What Are The Signs And Symptoms Of Colon Cancer Vs Ulcerative Colitis
Colon Cancer Symptoms and Signs
Some individuals with colon cancer have no symptoms, and if they do have symptoms they often are minimalized and overlooked until the cancer becomes more severe. Cancer screening tests for colon cancer thus are important in individuals 50 years of age and older. Colon and rectum cancer can have many different symptoms and signs. If you have any of these symptoms, seek immediate medical help. You may notice bleeding from your rectum or blood mixed with your stool. It usually, but not always, can be detected through a fecal occult blood test, in which samples of stool are submitted to a lab for detection of blood.
People commonly attribute all rectal bleeding to hemorrhoids, thus preventing early diagnosis owing to lack of concern over “bleeding hemorrhoids.” New onset of bright red blood in the stool always deserves an evaluation. Blood in the stool may be less evident, and is sometimes invisible, or causes a black or tarry stool.
Rectal bleeding due to colon cancer may not be noticeable or chronic, and may only show up as an iron deficiency anemia, not colon cancer. Colon cancer may be associated with fatigue and pale skin due to the anemia. Changes in bowel movement frequency also is a symptom of colon cancer.
If the tumor in the colon becomes large enough, it may completely or partially block your colon. Symptoms of bowel obstruction include:
Ulcerative Colitis Symptoms and Signs
Common symptoms of ulcerative colitis include:
Whats The Difference Between Colonoscopies & Sigmoidoscopies
Colonoscopy and sigmoidoscopy are similar in a number of ways: both are tests that allow doctors to see inside the large intestine. Doctors use colonoscopies and sigmoidoscopies to diagnose a number of health problems. There are differences between the two procedures, though, and these differences can be important.
Begin The Road To Symptom Relief
It is hard to live with chronic symptom flare-ups, and it can be overwhelming when you are in the process of figuring out exactly what illness you might have. Ulcerative colitis and Crohns disease symptoms also overlap with symptoms of IBS and other gastrointestinal conditions, making diagnosis difficult.
Take the information you learned from this article and track your symptoms, so you have information to share with your doctor to help with diagnosis. Then, get a treatment plan in place and start on your journey towards healing.
For more personalized help with healing your gut and IBD treatment options that are tailored to your specific situation, request an appointment at my functional medicine center.
Recommended Reading: Herbal Medicine For Stomach Ulcer
Are Hemorrhoids Considered Inflammatory Bowel Disease
Hemorrhoids are not considered IBD. Although both diseases affect the digestive tract, they are entirely different conditions.
Here are three important differences between the two:
- Hemorrhoids are seen as swollen veins around the anal canal. On the other hand, IBD does not affect the veins of the anus at all. Instead, it affects the walls of the digestive tract and doesnt present as swelling in the anal area. Sometimes, Crohns disease can present as a peri-anal fistula, which is a small opening around the anal area. A tunnel forms which begins inside the anus and ends as a small opening outside of the anus. But this will be different from the swelling seen in hemorrhoids.
- Hemorrhoids have symptoms limited to the anus such as bleeding and pain while passing stool. On the other hand, IBD affects other parts of the digestive tract and has additional symptoms such as fever, weight loss, and mouth ulcers.
- Hemorrhoids are treated by surgical removal. However, treatment for IBD requires a careful combination of drugs and usually lasts years.
The Difference Between Sigmoidoscopy And Colonoscopy
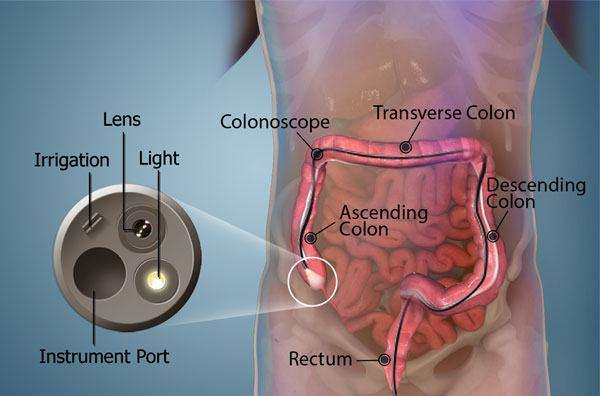
Both sigmoidoscopy and colonoscopy use a camera attached to a thin flexible tube to help doctors view the inside of the large intestine. There are some major differences between the two, though. The primary differences are the areas of the intestines examined and the conditions each can detect.
Colonoscopy is a thorough examination of the large intestine in its entirety, from the cecum to the sigmoid colon.
Doctors use colonoscopies to diagnose a number of digestive conditions, including:
In a sigmoidoscopy, doctors examine only the rectum and the sigmoid. A sigmoidoscopy helps doctors diagnose ulcerative colitis and polyps that might become colon cancer.
A sigmoidoscopy is less invasive than a colonoscopy, so doctors often start with a sigmoidoscopy if they suspect a condition affecting only the sigmoid and not the rest of the colon. Doctors typically recommend that patients undergo colonoscopy if they find polyps on sigmoidoscopy, as if polyps develop in the sigmoid colon, they are likely to develop elsewhere.
For more information on colonoscopies and sigmoidoscopies, or to learn more about each of these important procedures, contact the GI professionals at Allied Digestive. Our gastroenterologists are glad to help.
Also Check: Ulcerative Colitis And Lung Disease
Symptoms Of Ulcerative Colitis And Crohns Disease
The symptoms of Crohns and colitis are often similar and include both digestive and non-digestive symptoms.
Symptoms of both ulcerative colitis and Crohns may include [2, 3
- Arthritis or joint pain
- Hemorrhoids
Symptoms, especially the digestive symptoms, tend to flare-up and recede throughout the course of both diseases. Many people also struggle with brain fog and fatigue, which can flare, but often these two symptoms linger even in between digestive flares.
What Procedures And Tests Diagnose Crohn’s Disease And Ulcerative Colitis
Doctors diagnose ulcerative colitis by endoscopy . During this procedure the doctor can see and take pictures of the patients abnormal gut mucosa , and the presence of continuous disease . Other blood tests and imaging tests like CT scan or MRI are used, but these tests are not definitive.
Doctors use the same procedures and tests to diagnose Crohns disease. However, they also use small bowel studies, colonoscopy, and upper GI endoscopy to identify the abnormal gut mucosa that usually occur in multiple areas anywhere in the intestinal tract. These areas are not continuous, but are separated by normal areas of intestinal mucosa that distinguish them from ulcerative colitis lesions.
As with Crohns disease, nutrition is important if you have ulcerative colitis because symptoms of diarrhea and bleeding can lead to dehydration, electrolyte imbalance, and loss of nutrients. It may be necessary to take nutritional supplements if your symptoms do not allow you to eat a nutritionally balanced diet. Talk to your health-care professional about what supplements to take.
You May Like: Hydrocolloid Dressing For Stage 1 Pressure Ulcer
How To Treat Ulcerative Colitis And Crohns Disease
For both Crohns and colitis, the first-line of conventional treatment with a gastroenterologist tends to focus on:
- Using immunosuppressants such as Remicade and Humeria for both conditions
While many treatment options focus on reducing inflammation for symptom relief, it is also important to determine the root cause of the chronic inflammation. Discovering and treating the root cause can lead to fewer symptoms and minimal flare-ups. The root cause of inflammation is varied and may include toxins in the environment, any possible intestinal microbes, and foods that cause inflammation in your gastrointestinal tract.
Here are some of the main treatment foundations for IBD:
- Eating an anti-inflammatory diet
- Supporting the gut with probiotics
- Lifestyle changes to reduce stress
Burning Pain In Your Abdomen
This may seem like a no-brainer but the most common sign that people experience when they have a stomach ulcer is a persistent burning pain in their abdomen. This sensation occurs when juices in the stomach used for digestion come into contact with the open sore. For the most part, the pain is felt from the breastbone to navel and is often worse at night than during the day. On the other hand, if you are someone who frequently skips meals, you may find that you experience this pain much throughout the daytime.
Recommended Reading: Diabetic Foot Ulcer Treatment Guidelines
Recommended Reading: Are Eggs Bad For Ulcerative Colitis
Getting To A Diagnosis
Theres no doubt that IBD can significantly decrease quality of life, between uncomfortable symptoms and frequent bathroom visits. IBD can even lead to scar tissue and increase the risk of colon cancer.
If you experience any unusual symptoms, its important to call your doctor. You may be referred to a gastroenterologist for IBD testing, such as a colonoscopy, sigmoidoscopy, or a CT scan. Your doctor may also order blood and fecal testing. Diagnosing the specific form of IBD will lead to more effective therapies.
Commitment to daily treatment and lifestyle changes can help minimize symptoms, achieve remission, and avoid complications.
Regardless of your diagnosis, Healthlines free app, IBD Healthline, can connect you with people who understand. Meet others living with Crohns and ulcerative colitis through one-on-one messaging and live group discussions. Plus, youll have expert-approved information on managing IBD at your fingertips. Download the app for iPhone or Android.
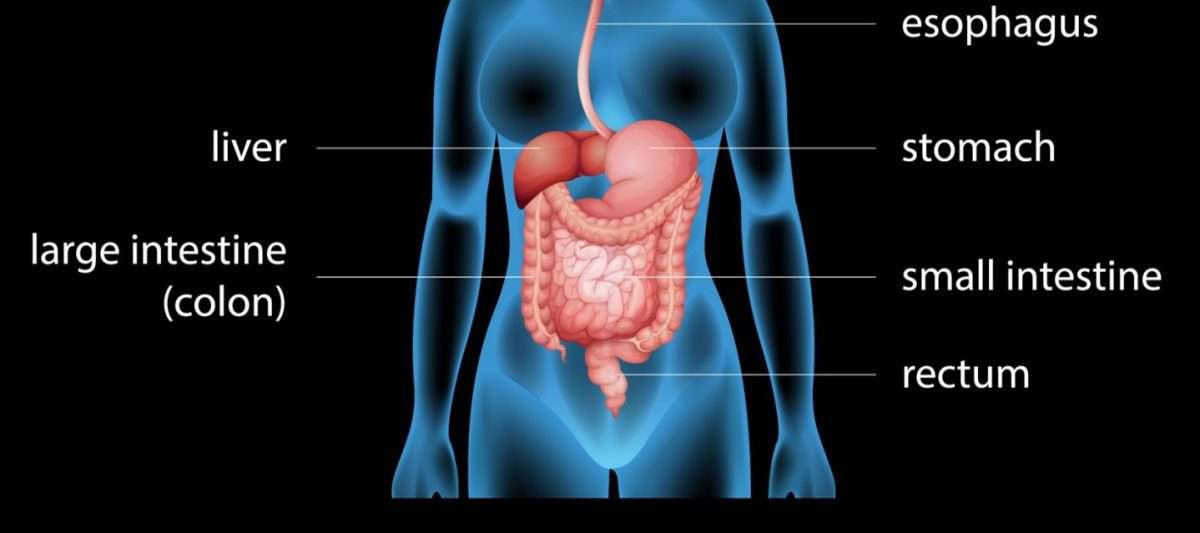
What Is Ulcerative Colitis
Ulcerative colitis is a medical condition that causes ulcers in the large colon and rectum. It is an autoimmune disease. This condition affects the innermost lining of the large intestine and rectum. Ulcerative colitis is debilitating and can lead to life-threatening complications. Doctors classify ulcerative colitis according to inflammation location. There are four types: ulcerative proctitis , proctosigmoiditis , left-sided colitis , pancolitis .
Figure 01: Ulcerative Colitis
The symptoms of this medical condition include diarrhea, abdominal pain, rectal pain, rectal bleeding, urge to defecate, inability to defecate, weight loss, fatigue, fever, and in children, failure to grow. The risk factors include age , ethnicity , and family history . Moreover, this inflammatory condition can be diagnosed through endoscopy, tissue biopsy, blood test, imaging tests , and stool tests. The treatments include anti-inflammatory drugs , immunosuppressant , biologics targeting immune system proteins , and surgery .
You May Like: Can Foot Ulcers Be Cured
Symptoms Of Ulcerative Proctitis
The presenting symptoms of ulcerative proctitis all relate to the rectum. Blood in the stool occurs in almost everyone with the disease. Diarrhea is a common symptom, although constipation can also develop as the body struggles to maintain normal bowel function.
Inflammation of the rectum may cause a sense of urgency to have a bowel movement, discomfort after having a bowel movement, and a sensation of incomplete emptying of the bowels. Systemic symptoms such as fever, tiredness, nausea, and weight loss are rare.
Ulcerative proctitis has very few complications but with increased irritation to the anal and rectal area, hemorrhoids may occur. Only rarely do other complications occur, such as abscesses and extra-intestinal manifestations. Individuals with ulcerative proctitis are not at any greater risk for developing colorectal cancer than those without the disease.
Rectal Bleeding And Inflammatory Bowel Disease

One of the many symptoms of inflammatory bowel disease is bleeding. Blood might appear in or on the stool or some people may pass no stool at all at times, and just pass blood.
Bleeding from the rectum and large intestine from IBD is typically red or bright red, while blood coming from higher up in the digestive tract could appear as darker or black stools. In most cases this bleeding is slow and steady.
However, you should get emergency attention if:
- Bleeding is severe
- Youre vomiting blood
- You faint or feel like youre going to
Blood in or on the stool can be frightening but it doesnt always mean that theres an emergency. Its sometimes part of an IBD flare-up and it should be discussed with a physician as soon as possible, especially if it hasnt happened in a while.
Bleeding means that there is some inflammation somewhere, and a change in treatment might be needed. Many treatments are available for IBD that can help stop the inflammation and the bleeding.
Read Also: Best Probiotic Brand For Ulcerative Colitis
Also Check: Can You Eat Oatmeal With Ulcerative Colitis
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
- Alcohol.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Salt.
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
How Is Ulcerative Colitis Diagnosed
To diagnose ulcerative colitis in children, teenagers and adults, your healthcare provider has to rule out other illnesses. After a physical exam, your provider may order:
- Blood tests: Your blood can show signs of infection or anemia. Anemia is a low level of iron in your blood. It can mean you have bleeding in the colon or rectum.
- Stool samples: Signs of infection, parasites , and inflammation can show up in your poop.
- Imaging tests: Your healthcare provider may need a picture of your colon and rectum. You may have tests including a magnetic resonance imaging scan or computed tomography scan.
- Endoscopic tests: An endoscope is a thin, flexible tube with a tiny camera. Specialized doctors can slide the endoscope in through the anus to check the health of the rectum and colon. Common endoscopic tests include colonoscopy and sigmoidoscopy.
Read Also: How To Find Out If You Have Ulcerative Colitis
What Supplements Should You Take For Crohn’s Disease Vs Ulcerative Colitis
Crohn’s disease nutritional diet deficiencies
- Your need for vitamin and mineral supplements depends on several factors, your diet, which parts of your digestive tract are affected, and whether you have had surgery on your small intestine.
- The most common vitamin deficiencies are
- vitamins D and B-12.
Ulcerative colitis nutritional deficiencies
As with Crohns disease, nutrition is important if you have ulcerative colitis because symptoms of diarrhea and bleeding can lead to dehydration, electrolyte imbalance, and loss of nutrients. It may be necessary to take nutritional supplements if your symptoms do not allow you to eat a nutritionally balanced diet. Talk to your health-care professional about what supplements to take.
What Are Causes To Bleeding Ulcers In The Stomach
Causes Use of NSAIDs. High doses of common NSAIDs such as ibuprofen and aspirin may cause peptic or bleeding ulcers. H. pylori infection. Zollinger-Ellison syndrome Zollinger-Ellison syndrome is an uncommon condition that causes tumors in the stomach, duodenum, or pancreas. Ulcers with other causes.
Don’t Miss: How To Heal Ulcerative Colitis Flare
What Makes This Hemorrhoids Breakthrough So Exciting Is That It Gives You The Power Todifference Between Hemorrhoid And Colitis
Difference Between Hemorrhoid and Colitis Hemorrhoid No MoreT is a 150 page downloadable e-book, jam-packed cover to cover with all the secret natural Hemorrhoids cure methods, unique powerful techniques and the step-by step holistic Hemorrhoids system Ive discovered in over 14 years of research. This program contains all the information youll ever need to eliminate your Hemorrhoids permanently in weeks, without using drugs, without surgery and without any side effects.
Ibs & Ibd Can Aggravate Hemorrhoids
Regardless of whether a patient suffers from IBS or IBD, both conditions can aggravate hemorrhoids in patients, leading to further discomfort. Aggravation typically occurs from some medications, aggressive wiping, sitting on the toilet for too long, and pressure on the veins and anus from constipation.
Read Also: Can Ulcers In The Colon Be Cancerous
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Recommended Reading: What Is Good For Ulcers In Your Mouth
Can Ibd Patients Develop Hemorrhoids
Yes, you can develop hemorrhoids if you have IBD. In fact, people with Crohns disease are more likely to develop hemorrhoids.
Thats because some patients with Crohns disease can experience persistent constipation. This increases the pressure inside the body and compresses the veins in the anus, which leads to the development of hemorrhoids.
Hemorrhoids in Crohns can be treated like regular hemorrhoids .