Contributions Of Editorial Base:
Nicky Cullum: edited the protocol advised on methodology, interpretation and protocol content. Approved the final protocol prior to submission. Sally BellSyer: coordinated the editorial process. Advised on methodology, interpretation and content. Edited the protocol. Ruth Foxlee: designed the search strategy and edited the search methods section.
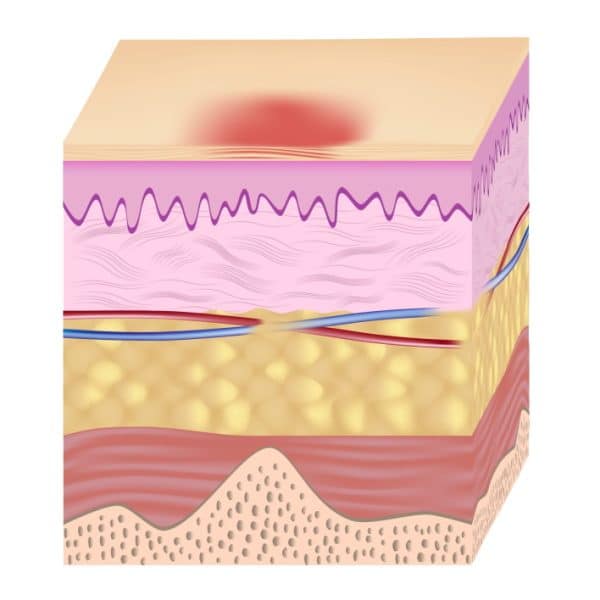
How Pressure Ulcers Develop
Pressure ulcers can develop when a large amount of pressure is applied to an area of skin over a short period of time. They can also occur when less pressure is applied over a longer period of time.
The extra pressure disrupts the flow of blood through the skin. Without a blood supply, the affected skin becomes starved of oxygen and nutrients, and begins to break down, leading to an ulcer forming.
Pressure ulcers tend to affect people with health conditions that make it difficult to move, especially those confined to lying in a bed or sitting for prolonged periods of time.
Conditions that affect the flow of blood through the body, such as type 2 diabetes, can also make a person more vulnerable to pressure ulcers.
Learn more about the causes of pressure ulcers.
Positioning And Support Surfaces
Preamble: Pressure and compression to soft tissue play a role in the etiology of pressure ulcers. Patient positioning and methods to reduce pressure-related tissue damage are recognized as important treatment components. While there are limited definitive studies, the best current evidence and expert opinion suggest the following guidelines.
Guideline #1.1: Establish a repositioning schedule and avoid positioning patients on a pressure ulcer.
Principle: Pressure ulcers are thought to result from compression of soft tissues against a bony prominence. It is reasonable to assume that pressure on an ulcer can result in delayed healing. Patients should be repositioned to relieve pressure over bony prominences. The exact turning interval is not known and is derived empirically. Reductions in pressure incidence have been achieved, but positioning is not universally effective.
Evidence:
You May Like: Ulcerative Colitis Symptoms Mayo Clinic
Compensation For Stage 2 Bedsores
You may be able to access compensation for stage 2 bedsores by taking legal action against a nursing home and its staff.
Nursing home compensation can help pay for:
- Medical treatments
Breaking News for Older Veterans: President Biden Signs The PACT Act
The vast majority of Americans are united in believing that older adults, especially veterans and their loved ones, should receive quality care and dignity from a grateful nation. Horrifyingly, we have documented the dangers of nursing home abuse of military veterans, shining a light in dark places to expose the truth. We rarely get toRead More
Elder abuse is considered a serious crime, but it often goes unreported. Older adults and their loved ones may be afraid that reporting abuse will lead to worse treatment. Thankfully, there are laws at both the federal and state levels to ensure punishments for elder abuse are carried out. Learn more about what to doRead More
Handling Abuse Allegations in Nursing Homes
Nursing home abuse is a serious claim that many people may feel uncomfortable making. However, because nursing home residents are usually frail and often cannot defend themselves, all allegations of abuse must be taken seriously. Learn how to handle abuse allegations in nursing homes and keep your loved one safe. Nursing Home Abuse Allegations: WhatRead More
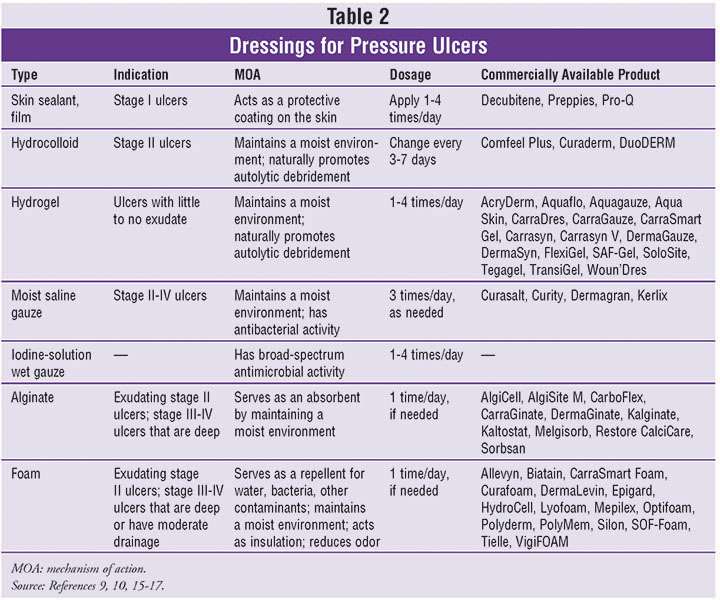
What Kind Of Dressing Do You Use On A Stage 4 Pressure Ulcer
If a pressure ulcer is at-risk of infection or has become infected, an antimicrobial silver foam dressing may be helpful. Alternatively, a silver alginate dressing in combination with a foam dressing may be used. It is important to select a debridement method most appropriate to the persons condition.
You May Like: Nursing Interventions For Pressure Ulcers
What Types Of Wound Dressing Can Be Used On Bed Sores
By Nursing Home Law Center
In order for bed sores to heal, attention must be paid to the removing dead tissue and protecting the wound from infection causing bacteria. Dressings are usually applied to help the body heal itself. The type of dressing and the frequency with which it is to be changed is ordered by a physician with the application and changes carried out by nurses.
Many patients with bed sores suffer additional harm when the staff responsible for caring for them fails to follow medical orders with respect to the frequency with which dressings are to be changed. If dressings are not changed according to orders set forth by a physician, the healing of the bed sores may be delayed and perhaps become infected.
The most commonly used dressings used to treat bed sores include:
Absorptive Dressings: These dressings are either applied directly to the wound or on top of other primary dressings. Absorptive dressings are intended to remove the drainage from the bed sore that may impede healing. Most absorptive dressings are changed on a daily basis. However, excessive drainage from a bed sore may require more frequent dressing changes.
Common types of Absorptive dressings include: Medipore, Silon Dual Dress, Aquacel Hyrofiber Combiderm, Absorbtive Border, Multipad Soforb, Iodoflex, Tielle, Telefamax, Tendersorb, Mepore and Exu-dry.
Related Information
Also Check: Does Colectomy Cure Ulcerative Colitis
What Are The Causes Of Pressure Injuries
Pressure injuries are caused when a force is applied to the skin, causing damage to the tissue. Several types of force include:
- Pressure: Constant pressure on the skin results from remaining in the same position for a prolonged period of time.
- Shear: Shear damage or a dragging force can occur when the head of the bed is raised and the body slides down. The skin sticks to the sheets, but internal structures are damaged.
- Moisture: Fluids that remains on the skin can cause the skin to become overly wet, which increases the risk for pressure injury development.
You May Like: Are Mouth Ulcers A Sign Of Hiv
Severity Of Pressure Ulcers
Healthcare professionals use several grading systems to describe the severity of pressure ulcers most common is the EPUAP grading system. Pressure sores are categorised into four stages corresponding to the depth of damage. It must however be emphasised that when an eschar is present, accurate staging is not possible.
How Can I Tell If I Have A Pressure Sore
- First signs. One of the first signs of a possible skin sore is a reddened, discolored or darkened area . It may feel hard and warm to the touch.
- A pressure sore has begun if you remove pressure from the reddened area for 10 to 30 minutes and the skin color does not return to normal after that time. Stay off the area and follow instructions under Stage 1, below. Find and correct the cause immediately.
- Test your skin with the blanching test: Press on the red, pink or darkened area with your finger. The area should go white remove the pressure and the area should return to red, pink or darkened color within a few seconds, indicating good blood flow. If the area stays white, then blood flow has been impaired and damage has begun.
- Dark skin may not have visible blanching even when healthy, so it is important to look for other signs of damage like color changes or hardness compared to surrounding areas.
- Warning: What you see at the skins surface is often the smallest part of the sore, and this can fool you into thinking you only have a little problem. But skin damage from pressure doesn’t start at the skin surface. Pressure usually results from the blood vessels being squeezed between the skin surface and bone, so the muscles and the tissues under the skin near the bone suffer the greatest damage. Every pressure sore seen on the skin, no matter how small, should be regarded as serious because of the probable damage below the skin surface.
Recommended Reading: How To Treat Equine Ulcers
When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
Wound Care: Pressure Ulcer Best Practices
Pressure ulcers, otherwise known as decubitus ulcers, comprise a significant portion of wounds requiring specialized care and presenting additional costs, so prevention is critically important. A pressure ulcer is any lesion caused by unrelieved pressure resulting in damage of underlying tissue. Pressure ulcers usually occur over bony prominences and are graded or staged to classify the degree of tissue damage observed. Stage 1 pressure ulcers are defined as nonblanchable erythema of intact skin the heralding lesion of skin ulceration. Stage 2 is defined as partial thickness skin loss involving epidermis and/or dermis Stage 3 as full thickness skin loss involving damage or necrosis of subcutaneous tissue that may extend down to, but not through, underlying fascia and Stage 4 as full thickness skin loss with extensive destruction, tissue necrosis or damage to muscle, bone or supporting structures.
The Wound, Ostomy and Continence Nurses Society says that pressure ulcer prevention is best accomplished by identifying patients who are at risk for the development of pressure ulcers and initiating early preventive measures. According to the WOCN, This requires an understanding of risk factors, the utilization of research-based risk assessment tools, knowledge of appropriate preventive strategies and access to essential medical equipment such as therapeutic support surfaces.
Related Content:
Recommended Reading: Compression Stockings For Leg Ulcers
Identifying A Stage 2 Bedsore
Stage 2 bedsores can be identified as an intact blister or shallow open sore. These sores are often red or pink and surrounded by red and irritated skin. These sores may also be moist if pus or fluid is present.
Human skin is made up of layers. The topmost level is called the epidermis. A stage 2 sore has broken the epidermis to create an open wound. The second layer of skin, the dermis, is visible in stage 2. In some cases, the dermis is broken.
Stage 2 bedsores have broken the skin but have not broken past the dermis to fat. The deeper a sore goes, the more difficult it will be to treat and the longer it will take to heal. People who are at risk of developing bedsores should receive regular skin checks to identify bedsores before they progress past stage 2.
Signs of a stage 2 bedsore include:
- Intact or ruptured blister
- Redness or discoloration
Identifying a stage 2 sore as soon as possible is imperative. Complications can occur when bedsores go unnoticed and untreated. In serious situations, bedsores can become life-threatening or lead to amputation. If a sore becomes infected, the infection can spread to the blood, heart, or bones.
Notify a doctor or other healthcare provider if you or a loved one has developed a stage 2 bedsore. A health professional can decide the best plan of action to treat the bedsore properly.
Who Is At Risk For A Stage 2 Bedsore
Nursing home residents that rely on staff members to help them move are at a higher risk of stage 2 bedsores. Other factors, described below, can also put seniors at risk of bedsores.
Certain Medical ConditionsJohns Hopkins Medicine notes that elders with circulation issues and diabetes are more likely to suffer from bedsores.
IncontinenceThe U.S. National Library of Medicine notes that incontinence can make skin problems more likely. Feces and urine can make nearby skin moist, increasing the risk of irritation. Further, adult diapers can trap waste, allowing them to damage skin unless they are quickly changed.
MalnourishmentMalnourishment reduces overall health and weight two factors that make bedsores more likely. It also may take longer for someone to heal from a bedsore if theyre malnourished and underweight.
Read Also: Irritable Bowel Syndrome Ulcerative Colitis
What Are The Stages Of A Pressure Injury
There are four stages that describe the severity of the wound. These stages include:
- Stage 1: This stage is discolored skin. The skin appears red in those with lighter skin tones and blue/purple in those with darker skin tones. The skin does not blanch when pressed with a finger.
- Stage 2: This stage involves superficial damage of the skin. The top layer of skin is lost. It may also look like a blister. At this stage, the top layer of skin can repair itself.
- Stage 3: This stage is a deeper wound. The wound is open, extending to the fatty layer of the skin, though muscles and bone are not showing.
- Stage 4: This stage is the most severe. The wound extends down to the bone. The muscles and bone are prone to infection, which can be life-threatening.
Assessing Sacral Pressure Ulcers
Pressure-induced skin and soft tissue injuries are often classified using the National Pressure Ulcer Advisory Panel staging system . Under this rubric, the wound should be staged to its deepest extent. This means selecting the highest number stage that accurately describes any part of the wound.
- Stage 1 Pressure Injury: Non-blanchable erythema of intact skin
- Non-blanchable is redness that stays despite applying pressure. This means the erythema is not caused by blood within capillaries . Purple or maroon discoloration is not part of stage 1, but rather indicates a deep tissue pressure injury.
Recommended Reading: Natural Supplements For Ulcerative Colitis
The Available Reconstructive Options Are
Split thickness skin grafting
When the ulcer is superficial and vital tissues such as bone, vessels, nerves or tendons are not exposed, and the ulcer is not copiously discharging, skin grafting is the first option for surgical treatment. The slimy layer over the surface of ulcer is sharply debrided to get a healthy vascular bed for skin grafting.
Local flaps
Variety of local flaps can be used to reconstruct the defect created by excision of pressure ulcers. Local transposition, rotation, limberg flap are the available options .3]. Biceps femoris V-Y advancement for ischial pressure sore and perforator based V-Y advancement is another good options if the anatomy permits .
Sacral pressure sore , debridement and cover by local perforator based V-Y advancement flaps , 1-month post-operative , recurrence on the flap after 11 years due to loss of family support and subsequent improper care. Another patient with the same flap after 16-year of follow-up with a proper weight shifting and care showing stable coverage
Regional flaps
Medial planter flap for heel sore: A long-standing deep trophic ulcer of heel . The islanded medial planter flap was transposed to the defect and the resultant donor site was covered by split thickness skin graft . The 1-week and 3-month post-operative pictures showing stable coverage. Patient allowed full weight bearing from 6th week along with silicone footpad protection
Microvascular free flaps
Description Of The Condition
Pressure ulcers, also known as pressure injuries, bedsores, decubitus ulcers or pressure sores, are localised areas of injury to the skin, the underlying tissue or both. They often occur over bony prominences such as the sacrum and heel , and are caused by external forces such as pressure, or shear, or a combination of both .
Risk factors for pressure ulcer development have been summarised into three main categories: a lack of mobility poor perfusion and low skin status the latter category includes the presence of stage 1 pressure ulcers or incontinence or both, which also increases the risk of ulceration by producing a detrimental environment for the skin .
Prevalence
Pressure ulcers are one of the most common types of complex wound. Prevalence estimates differ according to the type of population assessed, the data collection methods used and period of data collection and whether Stage 1 ulcers were included).
One large European study estimated a hospital pressure ulcer prevalence of 10.5% whilst a US study estimated a prevalence of 9.0% across acutecare, longterm care and rehabilitation settings ). In the UK, national pressure ulcer data are collected across community and acute settings as part of the National Health Service Safety Thermometer initiative . About 4.4% of patients across these settings were estimated to have a pressure ulcer in November 2014 .
Treatments for pressure ulcers
Impact of pressure ulcers on patients and financial costs
Recommended Reading: Fish Oil And Ulcerative Colitis
Symptoms Of Stage 2 Pressure Ulcers
Stage 2 pressure ulcers are shallow with a reddish base. Adipose and deeper tissues are not visible, granulation tissue, slough and eschar are not present. Intact or partially ruptured blisters that are a result of pressure can also be considered stage 2 pressure ulcers. Note that causes of erosion, ulceration, or blistering that aren’t a result of pressure are not included in the definition of a stage 2 ulcer.
Stage 4 Bedsore Prevention
The best way to prevent a stage 4 bedsore is by being proactive. If your loved one is at risk for bedsores, you can help them take the following precautions.
To prevent stage 4 bedsores, you can:
- Avoid buttons on clothes and wrinkles in bedding
- Avoid doughnut cushions, as they can add pressure to surrounding areas
- Change bedding and clothing on a regular basis
- Check skin daily
You May Like: Ulcerative Colitis Surgery Recovery Time
Don’t Miss: Signs Of Ulcers In Humans