Can Inflammatory Bowel Disease Be Fatal
Patients often ask if inflammatory bowel diseases can be fatal. This is really very unusual. Its true that the diseases can be serious ulcerative colitis can affect the whole of the colon, doesn’t always respond to medical treatment, and can need surgery. However, its extremely uncommon for it to be fatal, unless the disease is missed or not treated, or results in complications such as a perforation of the bowel. In this situation, an unpleasant and rather debilitating disease can turn into a dangerous and life-threatening one with peritonitis. This would then be a surgical emergency.
Crohns disease can affect any part of the digestive tract and can affect absorption of food and nutrients. In some unfortunate patients who have had Crohns in a very severe way affecting their small bowel, they can become nutritionally compromised and require intravenous feeding. There is a certain amount of mortality associated with this type of Crohns .
Can Inflammatory Bowel Disease Be Cured
Patients often ask me whether inflammatory bowel disease can be cured and the short answer is no. Interestingly, the cause of inflammatory bowel disease, while its not known, is a very active area of study and were finding out a lot about this quite quickly.
In brief, people have thought that Crohns disease is an autoimmune condition for very many years, but current research into genetics is giving us a lot of information that Crohns disease may, in fact, result from a failure of dealing with intestinal antigens and bacteria. We know that the bacteria in the gut are very relevant to the cause of Crohns. However, while this may lead to some more effective therapeutic innovations in the future, at the moment, we can’t say that we can cure Crohns disease.
Similarly, we cant cure colitis, although the mechanism of this is likely to be different. One day we may be able to cure these diseases, but at the moment, there is no definite cure for ulcerative colitis. However, we can induce prolonged periods of remission for years at a time, and help patients to manage their condition to improve their quality of life.
What Is The Treatment Of Ulcerative Colitis
The physician would do a complete physical assessment, and advise a series of blood and radiological investigations scan, etc.). Colonoscopy, endoscopy, biopsy, stool examination, and other tests would be required.
Ulcerative colitis is a lifelong disease with constant periods of flare-ups and remissions . Presently, there is no permanent medical cure for it, but there are various medications that can provide symptomatic relief, reduce inflammation, and manage flare-ups.
Treatment involves medical and surgical management, depending on the severity of the disease. Patients would also require dietary and lifestyle changes.
Medical treatment includes the following:
- Medication to suppress and/or modulate the immune system
Don’t Miss: Foods That Heal Stomach Ulcers
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Warning Signs Of Perforated Bowel And Hemorrhaging
A perforated bowel is a hole in the wall of the intestine which can occur as a consequence of toxic megacolon, but can also be caused by intestinal infections, and certain types of medication.
A full colonoscopyduring acute severe ulcerative colitis may also increase the risk of perforation, according to the January 2019 review in the BMJ Postgraduate Medical Journal.
This perforation is so dangerous because the contents of the intestine, which contain a large number of bacteria, can spill into the abdomen and cause a serious infection called peritonitis, notes the Crohn’s and Colitis Foundation.
Signs of bowel perforation include severe abdominal pain, a high fever, and heavy rectal bleeding or hemorrhaging. As a caregiver, look for, or ask about, sudden and dramatic increases in the amount of blood in your loved one’s stool.
If you suspect perforation, call 911 or go to the emergency room. Massive hemorrhaging in a patient with ulcerative colitis is an emergency condition that requires immediate medical attention and possibly surgical care to repair the hole in the colon wall.
RELATED: What Is Rectal Bleeding? Symptoms, Causes, Diagnosis, Treatment, and Prevention
Also Check: What Causes Ulcerative Colitis To Flare Up
Complications Outside The Bowel
Colitis doesnt just affect the bowel. As many as 1 in 5 people with Colitis develop problems in other parts of the body. Most affected are joints, eyes or skin. These are known as extraintestinal manifestations . They usually happen during a flare-up, but can occur without or before any bowel symptoms. These complications can often happen to people who dont have Colitis too. For many of the complications, there are things you can do to reduce your risk.
Joints
You may have pain and/or swelling in your joints. Around 1 in 6 people with Colitis experiences joint problems. For some, this will get worse during a flare, but will usually improve with treatment for Colitis. Others may have joint problems even when bowel symptoms feel better. Find out more in Joints.
Bones
People with Colitis are more at risk of developing thinner and weaker bones or osteoporosis. This can be due to ongoing inflammation, smoking, taking steroids or low levels of physical activity. Calcium is needed for bone formation, and this may be low if your diet doesnt contain enough dairy. Weight-bearing exercise, calcium and vitamin D supplements, not smoking and avoiding long-term steroid use can help. Some people may also take bisphosphonate medicines. Find out more in our information on Bones.
Skin
Colitis can affect the skin in different parts of the body.
Eyes
Anemia
Anaemia can make you feel very tired. If its more severe you may also have shortness of breath, headaches, and general weakness.
Liver
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Also Check: Best Treatment For Diabetic Foot Ulcer
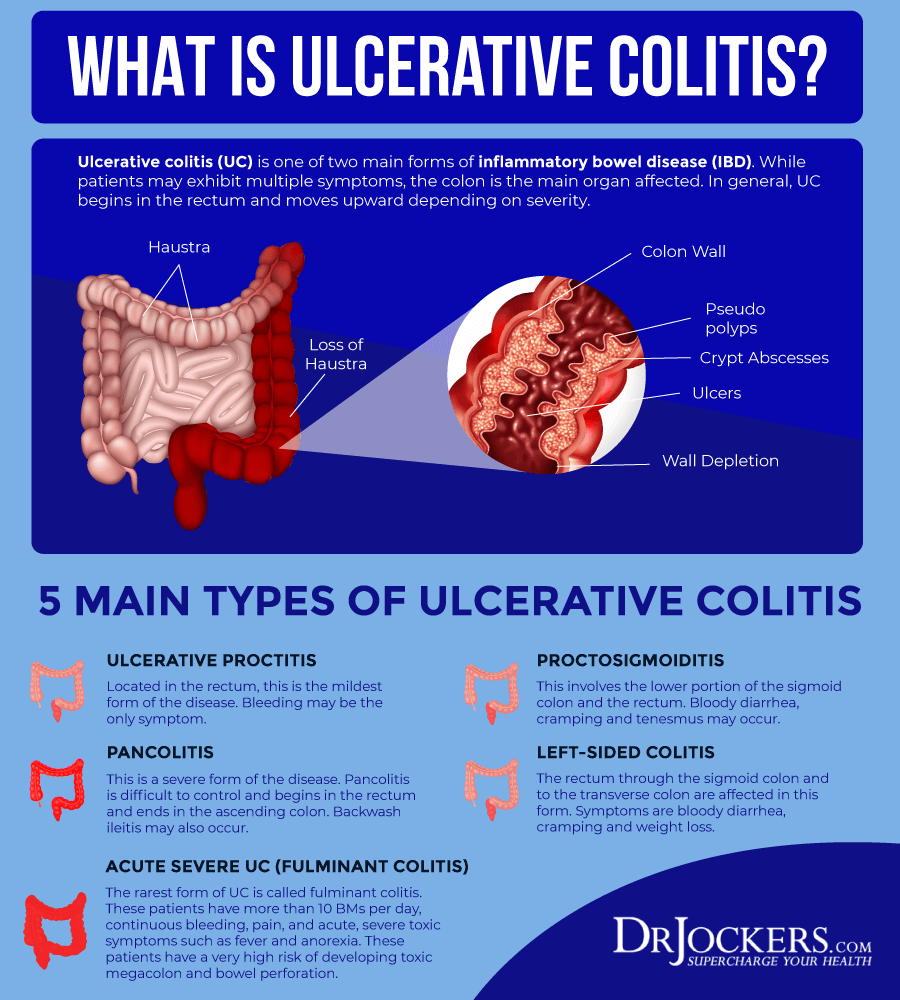
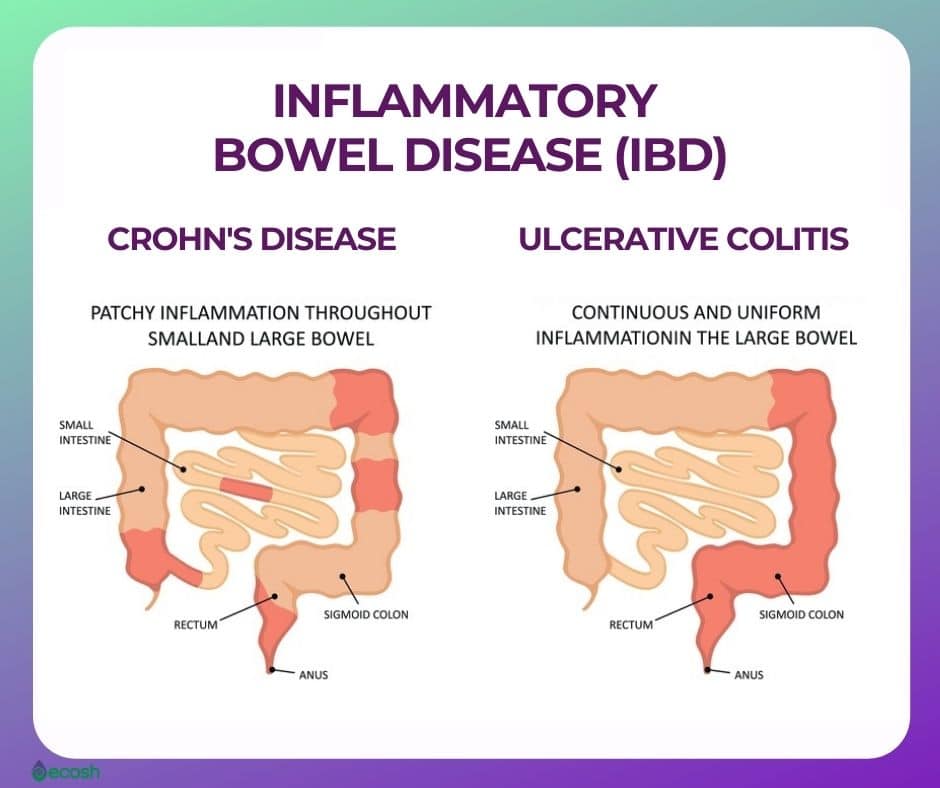
What Is Inflammatory Bowel Disease
We usually use it as a term to cover two diseases, firstly, ulcerative colitis, and secondly, Crohns disease, which can affect the body in similar ways.
Ulcerative colitis is an inflammatory disorder of the large bowel affecting the colon, which produces blood and diarrhoea. Thats what patients experience when they have flares of ulcerative colitis and it tends to proceed in a relapsing and remitting way patients can have long periods of remission, but then from time to time, they can have active flares.
Crohns disease is a different illness discovered by a New York physician called Burrill B. Crohn in the 1930s, which is characterized by inflammation . It classically tends to present with abdominal pain and diarrhoea rather than bleeding .
Is Ulcerative Colitis Serious
Unfortunately ulcerative colitis, or UC as its often referred to, does have the potential to be a serious illness due to some of the complications it can cause.
However, its important to remember that most people with ulcerative colitis dont experience some of the more serious complications that can occur due to receiving effective treatment. To help minimise your risk of complications you should follow the treatment prescribed by your doctor.
Some of the things that can cause serious complications include…
You May Like: How Do You Get Rid Of A Peptic Ulcer
The Signs And Symptoms Of Ulcerative Colitis
There are a number of different symptoms that can be associated with ulcerative colitis.
These can include:
In some cases, people may also experience:
- Eye inflammation
Ulcerative colitis can be a very debilitating condition, and it can cause a great deal of discomfort and inconvenience.
If you suspect that you may have ulcerative colitis, it is important to see a doctor so that you can get a proper diagnosis and treatment.
What Role Does Diet And Nutrition Play In Ulcerative Colitis
Diet does not cause the development of ulcerative colitis nor can any special diet cure the disease. However, the foods you or your child eat may play a role in managing symptoms and lengthening the time between flareups.
Some foods may make symptoms worse and should be avoided, especially during flareups. Foods that trigger symptoms are different from person to person. To narrow down what foods affect you, keep track of what you eat each day and how you feel afterward .
Problem foods often include:
- High sugar foods and drinks.
- Carbonated beverages.
- High-fiber foods.
In addition to the problem foods listed above, infants, children and teenagers can also experience issues with:
- Dairy products.
Keep a careful eye on your childs diet and nutrition. Their appetite may decrease during a flareup and they might not eat enough to stay healthy, and grow. Also, the inflammation caused by ulcerative colitis may keep their digestive tract from absorbing enough nutrients. This can also affect your childs health. For these reasons, you may have to increase the amount of calories your child consumes.
Its best to work with your provider and nutritionist to come up with a personalized diet plan if you or your child has ulcerative colitis.
Recommended Reading: Meals For People With Ulcers
What Are The Causes Of Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease affecting the inner lining of the large intestine leading to erosion and ulcers. It is a lifelong illness with no specific cause or cure. Patients have repeated cycles of flare-ups and remission with potential manifestations beyond the gut . There is a profound emotional and social impact on the affected patients.
What are the causes of ulcerative colitis?
The exact cause of ulcerative colitis is unknown, and the possible causes are as follows:
- Immune reactions
Stanford Scientists Link Ulcerative Colitis To Missing Gut Microbes
Bacteria normally inhabiting healthy peoples intestines and the anti-inflammatory metabolites these bacteria produce are depleted in ulcerative colitis patients, a Stanford study shows.
Aida Habtezion is the senior author of a study that describes how people with ulcerative colitis have insufficient amounts of a metabolite produced by a family of gut-dwelling bacteria.Steve Castillo
About 1 million people in the United States have ulcerative colitis, a serious disease of the colon that has no cure and whose cause is obscure. Now, a study by Stanford University School of Medicine investigators has tied the condition to a missing microbe.
The microbe makes metabolites that help keep the gut healthy.
This study helps us to better understand the disease, said Aida Habtezion, MD, associate professor of gastroenterology and hepatology. We hope it also leads to our being able to treat it with a naturally produced metabolite thats already present in high amounts in a healthy gut.
When the researchers compared two groups of patients one group with ulcerative colitis, the other group with a rare noninflammatory condition who had undergone an identical corrective surgical procedure, they discovered that a particular family of bacteria was depleted in patients with ulcerative colitis. These patients also were deficient in a set of anti-inflammatory substances that the bacteria make, the scientists report.
Read Also: Signs Of Ulcerative Colitis In Adults
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Complication : Blood Clots
Blood clotting after a cut is usually a good thing. But as UC progresses, patients enter a hypercoagulable state, meaning dangerous blood clots can form in the legs and lungs, says Dr. Hagan, perhaps due to dehydration, inflammation causing changes in the blood, and medication side effects. So, keep moving. Even if youre in a flare and feel crappy, take a walk, move around your home more, or try a few minutes on a stationary bike. Seek medical help if you notice swelling or pain in your calves, tightness in your chest, shortness of breath, or pain with deep breathing, she adds.
Also Check: Can Ulcerative Colitis Cause Chest Pain
You May Have An Increased Risk Of Osteoporosis
The reason undertreated and untreated ulcerative colitis can lead to osteoporosis is twofold, according to Bonthala. One is that active inflammation steals from the bones. Patients are in the bone-building phase of their life until their mid-30s, so if you have active inflammation, youre depleting nutrients from your bones, and youre not absorbing a lot of the nutrients your bones need, she explains.
The second reason: Flares that arise from poorly managed ulcerative colitis are often treated with steroids, which themselves can lead to osteoporosis. I get a lot of referrals for bone density tests in ulcerative colitis patients in their early 20s, she says.
How Do Doctors Treat Ulcerative Colitis
Doctors treat ulcerative colitis with medicines and surgery. Each person experiences ulcerative colitis differently, and doctors recommend treatments based on how severe ulcerative colitis is and how much of the large intestine is affected. Doctors most often treat severe and fulminant ulcerative colitis in a hospital.
Don’t Miss: How Dangerous Is Ulcerative Colitis
Emotional Impact Of Ulcerative Colitis
Living with a long-term condition that is as unpredictable and potentially debilitating as ulcerative colitis, particularly if it is severe, can have an emotional impact. In some cases anxiety and stress caused by ulcerative colitis can trigger depression.
You may find it useful to talk to others affected by ulcerative colitis, either face to face or via the internet.A good resource would be your local patient association. This website, operated by the UKs leading charity for people affected by ulcerative colitis, contains details of local support groups. The site also contains a large range of useful information on ulcerative colitis and related issues.
Living With Ulcerative Colitis
Ulcerative colitis, a disease that causes inflammation and sores in the digestive tract, affects everyone in a different way. About 10% of people get better after one attack, but it’s more likely that you’ll have flares that come and go throughout your life.
You may go weeks or years without any symptoms. That’s called remission. The longer you go without a flare, the better your overall health will be.
Your doctor will likely give you medicine to control inflammation and other symptoms.
If you don’t feel like your UC is under control, talk to your doctor. They may want to change your medicine dose or switch you to a different drug. If that doesn’t work, you may need surgery.
Read Also: What Foods Do You Eat When You Have An Ulcer
Physical Changes That Might Occur
Reduced absorptionThe reduced absorption of vitamins and some trace elements in patients with ulcerative colitis might result in symptoms such as:
- Night blindness,
- Hair loss, infertility ,
- Growth retardation and,
- Certain skin changesNot all patients have experience these physical changes.
ComplicationsFor example, a patient might encounter:
- Anaemia due to iron deficiency, loss of blood from the bowel, and/or by vitamin B12 mal-absorption
- Reduced uptake of bile acids in the small bowel and an increased absorption of bilirubin in the colon and have an increased risk of gallbladder stones
- Increased loss of water which may result in kidney stones
- Inflammation of the bile ducts this is known as primary sclerosing cholangitis and can cause symptoms such as itchy skin and tiredness
Serious complicationsThese can affect a few patients. Serious complications that have been reported are:
- Acute ballooning of the bowel due to gases becoming trapped inside the colon affecting approximately 1 in 20 persons with severe ulcerative colitis
- Perforation, the formation of a hole in the wall of the bowel
- Extensive haemorrhage
- Osteoporosis – affecting an estimated 1 in 6 people
Toxic megacolonToxic megacolon is a rare and serious complication that occurs in approximately 1 in 20 of cases of severe ulcerative colitis. In severe cases of inflammation, gases can get trapped in the colon, causing it to swell.
This is dangerous as it can:
The symptoms of a toxic megacolon include:
Complication : Toxic Megacolon
This complication is rareand as scary as it sounds. Toxic megacolon occurs when UC inflammation thats not well-controlled spreads deeper into the layers of the intestinal wall, causing the colon to expand and become severely distended, says Dr. Economou. A toxic megacolon stops working and, because you cant poop at all, gas and feces build up and can potentially rupture the colon, again releasing dangerous bacteria and fecal matter into your abdomen. Seek immediate medical help if over a short period you develop a painful, distended abdomen, fever, bloody diarrhea, and a rapid heart rate.
Also Check: Foam Dressings For Pressure Ulcer Prevention