Dont Skip Your Medication
If you already have prescription medication for colitis, take your medication as prescribed. Dont skip your medicine, even if you feel better.
If you need help remembering to take your medication, use a reminder on your phone and/or set a sticky note on your keys
Sticking with your medication schedule can help you stay in remission and avoid a flare-up.
Is Ulcerative Colitis Curable
Currently, theres no nonsurgical cure for UC. Treatments for the inflammatory disease aim to extend periods of remission and make flare-ups less severe.
For people with severe UC, curative surgery is a treatment option. Removing the entire large intestine will end the symptoms of UC.
This procedure requires your doctor to create a pouch on the outside of your body where waste can empty. This pouch can become inflamed and cause side effects.
For that reason, some people choose to have only a partial colectomy. In this surgery, your doctor only removes the parts of the colon that are affected by UC.
While these surgeries can help ease or end symptoms of UC, they can have adverse effects and possible long-term complications. Read more about these issues to determine if surgery is an option for you.
Find Ways To Chill Out
All of the stress-busting suggestions above are extra important when youre in the midst of a flare-up. Cohen also recommends implementing deep breathing exercises before every meal, as this relaxes your body and mind allows you to digest more optimally. And, since youll be eating 4-6 smaller meals, this is a great way to get a dose of calm at multiple points in the day.
Recommended Reading: List Of Foods To Avoid With Ulcerative Colitis
Recommended Reading: How Can I Get Rid Of Mouth Ulcers
Immune Thrombocytopenic Purpura As An Uncommon Extraintestinal Complication Of Crohns Disease: Case Vignette And Systematic Literature Review
Raisa Epistola
1Harbor-UCLA Medical Center, Department of Medicine, Torrance, CA, USA
2Harbor-UCLA Medical Center, Department of Medicine, Division of Hematology & Medical Oncology, Torrance, CA, USA
3Harbor-UCLA Medical Center, Department of Medicine, Division of Gastroenterology, Torrance, CA, USA
4University of California Los Angeles Division of Digestive Diseases, Los Angeles, CA, USA
Abstract
While the association of immune thrombocytopenic purpura and inflammatory bowel disease has been described in a few case reports, management of ITP as an extraintestinal manifestation of Crohns disease is less studied. There are approximately a dozen cases describing the management of patients dually diagnosed with CD/ITP. Previous reports postulated that the mechanism of ITP in CD was through the presence of circulating immune complexes in the serum and antigenic mimicry due to increased mucosal permeability in active colitis, versus increased mucosal production of TH1-type proinflammatory cytokines during CD flares, which may account for remission of ITP with surgery for CD. We present a case of a 27-year-old man who presented with medically refractory CD and ITP who responded to surgical management with colectomy and splenectomy, along with a systematic review of the literature. These cases suggest that colectomy should be considered in the treatment of medically refractory ITP among patients with concomitant CD.
1. Introduction
2. Case Description
3. Discussion
| Title |
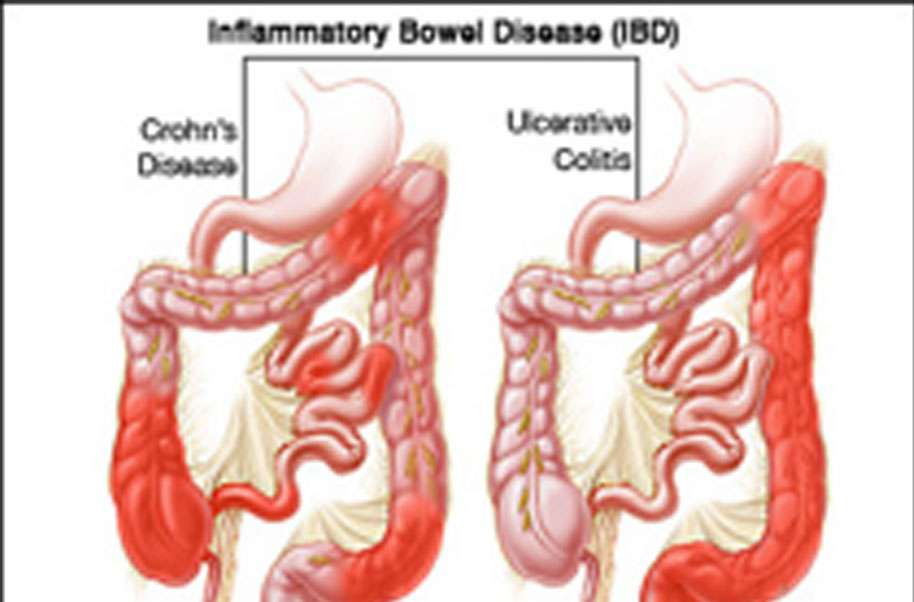
Types Of Ulcerative Colitis
UC can be categorized according to the parts of the GI tract that it affects.
- Ulcerative proctitis. In ulcerative proctitis, only the rectum is inflamed. Its considered a mild form of UC.
- Left-sided colitis. Left-sided colitis causes inflammation in the area between the splenic flexure and the last section of the colon. The last section of the colon, known as the distal colon, includes the descending colon and sigmoid colon. Left-sided colitis is also known as distal ulcerative colitis.
- Proctosigmoiditis. Proctosigmoiditis is a form of left-sided colitis. It causes inflammation in the rectum and sigmoid colon.
Different tests can help a doctor diagnose UC. UC mimics other bowel diseases such as Crohns disease. A doctor will order multiple tests to rule out other conditions.
Tests to diagnose UC often include:
You May Like: Ulcerative Colitis Flare Up Foods
Physical Exercises For The People Suffering From Low Platelets:
Although physical activities are advised to be limited in case of low blood platelets condition in patients, light and gentle exercises are preferred to be done in such cases, keeping the point in mind that risks of injuries should not be happening.
Exercising on a regular basis is beneficial in this condition. Some of the exercises that may be preferred include sitting exercises, light stretching, brisk walking, and stationary biking.
Treatment Of Ulcerative Colitis
If fulminant or toxic colitis is suspected, the patient should
-
Stop all antidiarrheal drugs
-
Take nothing by mouth and have inserted a long intestinal tube attached to intermittent suction
-
Receive aggressive IV fluid and electrolyte therapy with 0.9% sodium chloride, and potassium chloride and blood as needed
-
Receive high-dose IV corticosteroids or cyclosporine
-
Receive antibiotics
-
Perhaps receive infliximab
Having the patient roll over in bed from the supine to prone position every 2 to 3 hours may help redistribute colonic gas and prevent progressive distention. Insertion of a soft rectal tube may also be helpful but must be done with extreme caution to avoid bowel perforation. Even if decompression of a dilated colon is achieved, the patient is not out of danger unless the underlying inflammatory process is controlled otherwise, colectomy will still be necessary.
If intensive medical measures do not produce definite improvement within 24 to 48 hours, immediate surgery is required or the patient may die of sepsis caused by bacterial translocation or even perforation.
Also Check: Can You Drink Alcohol If You Have Ulcerative Colitis
Ulcerative Colitis: Causes And Risk Factors
Causes
Experts dont know what causes ulcerative colitis, but it may be related to your immune system. Normally, your immune system attacks bacteria and viruses that could make you sick. However, with UC, the immune system mistakes the cells of your large intestine for a threat and attacks. When your immune system attacks your own healthy cells, it is referred to as an autoimmune condition. This causes inflammation and ulcers.
Why some people develop ulcerative colitis and not others is still being studied. It may have to do with genetic factors. You are more likely to develop UC if a family member has it. However, most cases develop in people without a family history.
Environmental factors, like exposure to certain viruses or bacteria, may also play a role. Your body may try to fight this infection and then overreact.
Doctors used to think that excess stress and certain foods cause ulcerative colitis, but we now know this isnt true. Diet and stress can make symptoms worse, but they dont cause them.
Risk factors
A risk factor is anything that increases your chance of developing a certain disease. Some risk factors for ulcerative colitis include:
Effect Of Iron Therapy On Platelet Counts In Patients With Inflammatory Bowel Disease
-
Affiliation Department of Medicine 3, Medical University of Vienna, Vienna, Austria
-
Affiliations Department of Medicine 3, Medical University of Vienna, Vienna, Austria, Christian Doppler Laboratory for Molecular Carcinoma Chemoprevention, Medical University of Vienna, Vienna, Austria
-
Affiliation Department of Medicine 3, Medical University of Vienna, Vienna, Austria
-
* E-mail:
Affiliations Department of Medicine 3, Medical University of Vienna, Vienna, Austria, Christian Doppler Laboratory for Molecular Carcinoma Chemoprevention, Medical University of Vienna, Vienna, Austria
Read Also: What Are The Best Foods To Eat With An Ulcer
What Is The Treatment For A Low Platelet Count
The first step for the treatment of low platelets in blood involves diagnosis of the cause of the problem. Once the cause of the problem is confirmed, the treatment is done by the concerned doctor accordingly.
In case, the symptoms of low platelet count are not severe enough, the doctor do not go for any treatment and the condition is left to heal by itself. However, treatment for this problem becomes mandatory if the symptoms are severe.
The patients with low platelet count are often recommended to avoid contact sports and other works that have high risks of bleeding, less consumption of alcohol, to stop or change the medicines that affect the count of platelets adversely.
In very serious conditions of low platelet count the doctor recommends for medical treatments like blood or platelet transfusion, administration of immune-globulin, steroids and corticosteroids in order to block platelet antibodies, surgical removal of spleen , change of medications that leads to low platelet count, suppression of immune system of the patient by various medication. Once the root cause for low count of platelets is treated, the count of thrombocytes comes back to normal after a certain span of time.
Definition Of Mucosal Healing
We evaluated mucosal status by total colonoscopy. The Mayo endoscopic subscore contains the following four categories : 0, normal or inactive disease mild disease with erythema, decreased vascular patterns, and mild friability moderate disease with marked erythema, absence of vascular patterns, friability, and erosions severe disease with spontaneous bleeding and ulceration. Partial MH and MH were defined as category 0 and 01 in this study, respectively. Several endoscope specialists were responsible for evaluating MES and MH, and all endoscopists were blinded to platelet count.
You May Like: What’s The Difference Between Ulcerative Colitis And Crohn’s Disease
What Should I Eat During A Flare
Youre feeling good, taking your medication, eating generally anti-inflammatory foods, and all of suddenbamyou start to feel those telltale flare symptoms. What should you do now? Adjusting your diet may help you over the hump.
If you are in a flare, you may want to eat foods that are gentle on your digestive tract, while the inflammation calms down, says Dr. Singh.
Practically speaking, you can do this in a few ways. For instance, Freuman works with her clients to tailor a well-rounded diet to avoid their specific triggers and address their needs. This may include:
Its best to work with a professional when making changes to your diet, as they can ensure that you are getting the nutrients that you need, help you assess your trigger foods, and address any underlying history of disordered eating or dietary changes that could trigger those behaviors.
Also Check: How To Treat Sacral Pressure Ulcer
What Is An Ulcerative Colitis Diet
A person with ulcerative colitis may find they need to modify their diet to help manage their symptoms. There is not a single diet or meal plan that fits everyone with ulcerative colitis, and diets are individualized for each patient. Depending on symptoms different types of diets may be recommended, such as:
- A high-calorie diet: Many people with ulcerative colitis lose weight and can develop signs of malnutrition. A high calorie diet may prevent these problems.
- A lactose-free diet: People with ulcerative colitis may also have lactose intolerance.
- A low-fat diet: Ulcerative colitis may interfere with fat absorption and eating fatty foods may trigger symptoms. This is often recommended during an ulcerative colitis flare.
- A low-fiber diet : This can help reduce the frequency of bowel movements and abdominal cramps.
- A low-salt diet: This diet is used when patients are on corticosteroid therapy to help reduce water retention.
- A low FODMAP diet: FODMAPstands for Fermentable Oligo-Di-Monosaccha-rides and Polyols, which are types of sugars found in certain carbohydrates and sugar alcohols. This diet is used in people who have intolerance to FODMAPS.
- A gluten-free diet: People with ulcerative colitis may also be sensitive to gluten.
Recommended Reading: Aloe Vera Gel For Horses Ulcers
How Is Ulcerative Colitis Diagnosed
If you have symptoms of ulcerative colitis, you should reach out to your healthcare professional. They will start by asking you about your symptoms, your family and medical history, and your lifestyle. They will also perform a physical exam.
Your doctor may also order one or more of the following tests to rule out other diseases and confirm your diagnosis.
Lab tests
- Blood tests. A small blood sample can be checked in a lab for signs of infection or anemia.
- Stool sample tests. A stool sample can be checked in a lab for the presence of white blood cells or certain proteins, which can both be signs of ulcerative colitis. The sample can also be checked for other problems, like bacteria, viruses, or parasites.
Endoscopic procedures
The only way to know for sure if you have UC is to do an endoscopic procedure. This involves using a special tool, called an endoscope, to see inside your large intestine or other parts of your digestive tract. There are several possible types of this procedure.
Medical imaging
If you have severe inflammation or severe symptoms, your doctor may recommend doing a medical imaging test instead of an endoscopic procedure. These tests are non-invasive but still allow your doctor to look for serious complications. They include:
You Could Develop Chronic Fatigue
When you have active inflammation, your body is running a marathon, Bonthala says. You waste a lot of energy. Research backs this up: A study published in the March 2020 issue of the Journal of Crohns and Colitis found that people who were in remission reported less fatigue than people with active ulcerative colitis or Crohns disease, another type of IBD.
Also Check: What Can I Do For Ulcer Pain
What Can I Do For Periods Of Poor Appetite And Weight Loss To Prevent Malnutrition
At times, there are very few foods that are tolerated well. During these times it is important to eat high calorie foods in tolerable amounts as frequently as possible. During times when solid foods cause irritation or you have a poor appetite, liquid oral supplementation may help provide nutrition. The following list includes liquid supplements for Crohns Disease and ulcerative colitis.
Liquid Supplements for Crohns Disease
Liquid Supplements for Ulcerative Colitis
Because people with ulcerative colitis do not have malabsorption concerns, a supplement that contains partially broken down protein is not usually needed. Standard supplements are fine but are more easily tolerated if they are isotonic or low concentration, which helps prevent diarrhea. Some formulas that may be helpful include Modulen IBD or Enlive .
Ulcerative Colitis And Colonoscopy
Doctors can use a colonoscopy to diagnose UC or determine the severity of the condition.
Before the procedure, a doctor will likely instruct you to reduce solid foods and switch to a liquid-only diet. Then youll fast for a period of time before the procedure.
Typical colonoscopy prep involves taking a laxative the evening before the procedure, too. This helps eliminate any waste still in the colon and rectum. Doctors can examine a clean colon more easily.
During the procedure, youll lie on your side. Your doctor will give you a sedative to help you relax and prevent any discomfort.
Once the medication takes effect, the doctor will insert a colonoscope into your anus. This device is long and flexible so it can move easily through your GI tract. The colonoscope also has a camera attached so your doctor can see inside the colon.
During the exam, the doctor will look for signs of inflammation and check for precancerous growth called polyps. The doctor may also perform a biopsy. The tissue can be sent to a laboratory for further examination.
If youve been diagnosed with UC, a doctor may conduct periodic colonoscopies to monitor inflammation, damage to your intestines, and healing progress.
These symptoms are sometimes associated with UC complications.
If you havent been diagnosed with UC, see a doctor if you experience multiple symptoms of the condition. They can help determine whether you may have UC or another bowel disease.
Recommended Reading: How To Know If You Have A Peptic Ulcer
Who Is Not Eligible For The Treatment
The condition of thrombocytopenia or low blood platelets may not need urgent care or medical attention in some cases which are associated with mild symptoms such as when the level of platelets is not that much low in the blood.
The presence of some of the warning signs and symptoms like bruising of the skin, bleeding, skin rashes, etc. are not evident and the patient need not be admitted to the hospital.
Assessment Of Disease Progression
Body weight, fecal status, presence of occult blood in the stools, and perianal bleeding were observed and recorded daily while the mice received DSS. A disease activity index , ranging from 0 to 4, was used for clinical assessment of disease severity and calculated from data collected on stool consistency, fecal blood, weight loss, and macroscopic evaluation of the anus, as previously described17, 19. Daily measurements of DAI confirmed that DSS treatment resulted in clinical responses that are consistent with colitic disease activity. Disease progression in the T-cell transfer model was monitored using changes in body weight, colon weight-to-length ratio and a gross inflammation score that reflected colon wall thickening and rigidity, hyperemia, and evidence of colonic adhesions21.
A blood sample was obtained from T-cell transfer mice between 5 8 weeks after the adoptive transfer of T-cells, when there was clear evidence of disease activity . Colon length and weight were measured and scored for macroscopic evidence of inflammation as follows: 0, normal colonic morphology 1, mild bowel wall thickening in the absence of visible hyperemia 2, moderate bowel wall thickening and hyperemia 3, severe bowel wall thickening with rigidity and marked hyperemia and 4, severe bowel wall thickening with rigidity, hyperemia, and colonic adhesion21.
Recommended Reading: How Do I Find Out If I Have An Ulcer