Feeling Comfortable With Your Doctor
Its not always easy to talk about your bowel habits. Talking about poop can be embarrassing, and many people may not be ready to open up to their doctor about it.
Others may ignore the changes to their stool or think that nothing is wrong. However, ignoring symptoms will only make things worse.
Your doctor has studied the gastrointestinal tract along with all that it does and produces. They have seen and heard it all. Nothing you say about your bowel symptoms is going to offend or shock them.
Its part of their job to know about any changes in your symptoms. Your doctor is there to help you, not to judge you.
You dont have to know any fancy medical terms when talking with your doctor about your symptoms. Share your concerns and any changes in your bowel habits you have noticed. Talking with them about changes in your stool can only help get you closer to resolving the problem.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
What Does Skinny Poop Indicate
While narrow or pencil-thin stool is not always a sign of constipation, it may be if your poop doesn’t normally look that way. Constipation is usually caused by a lack of fiber in your diet or not enough exercise. Other causes include pregnancy, travel, use of some medications, and changes in your hormone levels.
Read Also: Is Oatmeal Ok To Eat With Ulcerative Colitis
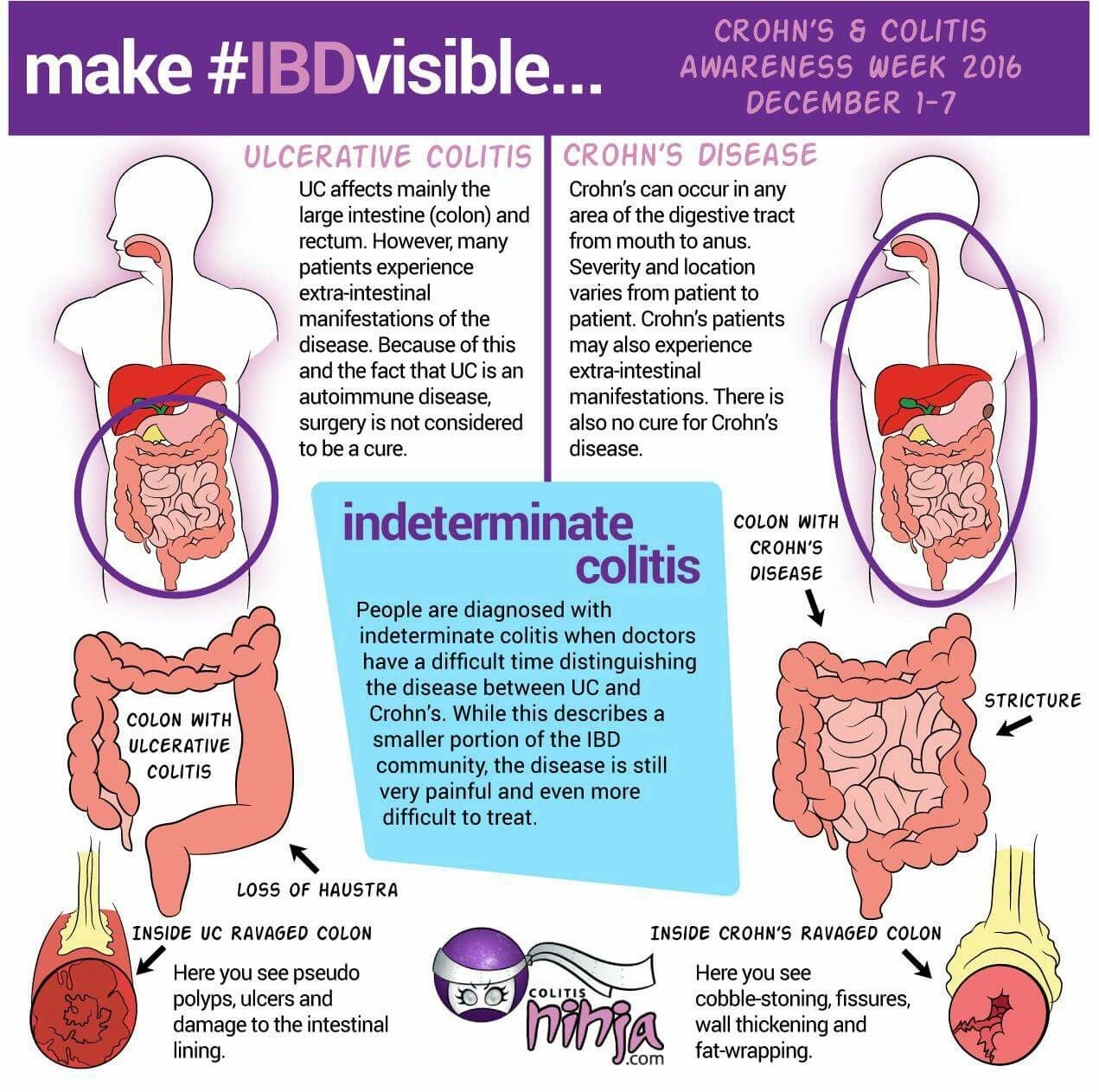
How Does Ibd Affect Pregnancy
IBD can affect your chances of getting pregnant and your symptoms during pregnancy. Pregnant women with IBD may have a high-risk pregnancy.
- Before you get pregnant: You may have more trouble getting pregnant during a flare-up . Also, if you have IBD, talk to your doctor about your risk of problems during pregnancy. If you have a flare-up during pregnancy, you have a slightly higher risk of premature birth, low birth weight, and cesarean delivery than women who do not have IBD.30
Your doctor may also change the type or amount of the medicine you take. Some medicines, such as methotrexate and thalidomide, cause birth defects and other health problems and should not be taken while you are pregnant or breastfeeding.31 If you might become pregnant, talk to your doctor about any medicines you take.
- During pregnancy: Some women say their symptoms get better during pregnancy, but others say they get worse. Women whose IBD is in remission before getting pregnant are more likely to stay symptom-free during pregnancy.31
Ulcerative Colitis Can Take A Toll On Your Mental Health Too
Being told you have a chronic illness can feel like someone has just rerouted the course of your whole life. I went through my own acceptance process, Skomski says. I definitely went through a period of questioning if my life would ever be normal. With time, processing the reality of having ulcerative colitis became easier. I had to learn there’s nothing wrong with me it’s just part of who I am, Skomski says. You have to do a lot of mental work to flip the way you perceive it because otherwise it can really eat away at you.
Dealing with the symptoms can also be mentally and emotionally taxing. The psychological side of the pain is a lot worse than the actual physical sensation, Sam says. It’s when you feel like it’s never going to end, or you’re going to be stuck in that high level of pain for a long period of time, or that no one gets how hard it is to deal with it. This has led to constant vigilance about her health. It’s very hard for me to not be closely monitoring my body 24/7, Sam says. The catch-22 is that stress is definitely a trigger for me.
Don’t Miss: What Will Help Stomach Ulcer Pain
Can Ibd Lead To Other Health Problems
Yes. IBD can lead to other health problems. Some of the conditions include:
- Iron-deficiency anemia.22 Iron-deficiency anemia happens when your level of healthy red blood cells, which carry oxygen to all the parts of your body, is below normal. This can happen because of blood loss from your digestive system.
- Dehydration or malnutrition.23 Diarrhea and cramping pain can make it harder to eat or for your body to get the nutrients it needs. You may need an IV or feeding tube to replace lost fluids or nutrients.
- Toxic megacolon. Toxic megacolon happens when the large intestine swells quickly and stops working. Toxic megacolon is serious and can cause severe pain and even death.24
- Colon cancer. Crohn’s disease can raise your risk of colon cancer.25 Talk to your doctor about your risk.
- Weak bones.26 Crohn’s disease can cause bone loss and osteoporosis. Medicines to treat ulcerative colitis may also lead to bone loss.
- Inflammation inside your body. IBD can cause liver problems, gallstones, and pancreatitis .27
- Kidney stones. Kidney stones are small, painful stones, sometimes formed from oxalate in the kidneys. They are more common in people with Crohn’s disease.28
Some of these other health problems get better when IBD is treated. Some other health problems must be treated separately from IBD.
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Don’t Miss: Stage Iv Sacral Decubitus Ulcer
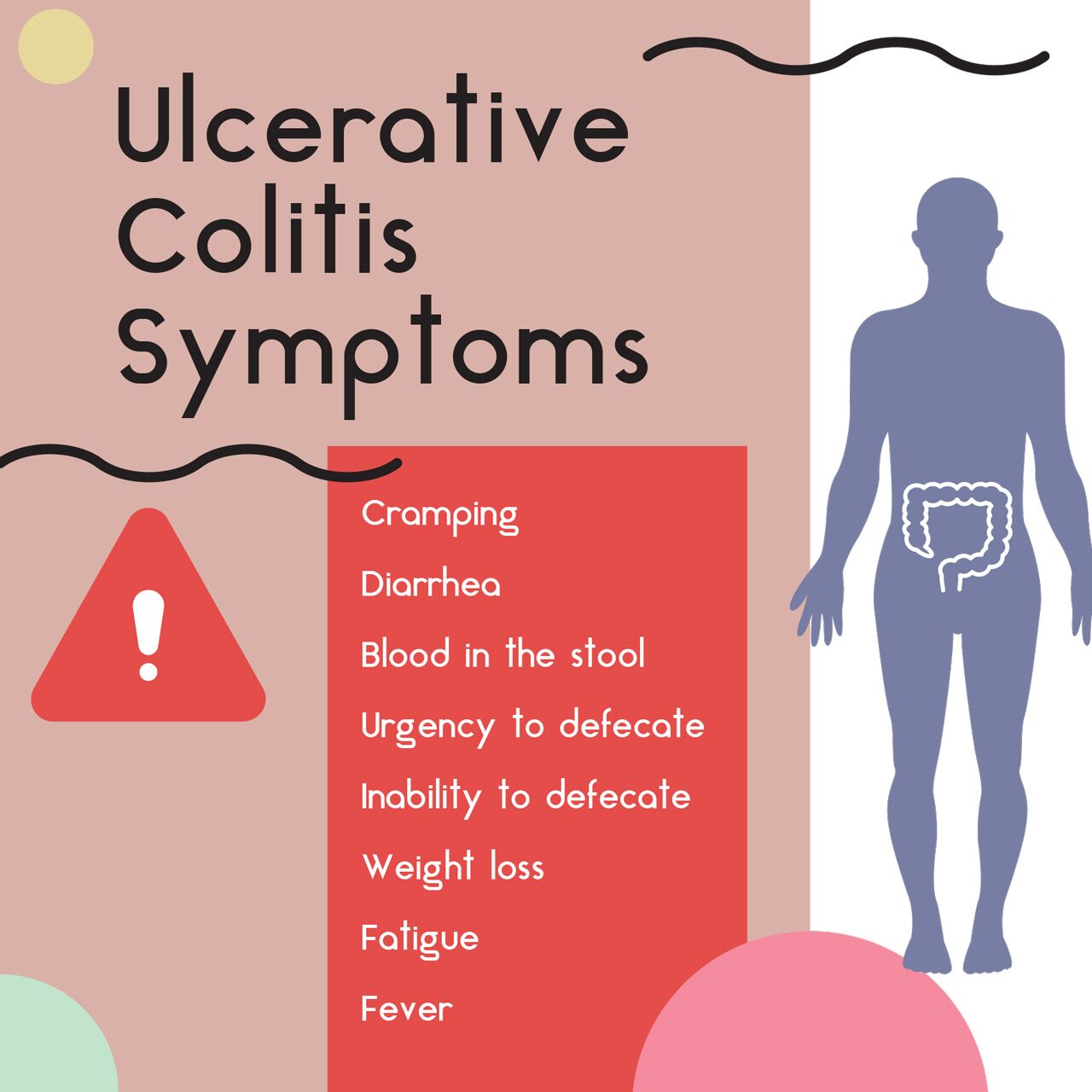
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medicine, such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. But more severe flare-ups need to be treated in hospital.
If medicines are not effective at controlling your symptoms or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
Read Also: Pediatric Ulcerative Colitis Treatment Guidelines
Pain Prevalence And Associated Factors
Slightly more than half of the entire group endorsed at least some pain over the previous two weeks before or during their index visit, with 108 people reporting a SIBDQ Pain Score of at least 4 . Considering the emphasis on frequency rather than severity, we correlated the SPS with the pain severity rating of the Colitis Activity Index, which showed a significant relationship between the two measures . Significantly more women than men described their pain as more frequent . Of note, 16 patients used opioids at the time of their index visit. Abdominal discomfort was the main reason for opioid use in 6 of these individuals, with the remaining patients receiving pain medications for joint, back, bone or muscle pains or chronic pancreatitis . In the remaining patients, no reason for opioid therapy could be identified. Opioid use was significantly more common in patients rating their pain as frequently or constantly present compared to those with no abdominal pain .
Abdominal Pain Prevalence in UC Patients with SIBDQ Scores. The histogram shows the distribution of pain scores, which are inversely related to pain frequency. The insert defines the fraction of patients with and without pain.
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
You May Like: Ulcerative Colitis And Lactose Intolerance
You May Like: Surgical Management Of Ulcerative Colitis Ppt
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Other Ulcerative Colitis Symptoms
Ulcerative colitis causes rectal and abdominal pain, but its not the only condition that does . UC pain is chronic, meaning its either continuous or flares up repeatedly over time.
Chronic gut pain isnt the only symptom of UC though, and if youre experiencing it with the following seek out a medical professional:
- A noisy/rumbling gut
Also Check: How To Determine Stomach Ulcer
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
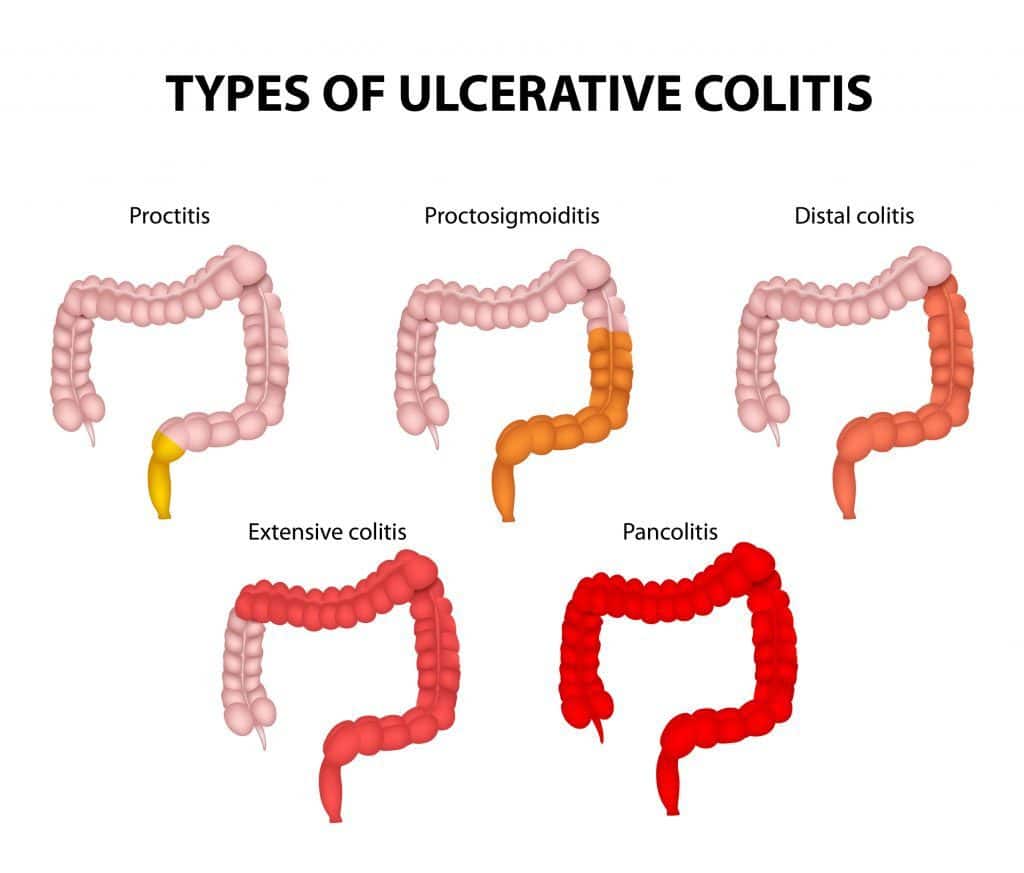
Digestive Changes In Ulcerative Colitis
Ulcerative colitis is a chronic condition, meaning it comes on slowly over a long period of time. Currently, there is no known cure for UC.
With UC, inflammation and ulcers develop on the lining of the large intestine . Sometimes the rectum is affected, as well.
This inflammation can cause changes in bowel habits, including urgency, diarrhea, blood or mucus in the stool, and abdominal pain. When your large intestine is inflamed, it contracts and empties often, which is why you may have urgent bowel movements and diarrhea.
When chronic inflammation damages the lining of your colon, ulcers can develop. The ulcers can bleed, leading to blood in your stool. If you regularly lose a lot of blood in your stool, you might develop anemia .
Though diarrhea is more common, some people with UC experience constipation. Inflammation limited to the rectum, known as ulcerative proctitis, may result in constipation.
Other symptoms of UC include painful bowel movements, nausea, vomiting, fatigue, unintentional weight loss, and fever.
Recommended Reading: Can Ulcerative Colitis Cause Heart Problems
Ulcerative Colitis And Joint Pain
When you have ulcerative colitis , its normal to have pain in your abdomen, along with diarrhea and other gastrointestinal symptoms.
Up to 30 percent of people with UC also have arthritis, which is characterized by swollen, painful joints.
Heres a look at the connection between UC and joint pain, as well as what you can do to protect your joints if you have UC.
‘ulcerative Colitis Is Painful Crippling And Humiliating’
As I crouch on the floor, doubled up in pain and clutching my stomach, the realisation that I am in the middle of a country park far from civilisation and a toilet hammers away in my head. It is a beautiful day in early summer the kind that draws everyone out into the glorious sunshine. But here I am, with my son, partner, his friends and their children, desperately wishing that I had stayed at home.
I was diagnosed with ulcerative colitis at the age of 27, when I was eight months pregnant with my son. I began experiencing the symptoms from early on in my pregnancy but my GP had repeatedly waved me away with talk of piles, advising me to “just get on with it”. As I grew seriously ill, I spent more and more time at hospital, with the doctors at a loss as to why I was so weak. I didn’t bother to mention the “piles”, thinking that they couldn’t possibly be to blame. It was only when I was well into my third trimester, and an obstetrician asked if there was anything else going on, that I described my symptoms. I was immediately referred to the gastroenterology department and the diagnosis was made. I had never heard of the disease before, and at the time felt only relief that I didn’t have cancer as I’d suspected. If I had only known what was to come, I would have been far more distraught.
So don’t take pity on me. Don’t treat me as if I’m different. But if I ask if I can jump in front of you in the queue for the ladies, please step swiftly aside.
Recommended Reading: What Is Good For Ulcerative Colitis
How Common Is Cramping Among Those Who Have Uc
Inflammatory bowel disease, which includes both UC and Crohns, affects about 1.6 million Americans of all ages, according to the Crohns and Colitis Foundation. More than half of those with UC experience abdominal pain.
The frequency and persistence of cramping can help determine the severity of UC, according to Faten N. Aberra, MD, MSCE, co-director of the Inflammatory Bowel Disease Center at the Joint Penn-CHOP Center and an associate professor of medicine at the Hospital of the University of Pennsylvania, in Philadelphia. Pain that comes and goes with bowel movements may indicate a moderate level of UC. Constant cramping and frequent, bloody stools, on the other hand, may indicate a more serious condition, says Dr. Aberra, such as a dilated colon.
If You Have Moderate To Severe Ulcerative Colitis
In 2020, the American Gastroenterological Association released updated treatment guidelines for adults with moderate to severe UC.
The AGA suggested that people whove never received biologics before should only receive tofacitinib if theyre a part of a clinical study or registry study.
The organization also recommended that people whove never received biologics before choose infliximab or vedolizumab instead of adalimumab .
Adalimumab isnt as effective as the other two biologics. However, people with UC can administer adalimumab to themselves, while healthcare professionals have to administer infliximab and vedolizumab. If youre looking for convenience over efficacy, its fine to choose adalimumab instead.
Don’t Miss: Prevention And Treatment Of Pressure Ulcers
How To Treat Pain
There are various treatment options for UC, and the best approach for a person will depend on the severity of their symptoms. Over-the-counter medications can sometimes help relieve the pain that UC can cause. However, severe cases require stronger pain relievers.
Medications for the treatment of UC include:
What Causes Uc Cramping
Common causes of UC cramping, according to Ha, are flare-ups, lack of sufficient control of the condition , eating foods that are high in saturated fat or sugar, and adverse reactions to medication.
Cramping due to gas and bloating can also be caused by irritable bowel syndrome , a separate condition from ulcerative colitis that can cause symptoms even when your disease is in remission. IBS can be linked to certain gas-causing foods, including dairy if youre lactose intolerant.
Recommended Reading: How To Get Remission In Ulcerative Colitis
What To Look For
The key is to pay attention to your specific symptoms. The more you’re aware of them, the better able you are to spot changes.
And there are lots of ways your symptoms can change. You might get new ones. Or the ones you have may get worse, last longer, or come on more often.
Usually, a flare-up brings at least:
- An urgent need to poop
- Blood or mucus in your stool
- Cramps in your lower belly
If it spreads to more areas of the colon, everything gets more intense. You have more diarrhea. Cramps get more severe. You have more mucus, pus, and blood in your stool. Pain in your belly gets worse and more widespread, especially up the left side. It can also affect your desire to eat and cause you to lose weight.
And some of those symptoms may just be signs of a stronger flare-up. You’ll need to see your doctor to find out for sure. Read more on ulcerative colitis symptoms to look for.