Is It An Ulcer Or Gerd
These two common digestive health problems are easily confused. Find out how doctors can tell the difference.
That burning sensation in your stomach could be an ulcer or it might be gastroesophageal reflux disease , a chronic acid reflux condition.
Either way, you should schedule a doctors visit to find out whether you have GERD or an ulcer. Both ulcers and GERD can be treated with the help of a gastroenterologist.
Ulcer or GERD: Stomach Discomfort
The two conditions are actually different, even if they make you feel equally miserable. By some estimates, one in five people experience heartburn at least weekly. Stomach discomfort can easily have a negative effect on your life, leading to:
- Lost sleep
- Problems with eating and drinking
Ulcer or GERD: Understanding the Differences
An ulcer is a small sore or lesion in the lining of your stomach or duodenum, the first part of your intestine. This sore is often aggravated by your stomach acid, but is usually not caused by the acid itself. More likely, the cause is either a bacterium known as Helicobacter pylori or taking non-steroidal anti-inflammatory drugs .
GERD, on the other hand, means that your stomach acid is coming up from your stomach into your esophagus, causing a burning sensation and unpleasant taste in the back of your mouth. This has to occur at least twice a week to be considered GERD.
Ulcer or GERD: Know the Symptoms
An ulcer often comes with these symptoms:
Ulcer or GERD: Making the Diagnosis
Complications Of Peptic Ulcers
Left untreated, peptic ulcers can result in severe complications and emergencies.
- Internal bleeding You can have bleeding in your stomach, esophagus, or duodenum when the ulcer opens a blood vessel. Ulcers can cause bleeding that occurs slowly over time or quickly, possibly resulting in hemorrhaging that can be life-threatening due to shock. Sometimes you may not notice a bleeding ulcer until you become anemic, a condition in which your body lacks red blood cells because of inadequate iron. This occurs when ulcers cause chronic, low-grade blood loss.
- A hole, or perforation, in the stomach wall You can develop a perforated ulcer, which means it has eaten through your stomach or intestinal wall.
- Obstruction This is when you have swelling or scarring related to your ulcer that is preventing your food from being digested properly.
The signs that you are having an ulcer emergency are:
- Blood in stool
- Mental confusion
- Severe abdominal distension
If you think you or someone you know is having an ulcer emergency, seek immediate medical attention.
What Are The Common Side Effects Of Ulcer Medication
All medications may produce side effects, and side effects will vary depending on the type of medication. This is not a complete list of possible side effects, so consult with a healthcare professional about any concerns or questions you may have regarding your specific situation.
Proton pump inhibitors and H2 blockers are relatively safe medications available in prescription and over-the-counter formulations. The most commonly experienced side effects are digestive system problems such as abdominal pain, nausea, vomiting, diarrhea, and constipation. H2 blockers can also affect the central nervous system, so headaches, drowsiness, and dizziness are often experienced.
Proton pump inhibitors can reduce the absorption of calcium in the body, which can lead to an increased risk of osteoporosis and bone fractures. Patients will often be prescribed or recommended calcium supplements to take along with proton pump inhibitors. Other serious side effects of proton pump inhibitors may include kidney disease, vitamin B12 deficiency, and diarrhea caused by Clostridium difficile infection.
The most serious side effects of H2 blockers are related to their effects on the central nervous system. These side effects may include delirium, hallucinations, extreme drowsiness, and slurred speech.
Also Check: Best Foods To Eat When You Have A Stomach Ulcer
You May Like: Removing Colon Due To Ulcerative Colitis
How Is Barrett’s Esophagus Diagnosed
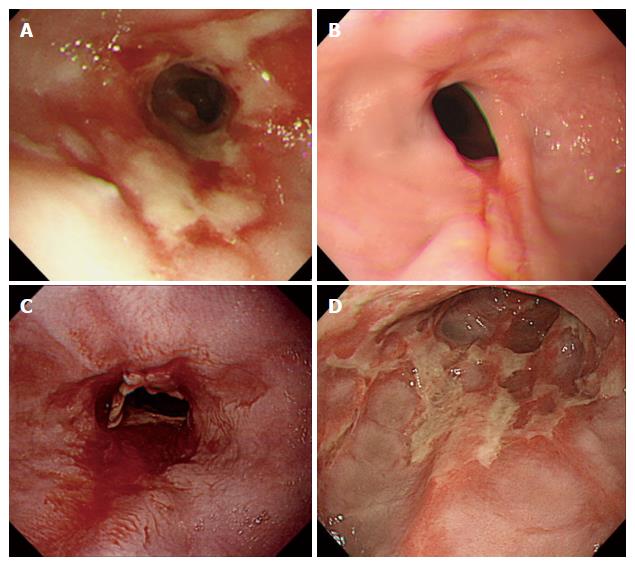
The only way to confirm the diagnosis of Barrett’s esophagus is with a test called an upper endoscopy. This involves inserting a small lighted tube through the throat and into the esophagus to look for a change in the lining of the esophagus.
While the appearance of the esophagus may suggest Barrett’s esophagus, the diagnosis can only be confirmed with small samples of tissue obtained through the endoscope. A pathologist will examine the tissue to make the diagnosis.
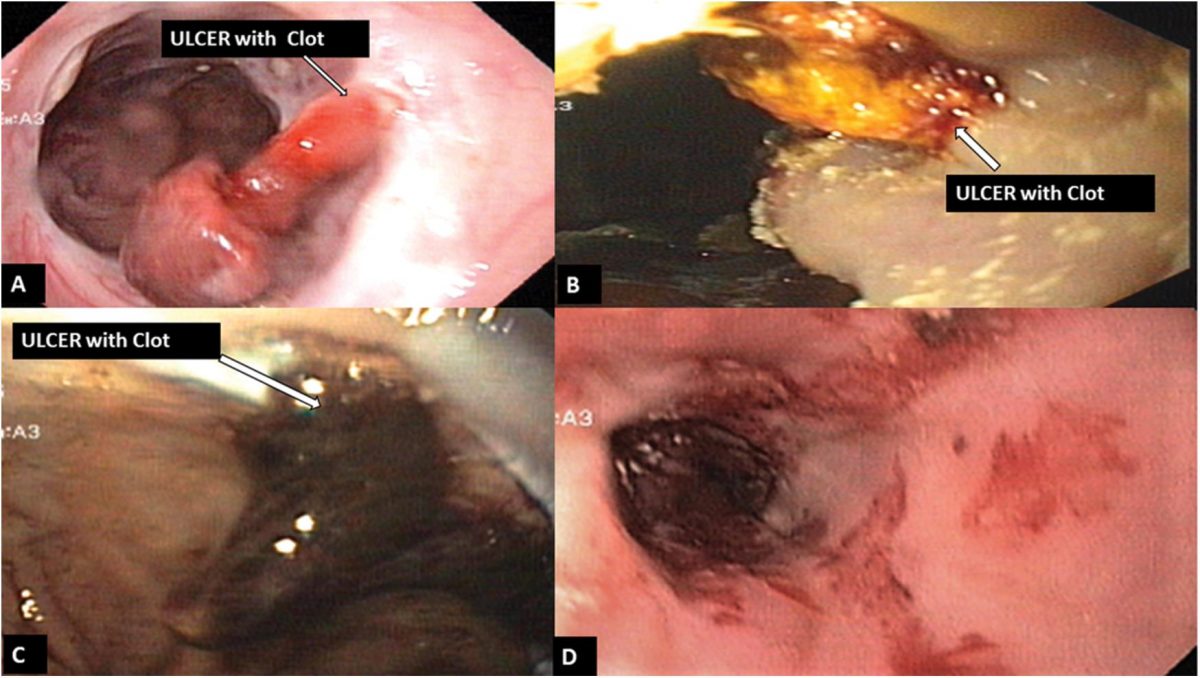
Diagnosis Of A Bleeding Ulcer
Early detection of the condition is quite challenging because the early symptoms are mild. It is for this reason that suspecting individuals should never disregard typical digestive tract symptoms and visit the doctor immediately for accurate diagnosis. Diagnosing the condition involves checking the medical history of the patient, conducting a physical exam and asking the patient about his/her symptoms. The doctor will then perform various tests to determine the location and severity of the ulcers, such as endoscopy, colonoscopy, esophagogastroduodenoscopy, Barium X-ray, sigmoidoscopy and anoscopy.
Also Check: How To Heal Ulcerative Colitis With Food
How To Recognize Gerd
GERD is a plumbing problem. It starts at the bottom of the esophagus, the tube that carries food from your mouth to your stomach.
When the valve at the bottom of your esophagus doesnt close properly, acid backs up and causes a painful burning sensation in your chest and throat. When youve got GERD, acid is coming back up and bathing your esophagus, instead of staying in the stomach where its supposed to be, says Dr. Brocato. That gives you a sensation of food coming up and irritation in your throat.
GERD is very common. According to the National Institutes of Health, it affects about 20% of Americans.
When Should You Call Or See A Doctor
If you think you have a stomach ulcer, call your doctor. Together you can discuss your symptoms and treatment options. If you dont already have a physician, you can use the Healthline FindCare tool to find a provider near you.
Its important to get a stomach ulcer taken care of because without treatment, ulcers and H. pylori can cause:
- bleeding from the ulcer site that can become life-threatening
- penetration, which occurs when the ulcer goes through the wall of the digestive tract and into another organ, such as the pancreas
- perforation, which occurs when the ulcer creates a hole in the wall of the digestive tract
- obstruction in the digestive tract, which is due to swelling of inflamed tissues
- stomach cancer, specifically
Symptoms of these complications can include those listed below. If you have any of these symptoms, be sure to call you doctor right away:
Also Check: What Foods To Eat If You Have An Ulcer
Best Natural Remedies For Healing Esophagus Damage After Acid Reflux
Hydrochloric acid is produced inside the stomach to aid in digestion, a process through which the food you eat is broken down into the different component nutrients. However, some people suffer from recurrent acid reflux where stomach acids travel up to the esophagus, causing irritation and inflammation. While some conventional treatments are recommended for this condition, it is advisable to seek for a long term solution. Besides medical treatment, why not also try natural treatment options. This discussion explores ways how to heal esophagus naturally.
When Should I Call My Healthcare Provider
See your healthcare provider right away if you have any of these symptoms:
- Vomiting blood or dark material that looks like coffee grounds
- Extreme weakness or dizziness
- Nausea or vomiting that doesnt get better, or gets worse
- A sudden, severe pain that may spread to your back
- Losing weight without even trying
Untreated peptic ulcers may cause other health problems. Sometimes they bleed. If they become too deep, they can break through your stomach.
Ulcers can also keep food from going through your stomach.
You May Like: How To Calm Down An Ulcerative Colitis Flare Up
What Is A Stomach Ulcer
A stomach ulcer, also called a gastric ulcer, is an open sore that develops in your stomach lining. You can also get one in your duodenum, the first part of the small intestine that your stomach feeds into. Duodenal ulcers and stomach ulcers are both types of peptic ulcers. Theyre named for pepsin, one of the digestive juices that are found in the stomach and that sometimes leak into the duodenum. These juices are a contributing factor in peptic ulcer disease.
Peptic ulcers occur when the protective mucous lining in your stomach and duodenum has been eroded, allowing gastric acids and digestive enzymes to eat away at your stomach and duodenal walls. This eventually results in open sores that are continually irritated by the acid. If left untreated, they can begin to cause serious complications, such as internal bleeding. Over time, they can even wear a hole all the way through. This is a medical emergency.
What Are The Complications Of Peptic Ulcers
Ulcers can cause serious problems if you dont get treatment.
The most common problems include:
- Bleeding. As an ulcer wears away the muscles of the stomach or duodenal wall, blood vessels may be hurt. This causes bleeding.
- Hole . Sometimes an ulcer makes a hole in the wall of your stomach or duodenum. When this happens, bacteria and partly digested food can get in. This causes infection and redness or swelling .
- Narrowing and blockage . Ulcers that are found where the duodenum joins the stomach can cause swelling and scarring. This can narrow or even block the opening to the duodenum. Food cant leave your stomach and go into your small intestine. This causes vomiting. You cant eat properly.
Don’t Miss: How To Treat Stage 4 Pressure Ulcer
Symptoms Of Peptic Ulcers
You may not have symptoms straightaway with an ulcer. Youre more likely to have a so-called silent ulcer if you are male, older, smoke, or are taking NSAIDs such as ibuprofen.
If you do have symptoms, a common one is abdominal pain or discomfort. You may also have pain in the middle of your back. If you have a duodenal ulcer , the pain tends to come on a couple of hours after a meal. Generally, it goes away when you eat again. You may also have pain that wakes you up at night when you have an empty stomach.
A gastric ulcer generally causes pain shortly after eating. Lying flat may relieve it. An oesophageal ulcer may cause abdominal or lower chest pain and make it difficult to swallow.
Indigestion is often a sign of a peptic ulcer. You may:
- feel or be sick
- have heartburn when the contents of your stomach go back up your oesophagus
Some symptoms may mean you have peptic ulcer complications. Or they can be caused by another medical condition, including cancer. You should see your GP urgently if you:
- are losing weight without dieting
- see blood in your vomit or your poo looks black and tar-like
- are very tired, as this may be caused by anaemia
- have trouble swallowing
- feel full soon after youve started eating
How To Spot Bleeding Stomach Ulcers
It is important to understand a few facts about peptic ulcers and bleeding from the upper gut. Firstly peptic ulcers refers to stomach ulcers and duodenal ulcers . Between the two, duodenal ulcers are more common. Secondly there are many possible causes of bleeding from the upper gut . A bleeding peptic ulcer is only one possible cause of upper gastrointestinal bleeding, albeit the most common.
Sometimes the signs and symptoms of an upper gastrointestinal bleed, like a bleeding ulcer, is overt and therefore obvious. It may be seen as fresh red blood in the vomit or similar to dark coffee grounds in the vomit. At other times the bleed is less obvious. A person may not vomit, may not seen any overt signs of bleeding and the bleed is discovered routinely with diagnostic investigations or when complications like anemia arise. Therefore there is no definitive way to spot a bleeding stomach ulcer in these cases without a medical assessment.
You May Like: How To Reduce Bloating With Ulcerative Colitis
Also Check: How You Know If You Have A Stomach Ulcer
What Is An Esophagus Ulcer
An esophagus ulcer is an open sore that forms on the lining of the esophagus, the tube that goes from the throat to the stomach. Some people who have an esophagus ulcer experience nausea, vomiting, abdominal pain, or chest pain. The most common causes are gastroesophageal reflux disease , anti-inflammatory medications, smoking, herpes, and human papillomavirus.
Patients with an esophagus ulcer often experience recurring problems. Over time, these ulcers can cause the esophagus to narrow, causing painful and difficult swallowing. Barretts esophagus can develop in patients who have recurring ulcers in the esophagus caused by GERD. Barretts esophagus is a condition where the lining of the esophagus changes, causing chest pain, heartburn, bloody vomit, and difficulty swallowing.
Esophagus ulcers are usually diagnosed by x-ray after the patient drinks a barium solution that allows the doctor to see the outline of the digestive tract clearly. Endoscopes, flexible tubes with a camera and a light, can also be inserted into the throat to look for ulcers. Once a patient is diagnosed, a doctor may check for GERD. GERD patients usually have to take medications and control their diet to help relieve symptoms.
How Is A Peptic Ulcer Treated
Some peptic ulcers heal on their own. But if you donât treat them, the ulcers tend to come back.
They can erode the blood vessel wall in your stomach or small intestine. The ulcers also can eat a hole through the lining and get infected. Or they can cause swelling, which may block food from moving from your stomach into your small intestine.
If H. pylori is the culprit, your doctor may prescribe a mix of antibiotics to kill it. If aspirin and other NSAIDs are behind the ulcer, you may need to cut down on them, stop taking them altogether, or switch to another pain reliever.
Your doctor may also give you antacids to fight stomach acid, or prescribe medicine to lessen the acid your body makes. Prescription drugs called cytoprotective agents can help protect the lining of the stomach or small intestine so the ulcer can heal.
Read Also: How To Treat Leg Ulcers With Sugar
What Is The Best Diet For Barretts Esophagus
There isnt a specific diet for Barretts esophagus. If you have GERD or heartburn, consider making the following changes:
- Avoid eating large meals.
- Have dinner at least three hours before bedtime.
- Limit foods that trigger heartburn or GERD symptoms. Common problem foods include fried or fatty foods, chocolate, soda and tomato sauce.
A note from Cleveland Clinic
Being diagnosed with Barretts esophagus isnt cause for alarm. But it is good information to have. Consider the diagnosis extra motivation to get GERD symptoms under control. Also, keep your regularly scheduled endoscopy tests. These two things will ensure that youre doing everything you can to stay well.
Last reviewed by a Cleveland Clinic medical professional on 06/23/2020.
References
Rev Col Gastroenterol Vol30 No1 Bogot Jan/mar 2015
Management of a Bleeding Ulcer by Post-esophageal Ligation of Varices with Self Expanding metal Stents: Case Report and Literature Review
Department of Gastroenterology at the Fundación Santa Fe de Bogotá in Bogotá, Colombia.
General Surgery at the Universidad El Bosque in Bogotá, Colombia.
Received: 15-05-14 Accepted: 02-02-15
Abstract
Early treatment of bleeding varices with direct compression dates from the work by Westphal et al. in 1930. Later in 1950, Sengstaken-Blakemore developed their balloon which Panes and collaborators defined as the first line of therapy for esophageal varices in 1980 while they used the Linton-Nachlass balloon for gastric varices .
Keywords
Esophageal stent, refractory bleeding esophageal varices, ulcer.
INTRODUCTION
CASE REPORT
Upon admission, the patients hemoglobin level was 10.2 mg/dl. Treatment with terlipressin and ceftriaxone was started immediately. While still in the emergency room, the patient began to vomit a large amount of blood which led to hemodynamic instability due to hypotension and to difficulty breathing. Tracheal intubation was performed, three units of red blood cells were transfused, and norepinephrine was administered for vasopressor support.
DISCUSSION
Approximately 10% to 20% of patients with bleeding esophageal varices do not improve with standard therapy combining medication and endoscopic treatment and must undergo rescue therapies such as balloon tamponade or TIPS .
REFERENCES
You May Like: Best Bone Broth For Ulcerative Colitis
What Causes A Peptic Ulcer
Causes of peptic ulcers include
- long-term use of nonsteroidal anti-inflammatory drugs , such as aspirin and ibuprofen
- an infection with the bacteria Helicobacter pylori
- rare cancerous and noncancerous tumors in the stomach, duodenum, or pancreasknown as Zollinger-Ellison syndrome
Sometimes peptic ulcers are caused by both NSAIDs and H. pylori.
Recommended Reading: Normal Colon Vs Ulcerative Colitis
Stomach Ulcer Remedies: 10 Ways To Heal And Reduce Inflammation
An ulcer is a kind of erosion or open sore on the surface of an organ or tissue. Ulcers generally occur in the esophagus, stomach, and duodenum and are known as peptic ulcers.
Types of Peptic Ulcers
- Gastric ulcer: A peptic ulcer in the stomach is called a gastric ulcer.
- Duodenal ulcer: A duodenal ulcer is a type of peptic ulcer that develops in the first part of the small intestine .
- Esophageal ulcer: An esophageal ulcer develops in the lower part of the esophagus.
A peptic ulcer is among the most common forms of stomach disease. About 4 million Americans suffer from this condition every year.
Read Also: Compression For Venous Leg Ulcers
You May Like: Ulcerative Colitis How Much Blood Is Too Much
If I Have Barrett’s Esophagus How Often Should I Have An Endoscopy To Check For Dysplasia
The risk of esophageal cancer developing in patients with Barrett’s esophagus is quite low, approximately 0.5 percent per year . Therefore, the diagnosis of Barrett’s esophagus should not be a reason for alarm. It is, however, a reason to have periodic upper endoscopy examinations with biopsy of the Barrett’s tissue.
If you have Barrett’s esophagus and your first two upper endoscopy examinations with biopsies do not show dysplasia, then upper endoscopy with biopsy should be repeated about every three years. If your biopsy shows dysplasia, then your doctor will make further recommendations regarding the next steps.