Looking After Yourself During Treatment
The following advice may help your ulcer heal more quickly.
- Try to keep active by walking regularly. Sitting and standing still without elevating your legs can make venous leg ulcers and swelling worse.
- Whenever you’re sitting or lying down, keep your affected leg elevated.
- Regularly exercise your legs by moving your feet up and down, and rotating them at the ankles. This can help encourage better circulation.
- If you’re overweight, try to reduce your weight with a healthy diet and regular exercise.
- Stop smoking and moderate your alcohol consumption. This can help the ulcer heal faster.
- Be careful not to injure your affected leg, and wear comfortable, well-fitting footwear.
You may also find it helpful to attend a local healthy leg club, such as those provided by the Lindsay Leg Club Foundation, for support and advice.
Define The Scope Of The Ebp
VLU is a common chronic condition affecting nearly 2.5 million individuals annually, characterized by an extended healing trajectory and a high risk of recurrence. According to the statistics, only 58 percent of patients heal, and 4 percent undergo amputation . Thus, the condition poses great clinical and economic challenges and requires an effective approach to its treatment.
Nowadays, practitioners may choose various methods for the healing of VLUs. Foam dressing is one of them, but it is not utilized so often compared to other products . Currently, there is not enough evidence on the efficacy of foam dressings in the treatment of the condition. Thus, the EBP research in this area is of great importance as it may contribute to the expansion of the existing knowledge base.
What You Need To Know
-
The cornerstone of treatment for venous leg ulcers is compression therapy, but dressings can aid with symptom control and optimise the local wound environment, promoting healing
-
There is no evidence to support the superiority of one dressing type over another when applied under appropriate multilayer compression bandaging
-
When selecting a dressing, look at the wound bed, edge and surrounding skin and decide on the goal of the dressing: for example, if there are signs of localised infection consider an antimicrobial dressing, if there is heavy exudate consider an absorbent dressing
A 65 year old man presents with a two month history of a wound in the gaiter area of his left leg. He has a history of a left leg deep vein thrombosis after a long flight but is otherwise fit and well. He had been self-managing with dressings bought over the counter, but the wound has gradually increased in size. The wound is not painful but is weeping serous fluid, causing irritation of the surrounding skin. Examination shows a 4×3×0.1cm wound above the left medial malleolus. There is haemosiderin deposition, venous flare, and moderate oedema in the limb. The ankle-brachial pressure index is normal at 1.0. He is diagnosed with a venous leg ulcer, which is managed with dressings and compression bandaging.
About 1% of the adult population in Westernised countries are affected by venous ulcers on the leg or foot.2 The prevalence increases with age to 1.7% in
Don’t Miss: How Does Ulcerative Colitis Affect The Body
Best Cream For Leg Ulcers
Many people suffer from leg ulcers. Leg ulcers are similar to a break in the skin of the leg, which allows air and bacteria to get to the underlying tissues. It can be formed by a minor injury that breaks the skin. It is also caused due to obesity, diabetes, and hypertension.
Contents
Determine Responsibility Of Team Members

Stakeholders are selected from different organizational levels and professional backgrounds because, in this way, it will be easier to integrate changes throughout the hospital. The Director will participate as a co-leader and will provide managerial support. The nurse epidemiologist will be responsible for monitoring and evaluation of the results. The charge nurse will co-manage and ensure the program follow-up.
Recommended Reading: Ulcerative Colitis And Hip Pain
Cleaning And Dressing The Ulcer
The first step is to remove any debris or dead tissue from the ulcer and apply an appropriate dressing. This provides the best conditions for the ulcer to heal.
A simple non-sticky dressing will be used to dress your ulcer. This usually needs to be changed once a week.
Many people find they can manage cleaning and dressing their own ulcer under the supervision of a nurse.
Foam Dressings For Venous Leg Ulcers
Venous leg ulcers are a common and recurring type of chronic wound. Compression therapy is used to treat venous leg ulcers. Dressings that aim to protect the wound and provide a moist environment to aid ulcer healing are applied beneath compression devices. Foam dressings are one of several types of dressing available. We evaluated the evidence from 12 randomised controlled trials that either compared different types of foam dressings, or compared foam dressings with other types of wound dressings. We found no evidence to suggest that polyurethane foam dressings are significantly better or worse than hydrocellular foam dressings in venous leg ulcer healing. Similarly, we found no evidence to suggest that foam dressings are significantly better or worse than other types of dressings , for the healing of venous leg ulcers. We found insufficient evidence to draw any conclusions regarding: adverse events, quality of life, costs, pain, or dressing performance. Overall, the current evidence is of low or unclear methodological quality. This limits the making of any specific recommendations regarding the use of foam dressings. Further, good quality evidence is required before definitive conclusions can be made regarding the role of foam dressings in the management of venous leg ulcers.
You May Like: Best Way To Heal Stomach Ulcers
Data Collection And Analysis
Two review authors independently performed study selection, ‘Risk of bias’ assessment and data extraction. We conducted this NMA using frequentist metaregression methods for the efficacy outcome the probability of complete healing. We assumed that treatment effects were similar within dressings classes . We present estimates of effect with their 95% confidence intervals for individual treatments focusing on comparisons with widely used dressing classes, and we report ranking probabilities for each intervention . We assessed the certainty of the body of evidence using GRADE for each network comparison and for the network as whole.
Treating An Infected Ulcer
An ulcer sometimes produces a large amount of discharge and becomes more painful. There may also be redness around the ulcer.
These symptoms and feeling unwell are signs of infection.
If your ulcer becomes infected, it should be cleaned and dressed as usual.
You should also elevate your leg most of the time. You’ll be prescribed a 7-day course of antibiotics.
The aim of antibiotic treatment is to clear the infection. But antibiotics do not heal ulcers and should only be used in short courses to treat infected ulcers.
Read Also: How To Treat An Ulcer After Gastric Bypass
Process Outcomes Evaluation And Reporting
During the EBP realization, the information about cost-efficiency, time of healing, and the overall patient outcomes should be collected. The evaluation will be carried out based on the objective patient data and nursesâ self-reports regarding the compliance with the specifically designed care protocols. The information will be collected on a daily basis and, by the end of week 11, evaluated by the nurse epidemiologist and the project leader. A comprehensive report on the project outcomes will be submitted to the hospital management and discussed at the collective meeting of the involved stakeholders.
What Is A Foam Dressing
Wound dressings can accelerate the healing process by protecting the injury or wound from bacteria and creating an environment which supports healthy healing. Foam dressings are an effective tool for moist wound healing and are particularly useful in preventing dressing-related trauma, managing exuding wounds, and minimizing dressing discomfort and pain.
Also Check: What To Do When Ulcerative Colitis Flares
How The Intervention Might Work
Animal experiments conducted over 40 years ago suggested that acute wounds heal more quickly when their surfaces are kept moist rather than left to dry and scab . A moist environment is thought to provide optimal conditions for the cells involved in the healing process with faster revascularisation , and development of granulation tissue , as well as allowing autolytic debridement , which is thought to be an important part of the healing pathway .
The desire to maintain a moist wound environment is a key driver for the use of wound dressings and related topical agents. Whilst a moist environment at the wound site has been shown to aid the rate of epithelialisation in superficial wounds, excess moisture at the wound site can cause maceration of the surrounding skin , and it has also been suggested that dressings that permit fluid to accumulate might predispose wounds to infection . Wound treatments vary in their level of absorbency, so that a very wet wound can be treated with an absorbent dressing to draw excess moisture away and avoid skin damage, whilst a drier wound can be treated with a more occlusive dressing or a hydrogel to maintain a moist environment.
Some dressings are now also formulated with an ‘active’ ingredient .
Description Of The Condition
Venous leg ulcers are common and recurring complex wounds that heal by secondary intention . Problems with the leg veins reduce the efficient return of blood to the heart and increase the pressure in the veins , which may result in venous leg ulcers. The precise chain of events that links high venous pressures with skin breakdown and a chronic wound is not fully understood .
Venous leg ulcers commonly occur on the gaiter region of the lower leg . A venous leg ulcer is defined as any break in the skin that has either been present for longer than six weeks or occurs in a person with a history of venous leg ulceration. Differential diagnosis of the type of leg ulcer is made by taking a clinical history, physical examination, laboratory tests and haemodynamic assessment . True venous ulcers are moist, shallow and irregularly shaped and lie wholly or partly within the gaiter area of the leg. Leg ulcers can be associated with venous disease in combination with vascular disease, which impairs arterial blood supply in these instances they are said to have a ‘mixed’ aetiology . Open skin ulceration due solely to limb ischaemia from vascular disease is less common.
You May Like: What Are The Symptoms Of An Ulcer In Your Stomach
Activheal Foam Adhesive Is An Absorbent Foam Dressing Ideal For Moderate To High Exuding Wounds
FEATURESEXCELLENT ABSORPTION OF EXUDATE // VERSATILE // PROMOTES HEALING THROUGH A MOIST WOUND ENVIRONMENT // REDUCES THE RISK OF MACERATION // WATERPROOF // BACTERIAL BARRIER // SOFT AND COMFORTABLE //
ActivHeal® Foam Adhesive is a two layer dressing indicated for moderate to heavily exuding wounds. Each layer of the ActivHeal® Foam Adhesive contributes to the performance of the dressing.
The dressing comprises of a polyurethane absorbent foam pad and a polyurethane membrane. The core of the dressing is a layer of absorbent polyurethane foam which absorbs wound exudate vertically into the dressing. The absorbent pad retains the exudate within the dressing preventing the exudate from re-entering the wound and preventing maceration to the peri wound and surrounding skin. The polyurethane membrane provides an effective barrier function and is waterproof whilst allowing the transpiration of exudate which aids the total fluid handling capacity of the dressing.
Indicated for moderate to heavily exudating wounds. The dressing offers a pressure sensitive acrylic adhesive border ensuring the dressing remains in place allowing the patient to continue everyday activities confidently. The dressing conforms to the contours of the body which reduces the risk of rucking or catching on clothing and bedding.
Construction And Features Of Foam Dressings
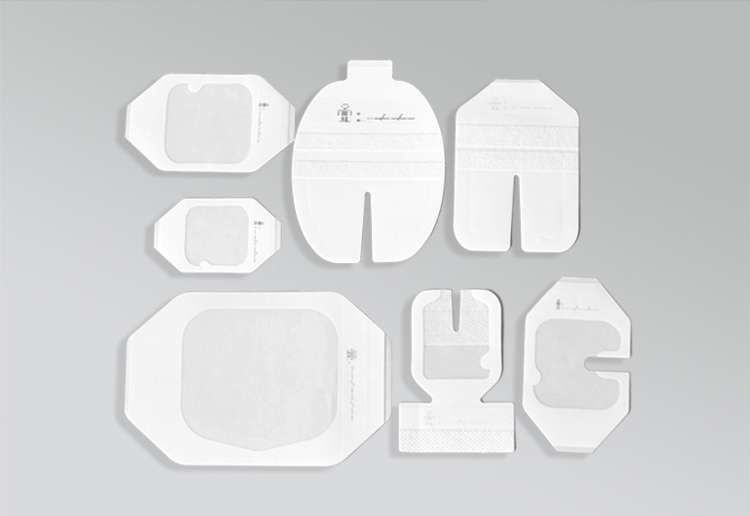
Made of semipermeable polyurethane, foam dressings contain foamed polymer solutions with small, open cells that can hold fluids. These cells may be layered with other materials. Their absorptiveness varies depending on the thickness of the dressing. The contact area of a foam dressing is nonadherent and nonlinting, so the dressing is easy to remove. The outer layer of the dressing is often hydrophobic or waterproof to keep out bacteria and other contaminants. Foam dressings come either with or without an adhesive border and in many sizes and shapes. Some foam dressings also include a bacterial barrier made from a transparent film. Additionally, some foam dressings are impregnated with an antimicrobial agent such as silver, Manuka honey, cadexomer iodine, antibiotics, or include surfactants as a vehicle for delivery of these substances to the wound bed.
A primary feature of foam dressings is that they help maintain a moist wound environment. Also important is that foam helps cushion the wound and periwound area from additional trauma, as well as providing thermal insulation for wounds. Easy to apply and remove, foam dressings don’t cause wound trauma. Foam dressings can be used when there is an infection and during compression therapy. In addition, foam dressings are compatible with enzymatic debridment agents. Depending on the amount of exudate, foam dressings have a wear time of one to seven days.
Read Also: Wound Care For Diabetic Leg Ulcers
Indications And Contraindications For Foam Dressing Use
Foam dressings are excellent for wounds which are exuding, whether minimally or heavily. Generally, foam dressings are meant for partial- or full-thickness wounds. Wounds which benefit from the use of foams dressings include:
- leg ulcers
- pressure ulcers/injuries
- wounds needing negative pressure wound therapy
- tracheotomy and gastrostomy tubes
- wound cavities
Foam dressings can be used on wounds that have softened necrotic tissue. They are also flexible and can be cut to fit specific body parts like toes, fingers, or ears. Because of their thermal properties, foam dressings can be used on a wound which needs insulation to keep it warm. Additionally, foam dressings can be helpful in protecting the skin on top of bony prominences or high friction areas on the skin.
Non-draining wounds and third-degree burns are generally not good candidates for foam dressings. These dressings are also not effective on wounds which have dry eschar because with no exudate, the wound bed may be too dry for a moist wound healing environment . Excessive exudate can be a contraindication if the foam is being soaked through quickly, possibly allowing external bacteria to enter the wound. In addition, excessive exudate can require too many dressing changes and cause maceration of the periwound area. In such cases, a more absorbent foam or another dressing type is indicated.
Proper Foam Dressing Application Instructions
The procedure for applying a foam dressing is as follows:
The flexibility of foam dressings allows for a wide variety of clinical applications with wounds that have from moderate to heavy exudate. Because they are easy to use and can be easily cut to fit irregular wound areas, they are a good dressing choice for many situations.
The views and opinions expressed in this blog are solely those of the author, and do not represent the views of IncontinenceSource, Kestrel Health Information, Inc., its affiliates, or subsidiary companies.
You May Like: Is Oatmeal Good For Ulcerative Colitis
Evaluating The Efficacy Of An Absorbent Foam Dressing Containing Silver Versus The Same Dressing Without Silver Used On Subjects With Venous Leg Ulcers Or Mixed Ulcers
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| First Posted : December 21, 2009Results First Posted : September 12, 2014Last Update Posted : September 12, 2014 |
| Venous Leg UlcersMixed Leg Ulcers | Device: Mepilex AgDevice: Mepilex without Ag | Phase 4 |
| Study Type : | |
| Quadruple | |
| Primary Purpose: | Treatment |
| Official Title: | A Double-blind, Comparative, Superiority, Multi-centre Investigation Evaluating the Efficacy of an Absorbent Foam Dressing Containing Silver Versus the Same Dressing Without Silver Used on Subjects With Venous Leg Ulcers or Mixed Ulcers |
| Study Start Date : |
| Placebo Comparator: Mepilex product | Device: Mepilex without AgMepilex is designed for a wide range of exuding wounds such as leg and foot ulcers, pressure ulcers and traumatic wounds, e.g. skin tears and secondary healing wounds. |
| Active Comparator: Mepilex Ag | Device: Mepilex AgMepilex is designed for a wide range of exuding wounds such as leg and foot ulcers, pressure ulcers and traumatic wounds, e.g. skin tears and secondary healing wounds. |
Curavance Foam Ag Bordered Dressings
CuraVance Foam Ag Dressings are indicated for the management ofmoderate to heavily exuding, acute and chronic wounds including: diabetic foot ulcers, venous leg ulcers, pressure ulcers, graft and donor sites, trauma wounds, second-degree burns, and post-operative wounds and skin abrasions.
The semipermeable polyurethane film outer layer acts as a liquidand microbial barrier to prevent contamination, while delivering balanced oxygen and moisture vapor transfer for a moist wound healing environment.
Non-adherent foam absorbs and retains exudate and ensures atraumatic dressing removal to deliver optimal patient outcomes.
Laboratory testing has demonstrated that CuraVance Foam Ag Dressingsprovide broad-spectrum antibacterial activity against the most commonpathogens associated with wound infections for up to 7 days.
CuraVance Foam Ag Dressings are available withand without adhesive border.
- Absorbent foam absorbs excess wound fluid to maintain the optimal moist wound healing environment.
- Non-adherent foam reduces pain and trauma during dressing changes.
- Broad spectrum antibacterial activity protects against the most common pathogens associated with wound infection.
- High MVTR semi-permeable PU film provides low coefficient of friction and extends wear time
- Transparent film serves as a physical barrier to prevent fluid and microbial contamination
Read Also: Boots To Prevent Pressure Ulcers