < 3.5 g/dL or weight < 80% of ideal. Protein intake of 1.25 to 1.5 g/kg/day, sometimes requiring oral, nasogastric, or parenteral supplementation, is desirable for optimal healing. Current evidence does not support supplementing vitamins or calories in patients who have no signs of nutritional deficiency.
Also Check: What Helps Ulcers In Your Stomach
Recommendations For Nursing Practice
Based on the findings of this literature review, nurses should almost always question wet-to-dry orders. They are only indicated for mechanical debridement, and should not be used when other methods of debridement are readily available. The improved outcomes of advanced wound care dressings compared to wet-to-dry dressings have been significantly researched, yet continue to be used frequently. Further research is needed regarding why wet-to-dry dressings persist and how to most effectively communicate the evidence supporting moist wound healing.
What Are The Long
If the wound becomes infected, the infection can spread to other parts of the body. Several conditions that may occur if an infection spreads include:
- Cellulitis: An infection of the skin.
- Osteomyelitis: An infection of the bone.
- Bacteremia: An infection of the blood.
- Meningitis: An infection of the brain and spinal cord.
- Endocarditis: An infection of the heart.
Don’t Miss: Remicade Vs Entyvio For Ulcerative Colitis
Who Is At Risk For Developing Pressure Injuries
- People with a limited amount of mobility or a total inability to move. Those in wheelchairs or bedridden are at particular risk and need to be moved or turned regularly.
- Those with prosthetic limbs. If the device does not fit properly, the skin can be irritated and a pressure injury can develop.
- People with a loss of sensation. They are at risk because they may not feel the pressure being applied to the skin. As a result, they may not move, which could worsen the damage.
- Those with malnutrition. Wound healing is slowed when nutritional needs are not met.
- The elderly. As people age, the skin naturally becomes thinner and more easily damaged.
Wound Care Best Practices And The Evolving Role Of Gauze Dressings
Modern dressings are generally non-adherent and ensure appropriate healing through maintaining a moist wound healing environment and maximizing patient comfort.5 Implementing advanced dressings and alternative debridement methods as best practices for wound care will help clinicians maintain a moist healing environment.Impregnated gauze, such as gauze containing substances such as petroleum, honey, hydrogel, iodine, bismuth, and zinc, can decrease trauma and prevent desiccation during dressing changes. It can also decrease moisture loss from the wound, thereby preventing local cooling and its adverse effects.3 It has also been demonstrated that the use of advanced dressings can be more cost-effective than the use of gauze because of the massive decrease in clinician time required for the application of the dressings, even though gauze is generally a far less expensive material.2 When selecting the optimal wound dressing, it should6:
- Maintain a moist wound healing environment.
- Facilitate gas exchange.
- Protect the wound from further trauma.
- Enable easy removal and dressing change frequency.
- Be biocompatible, biodegradable, elastic, and nontoxic.
- Be cost-acceptable.
The idea of scrubbing a wound with gauze has been in practice since the 2000s and was inspired by the effectiveness of brush scrubbing for contaminated injuries. When subcutaneous scrubbing occurs in conjunction with high-pressure washing following surgery, it can be effective at lowering the risk of infection.8
Also Check: Natural Cure For Stomach Ulcer
Say Goodbye To Wet To Dry
Despite the vast amount of advanced wound care products available as well as an evidence-based practice that supports wet to dry dressings are substandard, I still receive daily calls from clinicians reporting new wound care orders for wet to dry dressings to be performed in the home setting, usually twice daily.
What exactly is a wet to dry dressing?
A typical wet to dry is a saline moistened dressing, which is placed in the wound bed. It is left to dry and removed usually every 4 to 6 hours. Removing this dried gauze acts as a mechanical debridement agent.
Now lets discuss what happens to and in the wound with this removal process.
First, non- selective mechanical debridement. When that dry gauze is pulled from the wound bed, it also pulls any tissue that has adhered during the drying process. Often it is newly formed, healthy viable tissue that is removed, causing trauma and/or bleeding to the wound bed as well as increased pain for the patient.
The second thing that occurs is local tissue cooling. Wounds are very picky about the climate of the environment in which they can heal. Cells tend to do their best work at a normal body temperature of 98.6 F. When the wound temperature decreases, it may take up to 4 hours to return to an optimal temperature. During this time, healing stops. Therefore, the more frequent dressing removal, the less time the wound is healing.
What Are The Stages Of A Pressure Injury
There are four stages that describe the severity of the wound. These stages include:
- Stage 1: This stage is discolored skin. The skin appears red in those with lighter skin tones and blue/purple in those with darker skin tones. The skin does not blanch when pressed with a finger.
- Stage 2: This stage involves superficial damage of the skin. The top layer of skin is lost. It may also look like a blister. At this stage, the top layer of skin can repair itself.
- Stage 3: This stage is a deeper wound. The wound is open, extending to the fatty layer of the skin, though muscles and bone are not showing.
- Stage 4: This stage is the most severe. The wound extends down to the bone. The muscles and bone are prone to infection, which can be life-threatening.
Also Check: Is Colitis And Ulcerative Colitis The Same Thing
Common Questions About Pressure Ulcers
This is an updated version of the article that appeared in print.
JAQUELINE G.M. RAETZ, MD, and KEREN H. WICK, PhD, University of Washington, Seattle, Washington
Am Fam Physician. 2015 Nov 15 92:888-894.
Patients with limited mobility due to physical or cognitive impairment are at risk of pressure ulcers. Primary care physicians should examine at-risk patients because pressure ulcers are often missed in inpatient, outpatient, and long-term care settings. High-risk patients should use advanced static support surfaces to prevent pressure ulcers and air-fluidized beds to treat pressure ulcers. Physicians should document the size and clinical features of ulcers. Cleansing should be done with saline or tap water, while avoiding caustic agents, such as hydrogen peroxide. Dressings should promote a moist, but not wet, wound healing environment. The presence of infection is determined through clinical judgment if uncertain, a tissue biopsy should be performed. New or worsening pain may indicate infection of a pressure ulcer. When treating patients with pressure ulcers, it is important to keep in mind the patient’s psychological, behavioral, and cognitive status. The patient’s social, financial, and caregiver resources, as well as goals and long-term prognosis, should also be considered in the treatment plan.
SORT: KEY RECOMMENDATIONS FOR PRACTICE
Multicomponent interventions should be used to prevent pressure ulcers in high-risk patients.
Which Wound Dressing Is Best For Your Pressure Ulcer
Now that weve touched on some of the more common types of dressings used for pressure ulcers, you may be wondering which is the best for your particular situation. The answer will depend on multiple factors including where the pressure ulcer is located, how severe the bedsore is, and the degree of skin and tissue damage. Talk to your health care professional about any pressure wounds you notice on your body as soon as possible.
Recommended Reading: What To Eat If You Have Gastric Ulcer