What Can I Expect From The Test Results
Your doctor will typically talk with you about your results after the procedure, and they will be either negative or positive. Negative results mean nothing abnormal was found during the test. Positive results mean that polyps or other abnormal tissue was found during the exam. If youve only had a sigmoidoscopy, your doctor may want to schedule a colonoscopy to see the rest of your colon, per the Mayo Clinic. If your colonoscopy results were positive, your doctor will talk with you about a treatment plan moving forward.
What Else Should I Know
People with ulcerative colitis are at risk for colon cancer, which is related to chronic inflammation. So they should get a colonoscopy every 1-2 years, starting about 10 years after diagnosis.
Kids and teens with ulcerative colitis may feel different and not be able to do the things their friends can do, especially during flare-ups. Some struggle with a poor self-image, depression, or anxiety. They may not take their medicine or follow their diet. It’s important to talk to the doctor or a mental health provider if you’re concerned about your child’s mood, behavior, or school performance.
Parents can help teens take on more responsibility for their health as they get older. Encourage teens to take their medicine, take care of themselves, and manage stress in positive ways. Yoga, meditation, breathing and relaxation techniques, music, art, dance, writing, or talking to a friend can help.
You also can find more information and support online at:
Some Of The Common Symptoms Of Ulcerative Colitis Are:
- Frequent Diarrhea
- Loss of appetite
The disease may also cause other health issues like joint pain, eye problems or the liver disease. Small ulcers in the lining of the colon could cause bleeding and the passage of mucus. Often the symptoms of ulcerative colitis might disappear, but they have a tendency to relapse. About 0.5 to 1% people out of a 100 may suffer from these symptoms all the time.
Read Also: What Is Ultra Ulcerative Colitis
Alarm Symptoms Of Ulcerative Colitis:
If you are already diagnosed with ulcerative colitis, there are several alarm symptoms to look out for. A change in your ulcerative colitis symptoms may mean that additional treatment is needed. Talk to your doctor immediately if you experience a new symptom, a change in your current symptoms or any of the following:
- An unusual amount of cankers or sores in your mouth
- Unexplained or unintentional weight loss
- Failure to gain weight
- Delayed puberty in teens
- Anemia this blood condition results in fatigue and weakness. It is usually caused by heavy blood loss or a lack of dietary iron
- Rectal bleeding
- Nausea / vomiting inability to keep food / drink down
How Do Doctors Diagnose Ulcerative Colitis
To diagnose ulcerative colitis, doctors review medical and family history, perform a physical exam, and order medical tests. Doctors order tests to
- confirm the diagnosis of ulcerative colitis
- find out how severe ulcerative colitis is and how much of the large intestine is affected
- rule out other health problemssuch as infections, irritable bowel syndrome, or Crohn’s diseasethat may cause symptoms similar to those of ulcerative colitis
Read Also: Off Loading Shoe For Heel Ulcer
Oral Vs Rectal Treatments
Most physicians prescribe ulcerative colitis patients oral versions of 5-ASAs or corticosteroids, since this is a patient-preferred delivery method of medication. However, even if they have a specially designed release mechanism, they might not reach and treat the area where the disease is most active.
For example, when you apply sunscreen to your skin, you need to make sure that you cover every exposed part to protect it from the sun. Similarly, when applying these treatments to your rectum and lower colon, you need to make sure that the product covers all of the inflamed areas.
Oral tablets might not be the optimal way to reach the end of the colon, where stool and the fact that ulcerative colitis patients have diarrhea, might interfere with its effectiveness. Unfortunately, this is also the area in the colon where a flare usually starts. The best way to reach this particular area is by inserting the drug directly into the rectum.
Rectal preparations are particularly good at treating urgency and bleeding, symptoms that often are very bothersome. A positive response often occurs within days of treatment.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Also Check: Types Of Steroids For Ulcerative Colitis
Patient Profile: Jessica Adani
Jessica Adani, 37, has an active case of Crohns disease for a dozen years. She is director of the Annual Fund and leadership giving at the Fenn School in Concord, MA. She lives in Wayland, MA, with her husband, Jon, and their three -year-old son, Gavin. Adani is a member of the CIRCLE programs patient advisory board.
Can I Prevent Ulcerative Colitis
There is currently no known way to prevent or cure for ulcerative colitis but the proper strategy for managing your disease can help you lead a happier, healthier, fulfilling life.
The exact cause of ulcerative colitis is unknown. However, it is believed to be due to a combination of factors, including a persons genes and triggers in the environment. This interaction of genetic and environmental factors activates an abnormal response of the bodys immune system.
Normally, the immune system protects the body from infection. In people with ulcerative colitis, however, the immune system can mistake microbes , food, and other material in the intestines, as invading substances.
When this happens, the body launches an attack, sending white blood cells into the lining of the intestines where they cause inflammation and ulcerations.
You May Like: When Was Ulcerative Colitis Discovered
Eat This: The Best Ulcerative Colitis Diet Foods
People with ulcerative colitis are more likely to experience vitamin shortages due to the possibility that they wont be able to eat a variety of meals. Other elements, like issues with nutrition absorption, may also play a role in this.
Anyone with UC must consume meals abundant in vitamins and minerals, such as iron, calcium, and vitamin A, to make sure they obtain enough nutrients.
For those with ulcerative colitis, the following foods might be better options:
Fruits low in fiber: Bananas, watermelons, peaches, papayas, etc.
Cooked vegetables: Those who suffer from UC may be able to tolerate cooked, skinless, non-cruciferous vegetables. These consist of asparagus tips, cucumbers, and squash.
Probiotic foods: Include yogurts, which have probiotics that are active. Digestion may be aided by the good bacteria in them. According to several studies, taking probiotics frequently can help lessen the symptoms and flare-ups of colitis.
Omega-3-rich foods: Consuming foods high in omega-3 fatty acids, such as salmon, walnuts, flaxseed, and chia seeds, may be beneficial.
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
Also Check: Fasting To Heal Ulcerative Colitis
Symptoms Of Ulcerative Colitis
Most symptoms are related to the inflamed rectum. The inflammation does not allow the rectum to stretch or store properly. This affects a patients ability to sense what is in the rectum, making them feel the urgency to use the bathroom more often. Very little stool will pass during these many trips to the bathroom â sometimes just mucus and blood.
When inflammation spreads to the lower part of the intestine, people can feel paradoxically constipated. The reason for this is that the bowel above the inflammation is working fine, but when it gets to the inflamed area, it cant stretch like it is supposed to. That can cause an internal back up, causing bloating and gas.
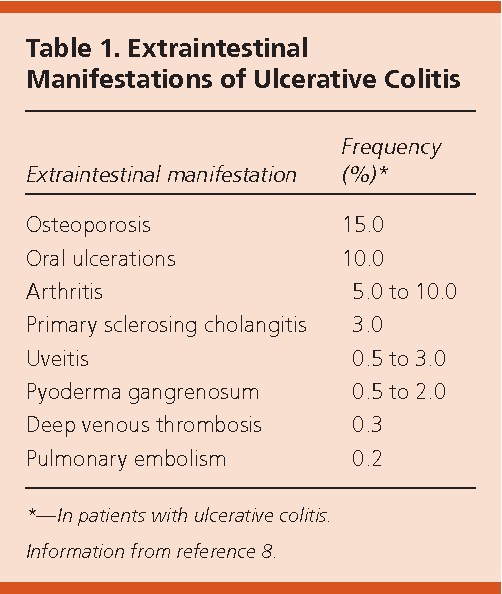
Some people may experience extraintestinal manifestations, which refers to inflammation in other parts of their body. The most common manifestation is symmetrical joint pain, which occurs on both sides of the body, often in smaller joints. Other less common types include skin and/or liver inflammation. Extraintestinal manifestations are connected to the bowel inflammation and will get better if the inflammation in the large intestine is treated.
What Procedures And Tests Diagnose Crohns Disease And Ulcerative Colitis
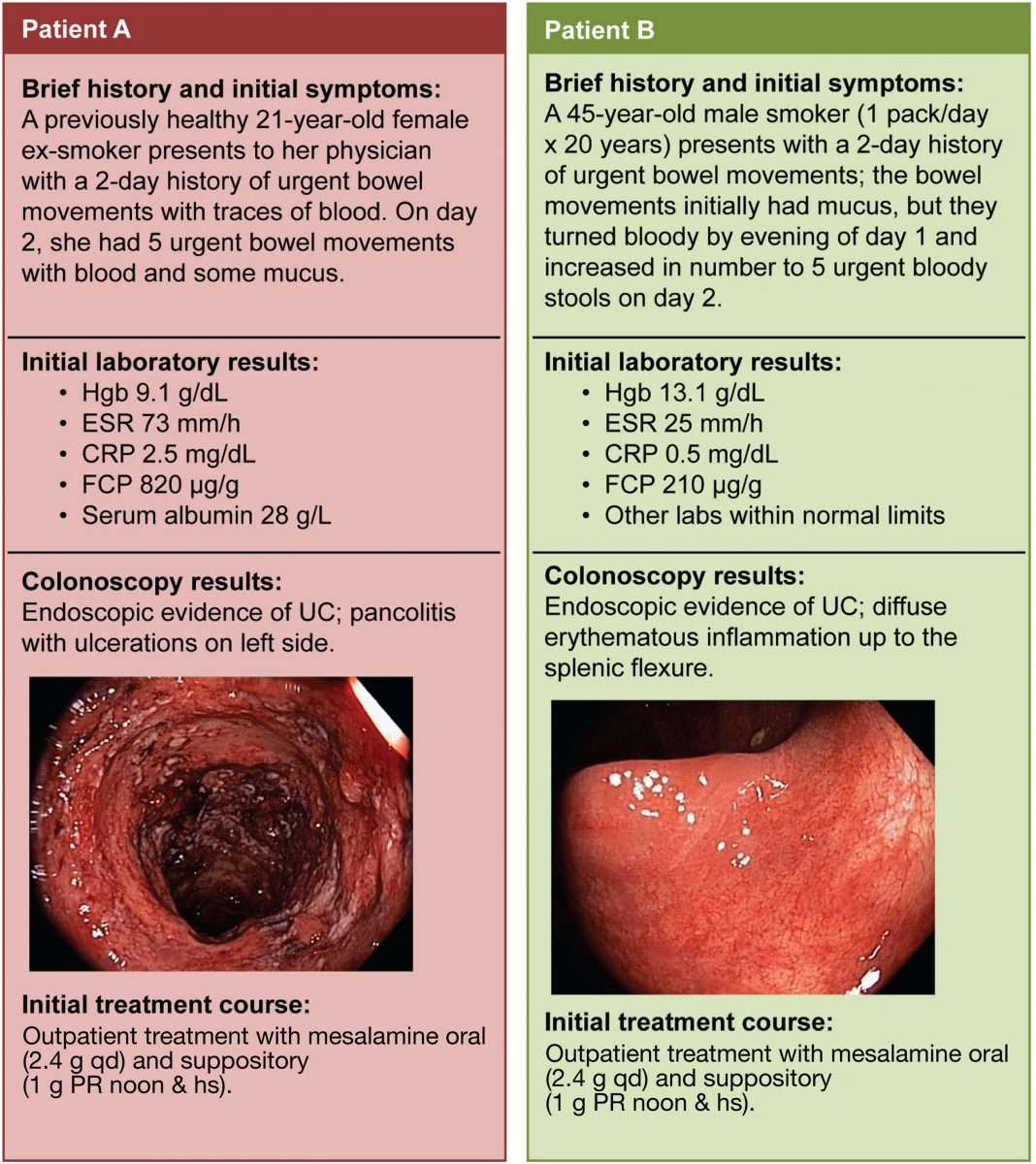
Doctors diagnose ulcerative colitis by endoscopy . During this procedure the doctor can see and take pictures of the patients abnormal gut mucosa , and the presence of continuous disease . Other blood tests and imaging tests like CT scan or MRI are used, but these tests are not definitive.
Doctors use the same procedures and tests to diagnose Crohns disease. However, they also use small bowel studies, colonoscopy, and upper GI endoscopy to identify the abnormal gut mucosa that usually occur in multiple areas anywhere in the intestinal tract. These areas are not continuous, but are separated by normal areas of intestinal mucosa that distinguish them from ulcerative colitis lesions.
As with Crohns disease, nutrition is important if you have ulcerative colitis because symptoms of diarrhea and bleeding can lead to dehydration, electrolyte imbalance, and loss of nutrients. It may be necessary to take nutritional supplements if your symptoms do not allow you to eat a nutritionally balanced diet. Talk to your health-care professional about what supplements to take.
Recommended Reading: Icd 10 Stage 4 Sacral Ulcer
Recommended Reading: Signs Of Having A Stomach Ulcer
What Ulcerative Colitis Treatments Should You Consider After A Diagnosis
We could write a whole article on treatments for ulcerative colitis , but know this: The majority of patients can get control of their disease with medical therapy, Dr. East says. About 15 out of 100 patients may need surgery by 10 years after diagnosis, but this varies by extent of inflammation. New drugs are making the need for surgery less common.
Biologics, which are powerful medications made from living things that are delivered via injection, are very effective at controlling the inflammation associated with ulcerative colitis, and are based on your own antibodies, Dr. East explains. They have the ability to bind to specific molecules involved in triggering inflammation, and have revolutionized treatment of UC and other autoimmune disorders, he says.
Dr. East says lots of patients see a change for the better in two to four weeks. In some cases, a fast-acting drugsteroids, for examplemay be used to get control quickly and then a slow-acting maintenance therapy takes over. Maintenance medications are considered safer than steroids for longer term use.
For some people, the internal J-pouch just wont work. Surgeons create an opening called a stoma in the abdomen, and an external pouch does the waste collection.
How Can I Tell If I Have Ulcerative Colitis Or Crohns Disease
Its important that you, your healthcare provider, and a GI specialist work together closely to figure out whats causing your symptoms. This is especially important since the symptoms of Crohns disease and ulcerative colitis can be similar. Your providers may check blood work and a stool sample. To get an accurate diagnosis, your GI specialist may do a colonoscopy, where a camera is pushed into the colon. Your provider will look at the inside of the colon and take tissue samples, which are important for making the right diagnosis. Your providers might get a CT scan or an MRI of your abdomen to check for complications related to your condition.
Recommended Reading: Ulcerative Pancolitis With Rectal Bleeding
Also Check: Home Remedies For Stomach Ulcers During Pregnancy
Diet And Lifestyle Changes
Although diet and stress do not cause ulcerative colitis, there may be times when changes in your lifestyle may help control your symptoms and lengthen the time between flare-ups.
The following changes may help to ease your symptoms:
- Limit milk/dairy products. If you are lactose intolerant , milk and dairy products can produce symptoms of excess gas and diarrhea.
- Restrict intake of certain high-fibre foods: such as nuts, seeds, and raw vegetables.
- Limit intake of caffeine, alcohol, carbonated drinks and fatty foods.
- Eat small, frequent meals, rather than large meals.
- Exercise regularly to promote movement of the colon and reduce stress.
- Minimize stress. Yoga, meditation and slow, relaxed breathing techniques can help people with ulcerative colitis manage stress.
Ask your doctor or pharmacist if one of these formulations may be right for you. It is important to take the probiotic in the dose and duration recommended by the manufacturer to achieve the best results.
Living Positively With Ulcerative Colitis
Ulcerative colitis is a chronic condition with symptoms that can disappear and then flare up again throughout your life. Living with the unpredictable nature of ulcerative colitis can pose physical and emotional challenges that may seem overwhelming at times. However, there are several things that you can do to contribute to your health and well-being.
Be informed, proactive, and involved in your care. By establishing a solid partnership with your health care team, developing coping skills, and maintaining a positive outlook, it is possible to stay healthy and happy, despite living with ulcerative colitis.
Also Check: Foods To Avoid With Ulcers And Gastritis
Tests Before Treatment Initiation
In addition to the tests used for diagnosis, some specific tests are recommended before treatment initiation. The European Crohns and Colitis Organisation recommends that pretreatment laboratory testing include electrolyte, renal function, iron level, immunization status, and vitamin D tests. See Monitoring for tests used to monitor treatment.
Anti-JC Virus Antibodies
Testing for antibodies to JC virus is recommended in patients with CD natalizumab should be used for CD treatment only in patients negative for anti-JC virus antibodies.
Thiopurine Therapy-Related Testing
Pharmacogenetic testing before treatment initiation may be helpful to guide therapeutic decisions, particularly because treatment failure due to individual differences in medication response is not uncommon in IBD. Thiopurine drugs are commonly used in treating IBD.
The American Gastroenterological Association recommends either phenotype or genotype testing in adults beginning thiopurine therapy.TPMT and NUDT15 gene variants as well as reduced TPMT enzyme activity are associated with a greater risk of myelosuppression in response to treatment with thiopurines due to accumulation of active thiopurines. Phenotype testing should not be performed in patients already receiving treatment with thiopurines because results will be falsely low. In addition, the current TPMT phenotype may not reflect the future phenotype, particularly in patients who received blood transfusions within 30-60 days of testing.
What Complications Are Associated With Ulcerative Colitis
There are some complications related to ulcerative colitis. Possible complications include:
- Severe bleeding
- Perforated colon
- Toxic megacolon
People with ulcerative colitis are also at increased risk of developing colon cancer. The risk of colon cancer is related to the length of time since you were diagnosed and how much of your colon is affected by inflammation. However, a regular examination by your doctor and colorectal cancer screening tests can help to reduce the risk of cancer and detect problems early.
Also Check: Can You Have An Ulcer In Your Esophagus
What Is Ulcerative Colitis
Ulcerative Colitis is a relapsing inflammatory bowel disease, a chronic health condition in which the small or large intestine swell up or the lining of the large intestine spots ulcers. Very often the disease affects the sigmoid colon i.e. lower part of the intestine and the rectum. However, the ulcerative colitis is also known to affect the entire colon. In this case, the more the colon is affected the worse the symptoms of the disease will be.
What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Read Also: Calcium Alginate For Pressure Ulcers
How Do We Diagnose Ulcerative Colitis
The Digestive Health Center at Stanford Health Care delivers expert diagnosis for all forms of inflammatory bowel disease, including ulcerative colitis. Part of what makes Stanford different is our expertise in measuring the degree of intestinal injury for each patient. This helps us understand the severity of your condition and how best to treat it.
Daisys Story: Symptoms And Medical History
I was 16 years old when I first noticed symptoms that I later found out were due to ulcerative colitis. The first symptom I noticed was severe fatigue, but I put this down to the exams I was taking at the time. I was also noticing abdominal pain more frequent bowel movements, and I was also passing blood. I noticed mucus in my stools and was experiencing frequent bouts of diarrhea.
At first, doctors thought that my symptoms were happening because of hemorrhoids, a stomach bug, parasite, or possibly a small tear. As my exams finished and my stress levels decreased, my symptoms became less noticeable too. However, they still persisted, and I was admitted to the hospital when I began to lose weight after not being able to eat drink.
When the doctors asked my mother and me about my family history, we explained that bowel cancer had affected some family members in the past. The doctors then ordered some blood and stool tests to investigate further.
Read Also: How Do You Develop An Ulcer