Ulcerative Colitis In Children
According to one study of IBD in the United States, 1 in 1,299 children between ages 2 and 17 years old were affected by the condition in 2016. Crohns disease was twice as common as UC, and boys were more likely to have IBD than girls.
For children with IBD, a diagnosis is more likely after 10 years old.
UC symptoms in children are similar to symptoms in older individuals. Children may experience bloody diarrhea, abdominal pain and cramping, and fatigue.
In addition, they may experience issues compounded by the condition, such as:
- anemia due to blood loss
- malnutrition from poor eating
- unexplained weight loss
UC can have a significant effect on a childs life, especially if the condition isnt treated and managed properly. Treatments for children are more limited because of possible complications. For example, medicated enemas are rarely used as a treatment method in children.
However, children with UC may be prescribed medications that reduce inflammation and prevent immune system attacks on the colon. For some children, surgery may be necessary to manage symptoms.
If your child has been diagnosed with UC, its important that you work closely with their doctor to find treatments and lifestyle changes that can help. Check out these tips for parents and children dealing with UC.
Drugs That Target Inflammation
Most people with UC take prescription drugs called aminosalicylates that tame inflammation in the gut. These include balsalazide , mesalamine , olsalazine , and sulfasalazine . Which one you take, and whether it is taken by mouth or as an enema or suppository, depend on the area of your colon that’s affected. As long as you avoid your triggers, these may be enough if your disease is mild to moderate.
You may need something else if your condition is more severe or if those standard treatments stop working. Your doctor may consider other medicines. Some people may also need surgery.
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
Read Also: What Causes Mouth Ulcers On Gums
Complications Of Ulcerative Colitis
UC increases your risk of developing colon cancer. The longer you have the disease, the higher your risk of this cancer.
Because of this increased risk, your doctor will perform a colonoscopy and check for cancer when you receive your diagnosis.
Repeat screenings are recommended thereafter, according to the American Cancer Society. Regular screenings help lower your risk of colon cancer. Follow-up screenings can detect precancerous cells early.
Other complications of UC include:
- thickening of the intestinal wall
- intestinal bleeding
Who Diagnoses Ulcerative Colitis
If you have symptoms of ulcerative colitis, your regular healthcare provider will probably refer you to a specialist. A gastroenterologist a doctor who specializes in the digestive system should oversee the care for adults. For young patients, a pediatric gastroenterologist who specializes in children should manage the care.
You May Like: How Can You Tell If You Have An Ulcer
Avoid Foods That Make Symptoms Worse
Diet does not cause ulcerative colitis flare-ups. You may, however, notice that some foods make your symptoms worse. If so, stop eating or drinking those foods. The most common foods that seem to exacerbate ulcerative colitis symptoms are dairy products, fatty foods, and spicy foods. High fiber foods also can worsen symptoms during a flare.
Avoid Foods That May Exacerbate Uc Symptoms
Because a healthy diet is a cornerstone for overall health, its no surprise that it tops Sniders list of natural remedies for ulcerative colitis. Diet is a foundational treatment for patients with ulcerative colitis, he says, adding that there’s often a dietary component to the disease.
According to a review published in October 2014 in Clinical Gastroenterology and Hepatology, people who reported a diet high in fats were more likely to have a relapse of UC. Other studies highlighted in the paper suggested avoiding greasy foods, dairy products, caffeine, and raw fruits and vegetables if you have ulcerative colitis. But the review notes that theres no one-size-fits-all diet for UC, so youll have to figure out what works best for you through trial and error.
It helps to keep a food diary to discover which foods are best for you. Snider says it can’t hurt to limit certain foods, and then if your symptoms improve according to your symptom diary, to continue doing so. He also notes that it’s worthwhile to avoid sugar because its effect on the pancreas hinders the output of anti-inflammatory enzymes.
Also Check: How To Treat A Diabetic Ulcer
Adherence To Topical Therapy
Ulcerative proctitis is an idiopathic and chronic disease. Continuous good adherence is important for controlling chronic diseases however, keeping good adherence of medication is difficult. Adherence to topical therapy in ulcerative colitis is low. In terms of 5-ASA formula consumption, mesalazine suppositories and oral 5-ASAs were used most often, followed by combination therapy , mesalazine enema , and rectal steroids in patients with new-onset ulcerative proctitis . However, in a Swiss IBD cohort study on 800 patients, only 26% patients with ulcerative proctitis were treated with topical therapy of 5-ASA or corticosteroids . From these evidences, low adherence to rectal therapy is considered a reason for low consumption of rectal formula. Recently, a prospective cohort study estimated the adherence of 70 patients treated with rectal mesalazine . In this report, adherence was assessed by tracking pharmacy refills and patients interview. Moreover, 55% patients self-reported occasional nonadherence at enrollment. Surprisingly, 71% of all the subjects were nonadherent to their prescribed regimen based on the medication possession ratio criteria. The reasons for nonadherence were transanal mode of administration and busy lifestyle.
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
You May Like: How To Prevent Pressure Ulcers In Wheelchairs
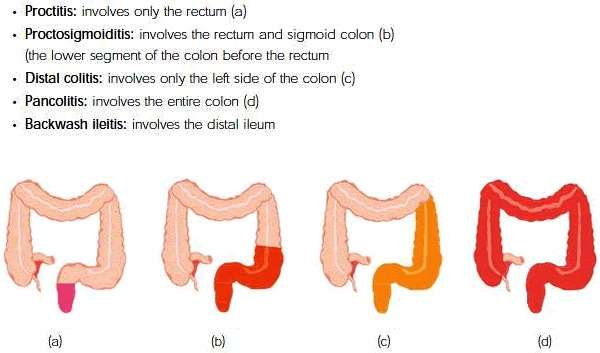
Does Ulcerative Proctitis Always Progress To Ulcerative Colitis
Getting treated for ulcerative proctitis can ease symptoms and even lead to remission, meaning you may not experience symptoms for a certain period of time, but thats not quite the same thing as a cure.
Progression of the disease can happen, but its not super common, although being younger at the time of your diagnosis tends to be a risk factor for more severe disease throughout life, adds Dr. Lerrigo.
Less than 15% of people with ulcerative proctitis go on to develop full-blown ulcerative colitis, according to the National Organization for Rare Disorders . A majority of the time, people with ulcerative proctitis just have ulcerative proctitis. It doesnt necessarily progress to other areas of the colon, Dr. Yoon says. In most people with IBD, wherever the disease is located, it usually stays in that area.
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Liver disease.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Don’t Miss: How To Eat With A Stomach Ulcer
How Do You Get Rid Of Proctitis
Treatment for proctitis depends on the underlying cause of the inflammation.Your doctor may recommend treatments such as:
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Also Check: Can Stomach Ulcer Cause Fever
Birthwort And Horsetail The Remedy For Ulcerative Proctitis
Birthwort and horsetail are two most amazing natural remedies for ulcerative proctitis. Birthwort is cicatrizing and horsetail is antihemorrhagic. Here is how you can use them as home.
Preparation
How to Use
Next Day
NOTE: In the first week of treatment its best to use only 1 tsp. of each of the plants.
How Can My Diet Help Reduce Symptoms Of Proctitis
Depending on the cause of your proctitis, changing your diet can help reduce symptoms.
Your doctor may recommend that you eat more foods that are high in fiber. Eating foods that are high in fiber can make stools softer and easier to pass and can help prevent constipation. A doctor or dietitian can help you learn how to add more high-fiber foods to your diet.
If your proctitis is caused by ulcerative colitis or Crohns disease, a high-fiber diet may make symptoms worse. If you have ulcerative colitis or Crohns disease, talk with your doctor about what foods are right for you.
If you have diarrhea, you may need to avoid certain foods that can make diarrhea worse:
- caffeine
- fructose, a sugar found in fruits, fruit juices, and honey and added to many foods and soft drinks as a sweetener called high-fructose corn syrup
- lactose, a sugar found in milk and milk products
- sugar alcohols, sweeteners used in food products that are labeled sugar-free
Talk with your doctor before changing your diet.
Your doctor may recommend nutritional supplements or vitamins that can help reduce some proctitis symptoms:
Read Also: Do Stomach Ulcers Cause Nausea
Uv Light Therapy In The Treatment Of Ulcerative Colitis
There has been an absence of innovations in treatment for mild ulcerative colitis in recent years. Current therapies have drawbacks that include daily dosing, side effects, and lack of efficacy for some patients. This presents an opportunity in the development of new approaches for treating mild ulcerative colitis.
One of these opportunities, and the subject of research by Dr. Melmed and others, is the use of ultraviolet light. “If you see a mucosal disease, and it is within reach of UV waves that might be brought directly to the colon, characterized by inflammatory pathwaysit may be modulated by light,” Dr. Melmed said.
UV light is outside of the spectrum of light that can be seen with the naked eye. It is already known that UV light is broadly anti-microbial. Photo therapy, which utilizes UV light, is used widely to treat inflammatory skin conditions, including psoriasis, eczema, atopic dermatitis, and vitiligo. In fact, it is a first- or second-line therapy for several skin conditions and has been shown to be safe during pregnancy. It is also known that some inflammatory skin conditions, like psoriasis, may have overlapping inflammatory pathways with IBD.
This led to a question: why only use this light on the surface of the skin? If the inflammatory pathways are similar between IBD and skin conditions, doesn’t it stand to reason that UV light would also work internally?
You can read the first and third posts in this series from IBD Innovate here:
Consider Therapy To Help Manage Stress And Pain
Working with a therapist on certain mind-body techniques can help you control ulcerative colitis symptoms.
Cognitive behavioral therapy and a technique called biofeedback may be useful, as these processes teach skills to cope with stress and pain. In CBT, you learn to recognize and change behaviors and emotions that affect you physically. According to an article in Therapeutic Advances in Gastroenterology, CBT can ease abdominal pain for some people. Biofeedback will teach you how to identify and control some bodily processes, such as heart rate or tension in your muscles, and it can be effective in helping manage chronic pain.
Recommended Reading: Best Feed For Ulcer Prone Horses
Whats The Difference Between Ulcerative Colitis And Crohns Disease
UC and Crohns disease are the most common forms of IBD. Both conditions are thought to be the result of an overactive immune system.
They also share many symptoms, including:
- cramps
- diarrhea
- fatigue
However, UC and Crohns disease do have distinct differences. Understanding the key differences between them can help you obtain a proper diagnosis.
Location
These two conditions affect different portions of the GI tract.
Crohns disease may affect any part of the GI tract, from the mouth to the anus. Its most often found in the small intestine. UC only affects the large intestine and rectum.
Response to treatment
Similar medications are prescribed to treat both conditions. Surgery is also a treatment option. Its a last resort for both conditions, but it can be a cure for UC, whereas its only a temporary therapy for Crohns.
What Are The Potential Complications Of Ulcerative Proctitis
Frequent bleeding due to ulcerative proctitis can lead to anemia, a condition where you dont have enough red blood cells to carry oxygen to the various tissues in your body, or iron deficiency, says Dr. Yoon. According to the National Institutes of Health , if your proctitis isnt treated or doesnt respond to treatment, complications can also include:
- Rectal stricture, which is an abnormal narrowing of the rectum
- Ulcers, or sores in the lining of the intestines
- Colon cancer
Progression to ulcerative colitis can also lead to other complications. With any severe inflammation, theres a risk for perforation of the colon wall, which weakens the whole colon, says Dr. Lerrigo. This means long-term inflammation of the colon has compromised the intestine wall so much that a hole forms, which can be very dangerous, as bacteria can infiltrate places it shouldnt be and cause an infection3.
Chronic inflammation in any organ for a long period of time causes damage at the cellular level, increasing the risk of colon cancer, Dr. Lerrigo adds. Thats why he recommends colonoscopies every year to two years for people who have progressed to ulcerative colitis and have had severe symptoms for many years.
Recommended Reading: Compression Therapy For Venous Leg Ulcers
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
What Is Ulcerative Proctitis

Ulcerative Proctitis is a mucosal inflammatory disease where a part of the bowel, in this case the rectum, is affected. What does that mean? It means youve got inflammation going on in your body that is presenting in the rectum area only in the case of a proctitis sufferer. These diseases with inflammation of the internal organs fall into the spectrum of the autoimmune response type disease.
The thing all these Inflammatory Bowel Diseases have in common is becoming inflamed due to some cause . The body works to neutralize the inflammation, but can sometimes overdo it by attacking and continuing to attack the affected area. This is an autoimmune response and can happen to the point of massive complications with a patients health.
Heres an article from PubMed that explains everything in graphic medical terms
What has happened when you have this Ulcerative condition is the body has turned on you. In this case of having Ulcerative Proctitis, you have a literal pain in the ass that isnt going to just go away. And this is not to be confused with regular Proctitis where the outcomes and interventions can be different.
Read Also: Foam Dressings For Pressure Ulcer Prevention
Heres The Deal About Fixing Ulcerative Proctitis And Other Chronic Illnesses
You need to go the natural route! See a Naturopathic Physician
The body is made to stay at a stasis point. Meaning we heal ourselves. This sounds hoakey? Shush and listen up. Ive done it.
Its real. Even though wikipedia basically implies it a bunch of quackery. Heres the issue, Im living proof of it herbs work
Human Homeostasis is the technical term for this type of balancing act that the human body does. I mean seriously we are some resilient people.
If aliens attacked I have no doubt they would have a serious run for their money. We agile, strong, regenerate quickly, critically analyze, learn, adapt and overcome. We are the apex predators in our ecosystem.
So with all of this ingenuity what are we doing about our Flaming Guts?
Because that is what is causing this problem. You gut is inflamed. Well your body for that matter.
And therefore you must first find out what is the cause of the inflammation.
***Hint: it is not that you are low on mesalamine or steroids in your body
Your blood is most likely boiling with something fierce. You need specific blood analysis to know what is going at a very granular level with you currently.
And once youve tested this, you must retest it every 3 months to see your progress.
No, this isnt cheap and no it is also not fair.
What it is, is what it is. Face it and move through it. Thats what this site is here for
Now get yourself to a naturopath and ask them what their plans are for curing your Ulcerative Proctitis.