Why It Is Important To Do This Review
The diversity of dressings and related materials available to health professionals for treating pressure ulcers makes evidencebased decisionmaking difficult when determining the optimum treatment regimen for a particular patient . With increasingly sophisticated technology being applied to wound care, practitioners need to know the relative effectiveness and costeffectiveness of these sometimes expensive dressings. Even where cost is not an issue, the most effective treatment may not be available or may be difficult or to use, so that information on the second and third best treatments is important too .
Current evidence syntheses include four Cochrane Reviews , two other systematic reviews , and two recent clinical guidelines . Each of these consists of a series of pairwise comparisons. No review finds clear evidence of any effect of one dressing compared to another in terms of assessed outcome measures, including complete wound healing.
In the absence of an overview or network metaanalysis, decisionmakers have to consider the findings of multiple pairwise randomised controlled trials simultaneously and qualitatively to judge, in the face of uncertainty, which dressing they might decide to use. It is extremely difficult to do this effectively, and this difficulty is compounded when the evidence comprises single small trials, about which decisionmakers may have little confidence.
A glossary of NMA terms is given in .
How Do I Use Medihoney
Before applying a MEDIHONEY product to your loved ones wound, carefully read the instructions on the packaging. Once you do, follow these simple steps:
-
Thoroughly clean the wound with a saline solution. . Then, if necessary, apply a barrier cream around the edges of the wound. Barrier cream prevents skin breakdown and infection.
-
Apply the MEDIHONEY gel or paste directly to the wound. If youre using a calcium alginate dressing, use sterile scissors to resize it, and then gently apply the dressing to the wound bed.
-
Cover the MEDIHONEY gel, paste, or alginate dressing with an absorbent sterile, secondary bandage or a compression garment.
-
When its time to change the dressing, thoroughly clean the wound with a saline solution. Once you do, repeat the same steps.
This video by YouTuber Alyssa McTavish demonstrates the entire process:
Keep in mind that its best that MEDIHONEY be on the skin for 12-24 hours at a time for maximum effectiveness. If you or your loved one is having a hard time keeping the dressing intact, soak a gauze dressing in the MEDIHONEY and apply it directly on the wound, then top with an abdominal pad dressing.
Also Check: Does Ulcerative Colitis Increased Risk Of Colon Cancer
How To Treat A Stage One Pressure Ulcer
Once a stage one ulcer has been diagnosed, there are several immediate actions that can stop its progression to open woundor decubitus ulcerwhich requires urgent wound care.
The first step should always be thorough pressure injury risk assessment using your hospitals existing assessment protocol/procedure, or better yet, by integrating technology that continuously monitors risk from the beginning of a patients stay.
To treat an existing injury, its important to reduce pressure on the area of affected skin immediately. This may involve turning the patient and/or using a specific mattress topper or material that helps redistribute pressure on the patients skin.
Stage one pressure ulcers require hospital staff to work fast. While the sores need not induce panic, they can become a considerable problem should they move into stage two. That, along with the possibility of already-sustained tissue damage, should encourage health care professionals to immediately implement preventative measures.
You May Like: How Many People Have Ulcerative Colitis
Stage 3 Pressure Injury: Full
Stage 3 pressure injuries involve full-thickness loss of skin, where fat tissue is visible and granulation tissue, rolled wound edges , and eschar may also be present. However, fascia, muscle, tendon, ligament, cartilage, and bone are not exposed. The depth of tissue damage may vary by anatomical location areas with significant amounts of fat are at risk of developing deeper wounds. For visual reference, see illustrations of pressure injuries from the NPUAP here.
Stages Of Pressure Ulcers And Treatment
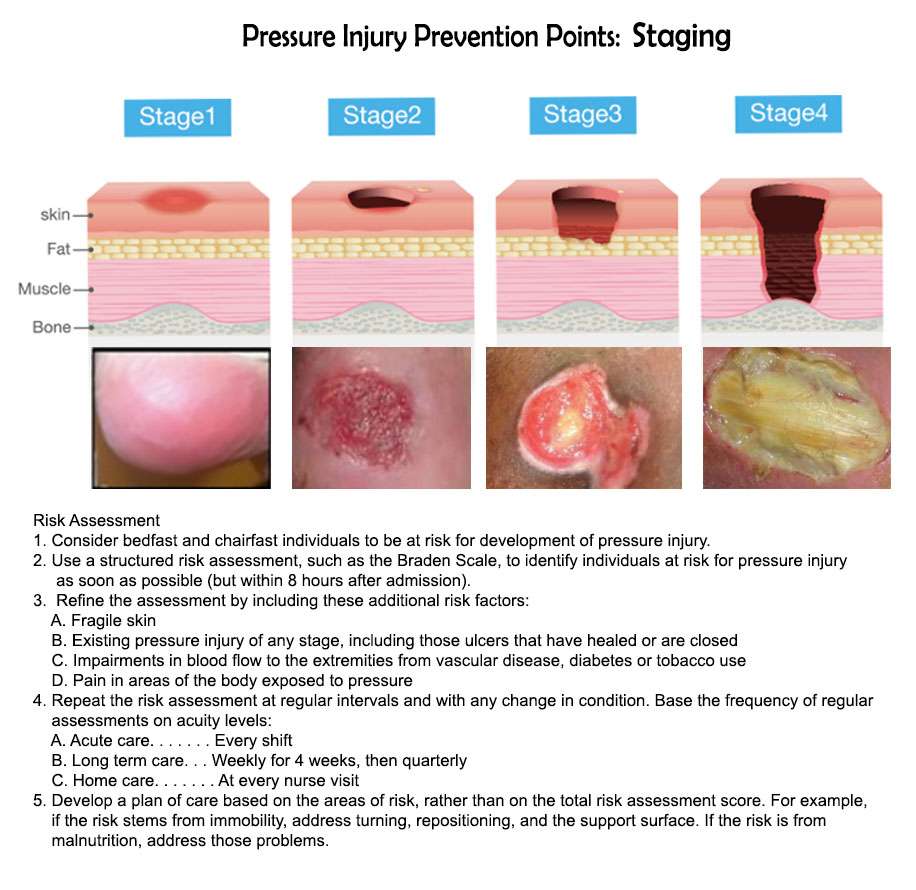
Pressure ulcers can progress in four stages based on the level of tissue damage. These stages help doctors determine the best course of treatment for a speedy recovery.
If caught very early and treated properly, these sores can heal in a matter of days. If left untreated, severe bedsores may require years to heal.
Read Also: Foods You Can Eat With An Ulcer
Stage 2 Pressure Injury: Partial
In stage 2 pressure injuries there is a partial-thickness loss of skin with exposed dermis. The wound bed is pink or red, moist, and may also present as an intact or ruptured serum-filled blister. Fat and deeper tissues are not visible. Connective granulation tissue and eschar are also not present. Stage 2 injuries are a common result of an adverse microclimate and shear in the skin. For visual reference, see illustrations of pressure injuries from the NPUAP here.
What Is A Pressure Injury
A pressure injury is an area of injured skin. A pressure injury happens when force is applied on the surface of the skin. This force can be a constant pressure on an area of skin or a dragging force between the skin and another surface. These injuries usually happen over bony parts of the body . A pressure injury can become life-threatening if it advances to a deep wound or becomes infected.
Recommended Reading: Ulcer Signs Symptoms And Treatment
What Are The Causes Of Pressure Injuries
Pressure injuries are caused when a force is applied to the skin, causing damage to the tissue. Several types of force include:
- Pressure: Constant pressure on the skin results from remaining in the same position for a prolonged period of time.
- Shear: Shear damage or a dragging force can occur when the head of the bed is raised and the body slides down. The skin sticks to the sheets, but internal structures are damaged.
- Moisture: Fluids that remains on the skin can cause the skin to become overly wet, which increases the risk for pressure injury development.
Here Are The Signs Of Stage One Ulcer Development
Its no secret that pressure sores are a major issue in hospitals and health care institutions nationwide. When it comes to pressure injury development in hospitals, people across the United States are certainly not alone. Every year, 2.5 million people develop hospital acquired pressure ulcers and 60,000 die of complications. Of high concern: up to 45% of these HAPU injuries are developed on the surgical table of operating rooms. With pressure sores and injuries being such a prevalent issue, we must pay attention to the early signs of their development this is key to prevent them from worsening to further injury and even death.
Of all the factors that go into pressure sore development, one thing is clear: by learning to identify the early signs of a bed sore and take appropriate actionparticularly during the first stage of its developmentmore serious pressure injuries can be limited.
At XSENSOR, our technology and products help healthcare professionals monitor risk of pressure ulcer development from the very beginning. Were working toward a reality where stage one pressure ulcers are the only injuries we seeif that.
Recommended Reading: How To Treat Skin Ulcer On Leg
The 4 Stages Of Ulcers
When we cut or scrape our skin, our cells require adequate blood flow to that area in order to heal the wound. This blood delivers clotting agents that stop the wound from bleeding, in addition to oxygen and nutrients that allow new skin cells to grow. Wounds or sores that do not heal properly are called ulcers. Ulcers may form on our feet for a few different reasons, including narrow blood vessels or constant pressure on a particular area. Individuals with poor circulation, like smokers or diabetics, are more prone to foot ulcers.
Ulcers, like any other break in your skin, should be taken seriously because they can become infected. However, the development of an ulcer is a progressive process, and each stage comes with different signs and symptoms. Here are some brief differences between each stage:
- Stage 1: The skin becomes red and irritated where there is pressure, and does not go away when the pressure is relieved. Pain and discomfort are common.
- Stage 2: The skin is broken for the first time. The sore may look like a blister or a shallow crater, and is typically painful and tender.
- Stage 3: The ulcer penetrates even deeper into the tissue underneath the skin, possibly exposing fat cells. There may be no pain due to severe nerve or tissue damage.
- Stage 4: The sore is now so deep that it reaches the muscles, bones, or tendons. Infections and other serious complications may occur. As with a Stage 3 ulcer, it is possible that the individual feels no pain.
What Exactly Is A Pressure Injury
A pressure injury is defined as an injury to the skin and underlying tissue resulting from prolonged pressure.
They most often develop on skin that covers bony areas of the body, such as the heels, ankles, hips, and tailbone, and are most common in patients with limited mobility such as the elderly, nursing home patients, patients in a coma, patients with reduced pain perception, and any patients who cannot move specific parts of their body.
In 2016 the National Pressure Ulcer Advisory Panel amended the official name from âpressure ulcerâ to âpressure injuryâ to more accurately reflect the fact that open ulceration does not always occur, and pressure injuries can describe both intact or ulcerated skin.
Recommended Reading: Natural Remedies For Mouth Ulcers
When Should I Call The Doctor
If you suspect you have a pressure injury, speak with your doctor. A pressure injury is easier to heal if it is discovered in the early stages. It is important to prevent a wound from becoming infected. Healing is delayed in an infected wound and the infection could cause problems in other areas of the body.
What Are The Stages Of A Pressure Sore
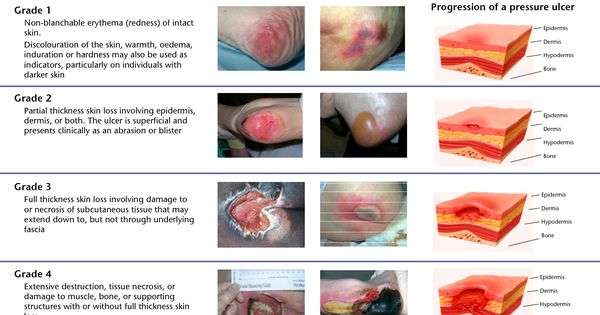
Pressure soresinjuries to the body coming from prolonged pressure exposurefall into one of four main categories, or stages. Whether a stage one ulcer, where the skin is just beginning to show damage, or a stage four ulcer, with open wounds, sores and signs of infectionthey all need to be treated with urgency. Here are the four stages of a pressure sore.
Stage 1 Pressure Sores and Ulcers: Early on in pressure ulcer development, the skin is developing injury. While no open sores or broken skin are present yet, skin may appear redder, warmer or firmer than usual. Known as a non-blanchable erythema of intact skin, the color change may indicate the beginnings of a serious injury to the deep tissue.
Stage 2 Pressure Sores and Ulcers: This is where the true sore, or ulcer, develops as a break in the skin. It is often very painful, and can create serious damage within the skin. Known as partial-thickness skin loss with exposed dermis, these bed wounds can quickly become something worse.
Stage 3 Pressure Sores and Ulcers: In stage three, the pressure ulcer has developed into the soft tissue underneath the skin. Known as full-thickness skin loss, this stage may showcase a deep wound, especially in an area with more adipose tissue.
Read Also: Rice Recipes For Ulcerative Colitis
Faqs For Pressure Ulcer Staging
Staging pressure ulcers can be challenging. Below are some common questionsand answersabout staging.
Q. If a pressure ulcer heals , but later reopens at the same site, how should it be staged?
A. According to the National Pressure Ulcer Advisory Panel, if a pressureulcer reopens in the same site, the ulcer should be listed at the previous stagingdiagnosis .1Remember that pressure ulcers heal to a progressively more shallow depth. They dont replace lost muscle, subcutaneous fat, or dermis before they reepithelialize. Instead, the full-thickness ulcer is filled with scar tissue composed primarily of endothelial cells, fibroblasts, collagen, and extracellular matrix. A Stage IV pressure ulcer, therefore, cant become a Stage III, Stage II, or subsequently Stage I pressure ulcer.1
Q. Can pressure ulcer staging be used for venous ulcers?
A. No. The National Pressure Ulcer Advisory Panel and European Pressure Ulcer Advisory Panel state that a pressure ulcer classification system cant be used to describe tissue loss in wounds other than pressure ulcers.2
Q. If a wound first presents as a suspected deep-tissue injury and then becomes open, should I chart it as a healing SDTI or restage it as it presents?
Q. Once a pressure ulcer is debrided, does it become a surgical wound and no longer need staging?
Q. What would be the new stage for a Stage II pressure ulcer that develops slough?
Q. Can a patient have a friction wound without pressure?
How Can I Tell If I Have A Pressure Sore
- First signs. One of the first signs of a possible skin sore is a reddened, discolored or darkened area . It may feel hard and warm to the touch.
- A pressure sore has begun if you remove pressure from the reddened area for 10 to 30 minutes and the skin color does not return to normal after that time. Stay off the area and follow instructions under Stage 1, below. Find and correct the cause immediately.
- Test your skin with the blanching test: Press on the red, pink or darkened area with your finger. The area should go white remove the pressure and the area should return to red, pink or darkened color within a few seconds, indicating good blood flow. If the area stays white, then blood flow has been impaired and damage has begun.
- Dark skin may not have visible blanching even when healthy, so it is important to look for other signs of damage like color changes or hardness compared to surrounding areas.
- Warning: What you see at the skins surface is often the smallest part of the sore, and this can fool you into thinking you only have a little problem. But skin damage from pressure doesn’t start at the skin surface. Pressure usually results from the blood vessels being squeezed between the skin surface and bone, so the muscles and the tissues under the skin near the bone suffer the greatest damage. Every pressure sore seen on the skin, no matter how small, should be regarded as serious because of the probable damage below the skin surface.
Also Check: Ulcerative Colitis Biologics Side Effects
Stages Of Pressure Ulcers
Casey Gallagher, MD, is board-certified in dermatology and works as a practicing dermatologist and clinical professor.
If a loved one has been severely injured or is extremely ill, they may need to spend a significant amount of time in bed. Prolonged immobility, while beneficial to recovery, can become problematic if it places persistent pressure on vulnerable skin. Unless preventive steps are taken, pressure ulcers, also known as decubitus ulcers or bedsores, can develop.
Stage 1 Pressure Injury: Non
In stage 1 pressure injuries the skin is still intact with a localized area of redness that does not turn white when pressure is applied . Stage 1 does not include purple or maroon discoloration these may indicate deep tissue pressure injury. For visual reference, see illustrations of pressure injuries from the NPUAP here.
Also Check: Ulcers In Small Bowel Crohn’s
The 7 Most Asked Questions About Medihoney
MediHoney® dressings are made with a special honey that is derived from the nectar of the Leptospermum plant. This type of honey has unique properties that have been scientifically verified and shown in clinical trials and by other clinical evidence to be effective for the management of wounds and burns.1-3
In one randomized controlled trial, the mean healing time of wounds treated with MediHoney dressings was significantly faster than the mean healing time of wounds treated with conventional dressings.4
Unlike regular honey, MediHoney is controlled against a rigorous set of systems and standards, including independent monitoring and auditing, to guarantee quality and batch-to-batch consistency. It is also ultra-filtrated and sterilized by gamma irradiation, removing any bacterial spores without loss of product effectiveness.3 MediHoney comes from a traceable source and is free of pesticides and antibiotics.3
Here are the 7 most asked questions about this dressing:
MediHoney dressings aids and supports autolytic debridement and a moist wound healing environment in acute and chronic wounds and burns,5-8 through two key mechanisms high osmolarity and low pH. The high sugar content of honey facilitates movement of fluid from an area of higher concentration, across a membrane, to an area of lower concentration. Osmotic potential draws fluid through the wound, to the surface, helping to liquefy non-viable tissue.
How To Use It On The Wound:
Clean: Clean the wound with saline water. Apply: Directly apply the honey gel to the wound bed. Ensure it is in full contact with the wound bed and has approximately 3mm thickness. It is recommended to pair MEDIHONEY® with XTRASORB®, which is a super absorbent cover dressing. Its osmotic gradient pulls exudate to the back of the dressing and converts it into a gel, locking it away even under compression!Whatever you choose, the secondary dressing should be sufficiently absorbent to accommodate the volume of wound exudate. Change: Periodically change the dressing. Do it gently. If the dressing is dry and sticking to the wound bed, moisten it first with normal saline or sterile water. Generally, this antibacterial gel can be left on the wound for up to 7 days depending on the exudate levels. The frequency of changing depends a lot of the amount of drainage coming from your wound. If there is a lot of fluid and the dressing becomes saturated, it may need to be changed more frequently.
Recommended Reading: Can An Ulcer Make You Nauseous