Support Drainage And Detox
Good drainage is essential for ridding your body of toxins that can compromise gut health. An unhealthy gut thats burdened with contaminants could become a stagnant breeding ground for pathogens.
Ways to support drainage and toxin removal, as well as gut health, include:
- Binders: Binders can help sponge up toxins. They haul out the garbage and give you additional support for your gut.
- Constipation support: Constipation is often involved in IBS. At a minimum, you need to poop daily to eliminate toxins. And pooping 23 times a day is best during detox. Certain herbs support regular elimination.
- Good bile flow: Bile is a primary route for eliminating toxins via your stools. Good bile flow may also reduce SIBO risk.
- Liver-supportive herbs: Liver inflammation often accompanies gut disorders. Herbs that support your liver function may help ease the inflammation of this organ.
Having A Support System Helps
Having a support system means the world with a chronic illness. For me, that’s my amazing mom and my sister-in-law.
Whenever I had flares growing up, my mom tirelessly searched for new recipes that wouldn’t bother my gut. She even followed my restriction diets out of solidarity and fasted with me when I prepped for a colonoscopy. Her support made me feel less alone as a teen, and it still does today.
It also helps to find a friend or support group who understands what you’re going through. My sister-in-law also has UC, and she can relate to everything I endured growing up. Talking with her always lightens my mood and we often text each other UC memes.
Sharing humor may seem like a small thing, but it helps to know someone else relates to your struggles. Plus, you can laugh about it during your next bathroom trip.
Quick tip: If you want to find your own support system, check out online organizations like the Crohn’s & Colitis Community.
What Is Crohns Disease
Crohns disease is the other major disorder under the IBD umbrella. Similar to ulcerative colitis, Crohns disease can cause severe inflammation and sores in your digestive tract. This can result in abdominal pain and diarrhea, which can be bloody.
However, there are distinct differences between the two main types of IBD. Read on to see how they compare.
Read Also: What Can You Take For Stomach Ulcers
Current Treatment And Prognosis
A distinction must be made between CMV infection and CMV disease. Cytomegalovirus infection refers to presence of detectable CMV in the human body, whereas CMV disease relates to symptoms due to CMV. Owing to its latency, CMV infection can be documented in various organs without evidence of organ damage. For instance, CMV has been documented in the urine and saliva of pregnant and immunocompromised patients without evidence of clinical disease. Some have described CMV as an innocent bystander, with the clinical relevance of CMV infection in tissues being unclear. In one study, histologically proven CMV infection was assumed to be the cause of colitis however, only 17 of 44 patients had supporting serologic results, and only 13 of 44 had a positive IgM finding to suggest primary as opposed to latent infection. Some patients could potentially have had colitis from other causes, with the incidental discovery of nonpathogenic CMV infection.
Cytomegalovirus immunoglobulin, either alone or in combination with antiviral medications, is not currently indicated for the treatment of CMV colitis. A small mortality benefit may exist, but there is significant heterogeneity among the studies evaluating its use in CMV disease.
New Study Reveals 1 In 10 Inflammatory Bowel Disease Patients Are Misdiagnosed With Irritable Bowel Syndrome
A new study, published in the latest issue of the UEG Journal reveals that 10% of IBD patients are misdiagnosed with IBS and in 3% of cases the misdiagnosis can persist for five or more years. The case-controlled study, conducted in the UK, assessed the proportion of patients with IBS recorded prior to the IBD diagnosis to reveal the alarming statistics.
Leading IBD researcher and United European Gastroenterology spokesperson Dr Michael Scharl says, IBS has been estimated to affect at least 10% of the population in Europe and it causes distressing symptoms that disrupt normal life. He explains, We have known for some time that there are similarities between symptoms of IBS and IBD, but when it comes to diagnosis and treatment, this differs greatly.
He adds, Misdiagnosis is understandable as many symptoms such as diarrhoea, abdominal cramping and pain are common to both and the specific alarm symptoms for IBD such as bloody stool, weight loss or fever are often absent in IBD patients in the initial phase of their disease. However, increased use of faecal calprotectin testing would help doctors distinguish between inflammatory bowel diseases, such as Crohns disease and ulcerative colitis and non-inflammatory bowel diseases, such as irritable bowel syndrome.
UEG, or United European Gastroenterology, is a professional non-profit organisation combining all the leading European medical specialist and national societies focusing on digestive health.
Recommended Reading: What Foods To Eat If You Have An Ulcer
How To Fix Your Gut Issues
No matter which bowel condition you might have such as IBS or ulcerative colitis thereis hope.
Generally, the solution requires removing toxins and treating chronic infections. Dietary and lifestyle changes may help, too.
Consider the following strategies to help you get a handle on your gut issues:
Symptoms Outside Of The Gi Tract
In IBD, inflammation may occur beyond the gut in the skin, joints, and eyes for examples. The resulting dermatitis, arthritis, and iritis can be as debilitating as the IBD itself. None of these physical disabilities result from IBS, and having IBS does not predispose one to IBD, nor any other structural condition such as cancer, celiac disease, nor diverticulosis. While neither condition will shorten life expectancy, most of those with IBD will require surgery at some time during their illness.
Sometimes psychological disease is thought to be a part of IBS. Certainly, some patients who seek medical attention may also have psychosocial problems that require attention in their own right. However, there is little evidence that this is true of IBS overall, and psychosocial difficulties are found in some people with IBD as well. While many people with IBS complain of social inconvenience, embarrassment, fear of appearing in public, and work loss, these features are more universal and profound in IBD, as the foregoing comparisons imply. While IBD is described as a structural or organic disease, IBS is said to be functional or a disorder of function. None of these terms is entirely satisfactory.
You May Like: Stress And Ulcerative Colitis Flares
What Is Irritable Bowel Syndrome
IBS refers to chronic digestive issues that dont have a clearly identifiable cause. Its estimated to affect up to 15% of Americans.
Symptoms of IBS include unexplained chronic abdominal pain, along with irregular bowel habits. You may have diarrhea, constipation, or alternate between the two.
Getting to a diagnosis of IBS isnt a very straightforward path, though.
First, doctors typically rule out other possible conditions. For example, your doctor may test to see if you have ulcerative colitis, Crohns disease, or celiac disease. After likely causes of your symptoms are ruled out, your doctor may diagnose IBS.
Resolving IBS isn’t straightforward either. That’s because experts aren’t sure what causes it. Theyve only identified factors that may predispose you to the condition. But, knowing risk factors for IBS may give you some clues for remedies.
Some risk factors for IBS include:
Among this list, an often overlooked factor in IBS is parasitic infections. Some parasites interfere with your gut motility, resulting in diarrhea or constipation. They may also trigger abdominal pain, bloating, and neurotransmitter imbalance.
If your attempts to fix IBS have fallen short, you are well-advised to consider whether you might have a chronic parasite infection.
As scientists continue to unravel the mystery of what causes IBS, keep the above list of risk factors in mind. Addressing parasites and other potential culprits may help you conquer the condition.
Other Sibo Risk Factors
Many other factors can affect your chance of SIBO. These include your diet, medication usage, and several disease conditions.
If your diet is high in sugar and other refined carbs, your risk of SIBO may increase. Sugar can shift the balance of your gut microbiome. It favors the overgrowth of harmful bacteria and fungi like candida.
Additionally, if you take heartburn drugs that reduce stomach acid, your risk of SIBO increases. Frequent antibiotic use may also boost your chance of SIBO.
Low thyroid function or hypothyroidism has been linked to increased SIBO risk as well. But, research suggests that this increased risk may stem from taking levothyroxine. Thats a synthetic thyroid medicine.
Some of the other disorders that may increase your risk of SIBO include:
- Crohns disease
- Chronic pancreatitis
All these diseases can impact your digestive tract. They may slow it down and prevent your ileocecal valve from working correctly.
Don’t Miss: Acute Ulcerative Colitis Icd 10
Alicias Story Ulcerative Colitis
“I remember being on the bus back from college one day and felt the most excruciating pain Id ever had in my stomach. I was 17, terrified and in pain”Alicia’s story from diagnosis of Ulcerative Colitis to sharing her story and experiences with thousands as she travels the globe.
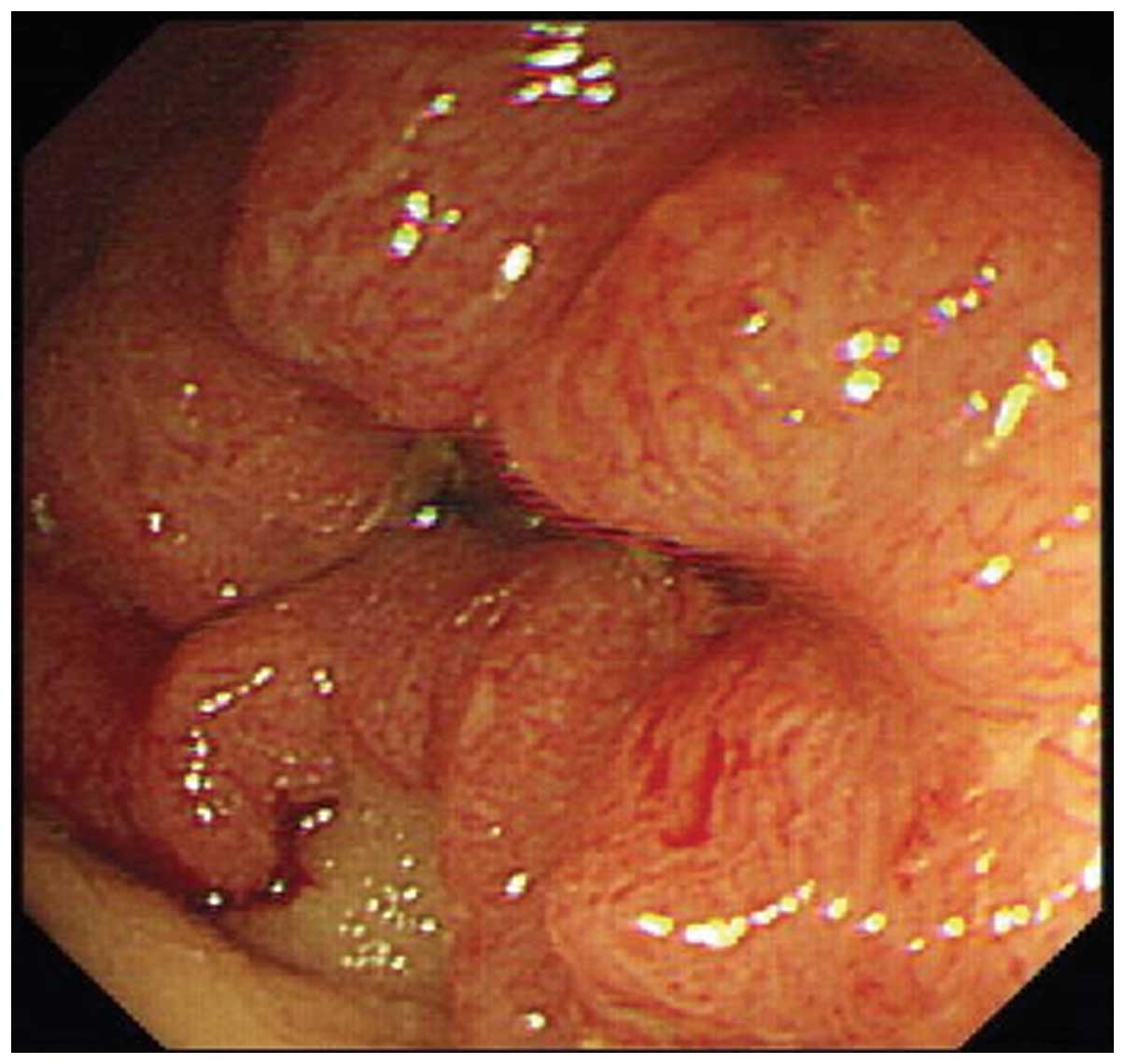
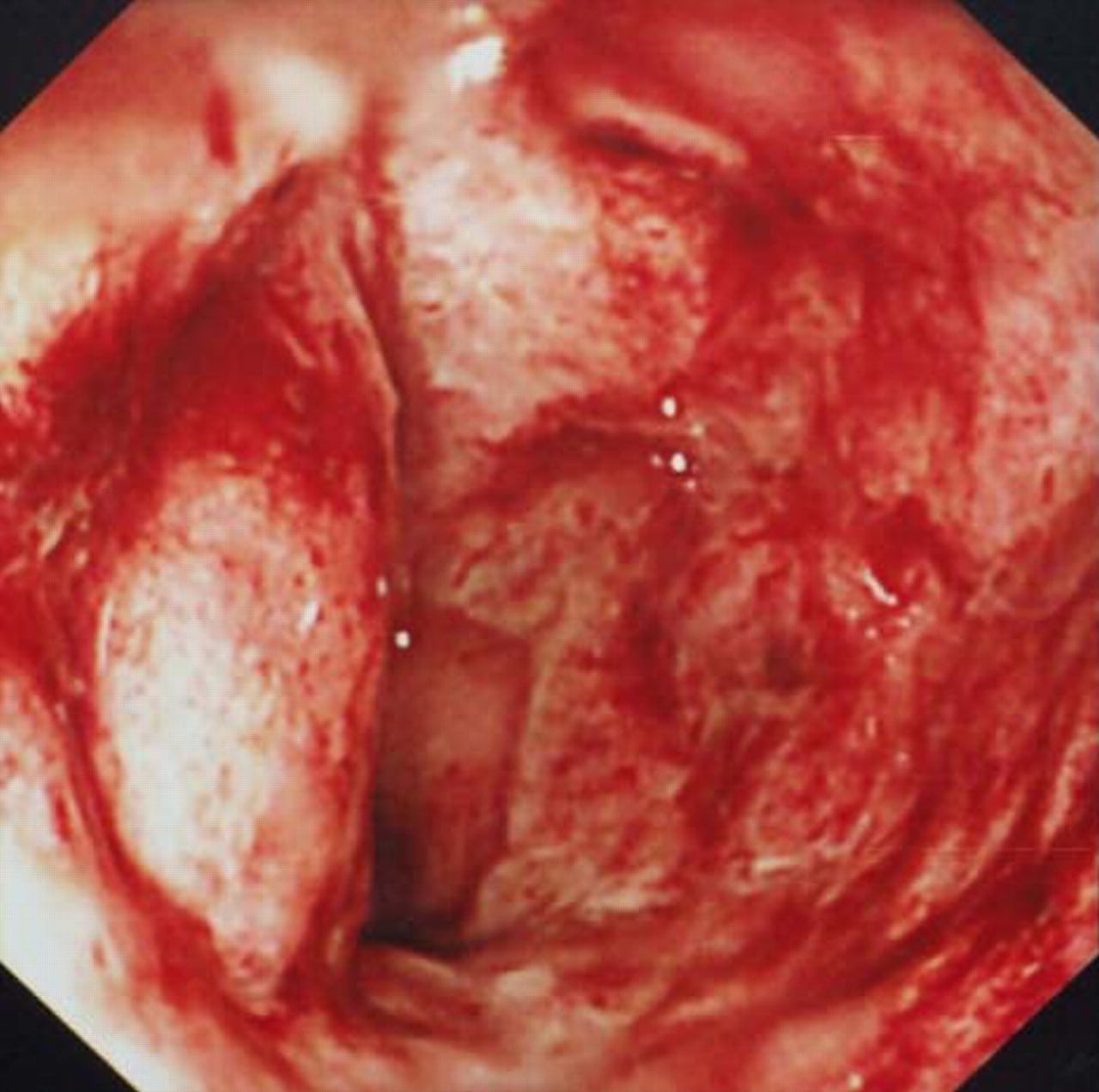
My first memory of Ulcerative colitis was seeing blood in the toilet. I googled it and thought the worst. But I thought itd pass. Days turned to weeks and months, each time I went the toilet more and more blood appeared. Clots. I remember being on the bus back from college one day and felt the most excruciating pain Id ever had in my stomach that I needed to sit down and get off at the next stop. Even this wasnt enough for me to raise my concerns, I was 17, terrified and in pain.
Aged 18, I was diagnosed with Ulcerative Proctitis.
It was a bizarre sensation, I was partly relieved there was an answer to feeling so rubbish but also scared at the information given, confused the specialist addressed the condition like there was no cure. Looking back it took a really long time to comprehend this was my forever.
The next two years was a rollercoaster of one month being OK, the next not so fine, blood, mouth ulcers, fevers, aching joints, abdominal pains & weight loss.
This meant a new treatment plan immunosuppressant Azathioprine. The first few weeks taking this medication made flares seem like a walk in the park. After persevering though, I slowly started to gain my normality back.
Ibs Vs Ibd: Two Very Different Illnesses
It is of vital importance to distinguish these two very different gut conditions. While both are chronic, the overall treatment and prognosis are very different. There are other important considerations. Because so may people have IBS, it is not surprising that some will also acquire IBD. That is, they may occur in the same patient due to chance. It is therefore crucial that the IBS symptoms in these patients not be confused with those due to IBD. The powerful, often expensive, sometimes-toxic drugs employed to treat IBD will not improve IBS symptoms. There are many reported instances where IBD has been misdiagnosed as IBS for years until finally the diagnosis is made. A more likely explanation is that IBS was present first and the IBD started later.
Finally, both IBD and IBS may be mistaken for other diseases such as appendicitis, diverticulitis, and chronic gut infections. Careful attention to the medical history and a thorough physical examination should avoid any such confusion.
Both IBD and IBS trouble many people. However, because of its propensity to damage the gut and other organs, IBD may produce disfigurement and sometimes-permanent physical disability. While there is no doubt IBS patients can suffer greatly from symptoms, their outlook is better than those who have IBD. A perusal of Table 1 illustrates many important reasons to distinguish the two conditions.
Read Also: How To Treat Unstageable Pressure Ulcer
The Trouble With Misdiagnosis
From January 2017 to June 2017, I had a flare-up throughout my GI tract. On June 8, I had an endoscopy and a colonoscopy. The scopes showed inflammation in my esophagus, gastritis, and signs of active disease in my ileum and colon. By the end of June, I was hospitalized.
A team of GIs revisited my health records. I was taking HUMIRA at the time, but unfortunately, my body was building antibodies towards the medication.
I remember lying in my hospital bed when one of the GIs on call came to my room. After a discussion with several of his colleagues, he said my results and symptoms were more consistent with Crohns disease.
The doctors also wanted to change my treatment. They wanted to try a biologic called Stelara.
UC and CD are very similar however, they have slight differences, and it is important to get the right diagnosis. Heres a perfect example of why:
Even though my doctor had prescribed Stelara, it took about four months to get it approved by my insurance company because Stelara was only approved for people with Crohns disease.
Sure, the doctors finally agreed that I had Crohns disease. But most of my medical reports at the time said ulcerative colitis. So it was a challenge to prove to my insurance company that I actually had CD.
What Other Problem Can I Have With Treatment
Misdiagnosis isnt the only problem you can face with treatment, there are two other ways you can encounter difficulties.
Firstly, you might have contended with delayed diagnosis, which is when a doctor does not carry out appropriate testing over an extended period of time despite your symptoms. This can mean your condition gets worse or becomes harder to treat because it has developed so much further.
Secondly, you may face poor treatment, which means you may be diagnosed correctly but are still given incorrect treatments or are not given check-ups to monitor your condition. For example, if you suffer from ulcerative colitis your chances of developing bowel cancer are increased and you should have regular check-ups to monitor your health.
Don’t Miss: Bowel Ulcers Signs And Symptoms
Treat Parasites And Other Chronic Infections
As mentioned above, parasites and candida overgrowth sometimes are at the root of gut conditions. In fact, sometimes gut issues are misdiagnosed as IBD when theyre really parasite infections.
You can fight back against parasites with immune-supportive herbs.
Additionally, you can use certain essential oils to help you get rid of parasites.
Finally, if candida overgrowth is contributing to your gut issues, consider a candida cleanse. That may help reduce the burden on your digestive tract.
It Can Make Social Events With Food Stressful
Food often dominates family, friend, or coworker gatherings, which can be tricky when you have an invisible illness like UC.
Not everyone understands the challenges of chronic GI issues. People might look at you funny if you’re the only one not happily chowing down at the potluck, or you bring a lunchbox to a catered dinner.
But even when I explain, not everyone understands or accepts my reasons perhaps because they don’t understand how much food can influence UC.
A few bites of the wrong food could leave me doubled over with cramps or make me pull over and dash for a bathroom while driving home. If I say “No, thanks” to a plate, I’m not trying to be rude. I’m just trying to stay on my gut’s good side.
Don’t Miss: What Does An Ulcer Look Like In The Stomach
Liver Health And Sibo Risk
Your liver may not be the first thing you connect with SIBO. Yet, it has important links to an increased risk of the condition.
People with liver cirrhosis extensive scarring tend to have slower gut motility. This means your gut contents sit in the small intestine longer. That gives microbes more time to feed on nutrients in your gut and multiply in number. In other words, they overgrow.
One study found that nearly half of people with liver cirrhosis had SIBO, compared to less than 10% of otherwise healthy people.
Poor liver health may also lead to backed-up bile ducts. When your bile ducts are clogged, less bile gets into your small intestine. Lower levels of bile in your gut are linked to bacterial overgrowth. That could be because bile has anti-microbial properties.
Additionally, parasites can interfere with your liver health by clogging your bile ducts. For example, Ascaris lumbricoides roundworms and fasciola flukes have commonly been found in bile ducts.
To recap, poor liver health and parasites can slow your gut motility and reduce bile levels in your gut. That may increase your risk of SIBO.
C Diff Infection And The Effect On Ulcerative Colitis
C. diff infection is one of the most common complications to watch for if you have ulcerative colitis. It can happen even if you are not taking antibiotics, especially if you take steroid medications to keep the disease under control. A database of patients with IBD showed 10% will have at least one C. diff infection over the course of their lifetime. Half will have more than one.
When people with ulcerative colitis get a C. diff infection, they are more likely to need a colectomy, an operation to remove part or all of the colon. They also have a higher risk of developing complications after surgery, and they have a higher death rate.
Recommended Reading: Plant Based Diet Ulcerative Colitis
Whats The Outlook For C Diff Infection In Ulcerative Colitis
Since C. diff infections can cause serious complications for people with ulcerative colitis, the outlook can be challenging. While not common, C. diff infections do cause more deaths among people with IBD than those without, especially if they need surgery. They also tend to have to stay longer in the hospital and need more surgeries. But with vigilance and treatment, most people start to feel better within 3 days of starting treatment.
If you have ulcerative colitis and have any symptoms of C. diff infection, call your doctor or health care team right away so you can start treatment as soon as possible.
Show Sources