Fmt Treatment For Ulcerative Colitis
Fmt treatment for ulcerative colitis
Fmt Treatment For Ulcerative Colitis. Donors are often selected from relatives, spouses, friends, or healthy volunteers. Fmt has gained acceptance as standard therapy for the treatment of rcdi with proven efficacy, safety and patient tolerability . Early studies utilizing fmt to treat ulcerative colitis show amelioration of symptoms as well as the possibility of sustained remission and even cure. Researchers believe that microbiome dysbiosis may play a large part in the symptoms of uc.
Is FMT Ready for IBD? AGA Journals Blog From journalsblog.gastro.org
Of the 20 patients enrolled in this study, 7 patients achieved a clinical response by week 4. 9 in a small trial of patients with ulcerative colitis and high antibody titres of fusobacterium species, the use of amoxicillin, metronidazole, and tetracycline led to. Objective we conducted this systematic review to assess the efficacy and safety of fmt in uc. Early pilot studies demonstrated a mixed result for the use of fmt in ibd. Significant microbial differences have been noted in the guts of those who suffer from ulcerative colitis. Fmt, or fecal microbiota transplantation, could be the therapeutic solution for patients with crohns disease or ulcerative colitis.
What Do You Mean By A Tailored Plan
Its our duty to ensure you receive the most precise strategy for your age, sex, and state of condition. Thats why we tailor each treatment plan to the individual through our online assessment, which is based on official disease indexes. This information helps us provide the most accurate and evidence-based plan for each individual.
Randomized Controlled Trials In Uc
Another recent study from Australia presented at this years European Crohns and Colitis Organisation conference took a novel approach to FMT preparation in their RCT of FMT in UC. They conducted a short duration, low intensity pooled faecal microbiota transplantation in patients with mild-moderately active ulcerative colitis with donor and autologous stool prepared in entirely anaerobic conditions. In remarkable results published as an abstract they showed that 12/38 achieved steroid-free remission in the active arm compared to 3/35 who received autologous FMT in the intention to treat analysis. Similarly clinical response and clinical remission rates were 55% vs. 20% and 50% vs. 17% , respectively. Whether this improvement in disease activity, that rivals results from biologic trials in UC, is due to viability of donor bacteria in anaerobically prepared conditions will hopefully be elucidated in the studys full publication.
Read Also: Prednisone Dosage For Ulcerative Colitis Flare Up
Donors Needed For Pioneering Faecal Microbiota Transplantation Service
With the faecal microbiota transplantation programme fully up and running following the COVID-19 pandemic, University Hospitals Birmingham is looking for new recruits to the donation programme.
FMT involves using gut bacteria from a healthy screened donor to effectively treat patients with recurring bowel infections, such as clostridioides difficile infection . CDI can cause symptoms such as severe diarrhoea, fever, stomach cramps, and can be life threatening.
FMT has been proven to be highly effective when treating patients with CDI, and is associated with higher cure and lower recurrence rates than antibiotics.
The FMT procedure involves transplantation of processed stool into a patients stomach or small bowel via a nasogastric tube, or PEG site or into their colon via a colonoscopy or an enema.
Set up in 2017, UHB provides the FMT service in partnership with The University of Birminghams Microbiome Treatment Centre .
Gastroenterologist Professor Tariq Iqbal, of University of Birmingham and UHB, said: The FMT service is a great success story for Birmingham, as the Microbiome Treatment Centre is unique in the UK, having helped many patients with ongoing severe bowel infection where antibiotics have become ineffective. The quality of life for these patients has been substantially improved, and the procedure can even save lives.
To register your interest or for further information about the donor recruitment and screening programme, please contact the MTC.
What Are The Anti
Curcumin has a wide range of potent anti-inflammatory effects through multiple mechanisms. It inhibits proliferation of pro-inflammatory T-cells and inhibits pro-inflammatory cytokines like TNF- and molecular cell factors such as NF-B. This directly relieves inflammation in the intestinal mucosa, allowing for complete mucosal healing.
Recommended Reading: Medications For Ulcers Over The Counter
What Should A Person Do After A Fecal Transplant Are There Any Particular Foods They Should Eat Or Avoid
Before a person undergoes a fecal transplant, their healthcare team will likely recommend that they use a bowel prep to mobilize the stool and try to empty the colon.
Post-fecal transplant protocols usually include an antidiarrheal regimen to allow for the uptake of the transplanted microbiota into the recipients colon.
There are no specific foods to avoid after a fecal transplant. However, the for people with UC is to eat a nutritious, well-balanced diet and minimize pro-inflammatory foods. These foods include animal and milk fats and protein, polyunsaturated fatty acids, and refined sugars.
Some examples of suitable diets to follow include:
- the specific carbohydrate diet
To date, researchers have studied fecal transplant in individuals who are younger, have relatively mild disease forms, and are already on stable dosages of medications.
Some unanswered questions that researchers are actively studying include:
- What is the optimal administration route?
- Can healthcare professionals reliably use fecal transplants without other treatments?
- How practical and sustainable is each treatment session?
With Multiple Microbiota Therapeutics In The Pipeline For Recurrent Clostridium Difficile Infection Clinicians Foresee A Shift In Treatment Options For The Condition
Shawna Williams
Learn about our editorial policies.
ABOVE: A fecal microbiota transplant capsule filled by staff at OpenBiomeCOURTESY OF OPENBIOME
Alexander Khoruts wishes wed all stop using the F-word. In addition to its yucky connotations, the term fecal transplant is an inaccurate description of the procedure he helped pioneer, he argues, since you cant transplant feces. Rather, its the intestinal microbiome that gets engrafted, says Khoruts, a gastroenterologist at the University of Minnesota who coauthored the first detailed how-to guide for the procedure. Accordingly, he says, he prefers the term intestinal microbiota transplant. As director of the universitys Microbiota Therapeutics Program, he regularly works with people who undergo the procedure, and Ive seen the patients really have a sigh of relief when you lose the fecal word.
Khoruts realizes that the term fecal microbiota transplant, or FMT, is likely here to stay, however. The procedure, which involves transferring carefully screened donor stool via colonoscopy, enema, or a pill, has gone mainstream over the past decade. FMT is now a go-to treatment for recurrent or refractory infections with a bacterium known as Clostridium difficile , which causes sometimes debilitating gastrointestinal symptoms and can be fatal if not successfully treated. Researchers are also investigating the efficacy of FMT for a range of other conditions.
Recommended Reading: Hand Foot And Mouth Ulcers
The Poo Panacea: Inside The Strange Surprising World Of Faecal Transplants
When treating antibiotic-resistant infections, injecting patients with other peoples excrement can be highly effective. Could it be the answer to dementia, anorexia and obesity too?
The man and woman are wearing blue hospital gowns and clear face shields. Dr James Sones and Dr Indu Srinivasan are in a room in the Division of Digestive Diseases at the University of Mississippi Medical Center in Jackson. They are about to create something that has spread through medicine like, well, a shitstorm.
Sones takes a brown gloopy material and spoons it into what looks like a regular kitchen blender. The camera zooms in to a label on it: faecal blender. The brown gloopy stuff is, depending on your profession and level of politeness, faecal matter, stool, excrement or poo. It has been donated by a generous volunteer and it is almost certainly going to transform the life of the person who is going to receive it.
Once blended and mixed with saline, the brown stuff is poured into large syringes and infused into a willing patient by colonoscopy. In the UK, this treatment is available for patients suffering from repeated infections of Clostridium difficileor C diff.
Human waste is a misnomer. What we excrete contains nutrients and bacteria, and it can be a useful fertiliser or fuel. That the bacteria it contains can also cure ailing guts was known by ancient Chinese writers, who wrote of yellow soup , which was used to treat food poisoning and bad diarrhoea.
How Does It Work
The process starts with the careful selection of a healthy donor. All donors need to undergo thorough and regular medical examinations that include testing for a wide variety of conditions, including infectious diseases such as HIV and hepatitis. During this process the medical history and predispositions of the donors are also assessed and donors with an increased risk of developing certain conditions arent eligible to donate stool.
All donors need to follow lifestyle and diet recommendations, which ensures that their intestinal ecosystem is at an optimal, balanced level. To make sure thats really the case, all donors also undergo microbiome testing, which analyses parameters such as the composition and diversity of their intestinal flora. Finally, the stool is checked to rule out the presence of parasites and pathogens. Only stool that meets all these strict parameters and contains a balanced and varied intestinal flora is used for further processing.
Unlike some other FMT providers, we do not use whole, unprocessed stool. Instead, donated stool is filtered under special anaerobic conditions to remove all waste material such as digested food residues, mucus, dead cells, hormones etc. At the end of this process were left with liquid implants that contain only gut microbiota, which significantly reduces the potential health risks and side effects of FMT.
Recommended Reading: Foods For People With Ulcerative Colitis
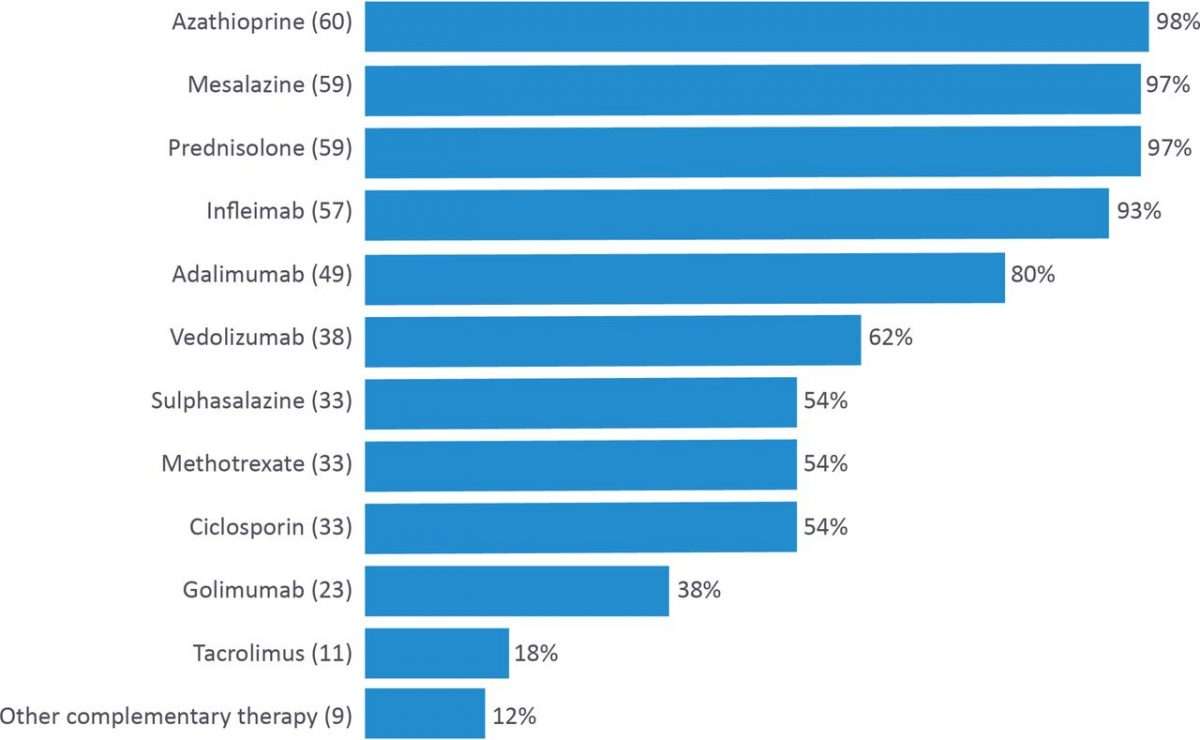
Common Uc Treatment And Surgery Options
Ulcerative Colitis treatment depends on the severity of each case. Cases are generally managed with different medications and some people find diets and natural remedies for Ulcerative Colitis effective. Though diets and medication can help manage UC, many people will continue to have bad or worsening symptoms.
For those who continue to have severe symptoms despite the use of medication, surgery is an option. Partial or full removal of the colon is possible . In a colectomy, the colon is removed and replaced by a medical bag that acts as a transplant colon. The bag is left outside the body at first, but may be put inside at a later time if the patient recovers well.
These common treatments for UC are unsatisfactory for many, as is allowing your illness to progress to the point of needing a colectomy. Thankfully, alternative new treatments for UC are being explored, and one of the more promising ones include FMT. The possibility of FMT and continued focus on treating the microbiome could one day mean the end of the invasive surgeries that are currently common practice for treating Ulcerative Colitis.
Icipant Rights And Confidentiality
The chief investigator will be the custodian of the data. Information with regards to study participants will be kept confidential and managed in accordance with the Data Protection Act, National Health Service Caldicott Guardian, The Research Governance Framework for Health and Social Care and Research Ethics Committee Approval.
There will be no patient identifiable data on the CRF and a unique participant number will be allocated. The principal investigator will hold the key to the coded number of the participants only. Only the principal investigator will have access to the patient identifiable information.
Don’t Miss: Wound Vac For Pressure Ulcers
You Dont Have To Just Take Our Word For It Heres What Our Own Patients Have To Say After They Took That Brave First Step And Started Their Journey With Us
Weve spent years with our patients, been with them through the highs and lows, and watched many of them grow up into healthy adults with full lives. Its thanks to their courage and partnership that we could develop our integrative strategy, launch our clinical trials and share our findings with the world.
Patient And Public Involvement
Patients with UC were surveyed during the trial design stage to ascertain willingness to participate in the trial as described. All seven patients approached indicated by return of questionnaire their willingness to be recruited into the trial.
The investigators will invite IBD-specific charitable organisations and their patient representatives to help disseminate the findings of the feasibility trial and to design phase III.
Don’t Miss: How To Test For Ulcerative Colitis
Baseline Patients And Healthy Donors Characteristics
Patients and healthy donors baseline characteristics,including sex, age, height, weight, history of taking medicine before FMT for inflammatory bowel diseases, course of the disease, levels of inflammatory markers , colonic mucosal score, and Mayo score before FMT, are listed in Table .
Table 3 Basic patient and healthy donors information ± SD)
Fmt For Ulcerative Colitis And Crohns Disease
Since the late 80s FMT trials have been carried out on patients with ulcerative colitis. In 1989 55 patients with various gastrointestinal disorders were given faecal microbiota transplants and a follow up of six patients in 2003 who had UC showed there was no clinical, colonoscopic or histologic evidence of UC in any patient2.
A review published in August 20183 of the FMT trials to date said: Clinical trials data are still poor but strongly support a future introduction of FMT in therapy to manage IBD microbiome. More studies are needed to assess the optimal route of administration and the frequency of FMT, the best matched donor for each patient as well as the risks associated with FMT in IBD.
Much of the evidence for FMT use to treat inflammatory bowel disease appears to be for ulcerative colitis, rather than Crohns disease.
In an interview in Gastroenterology & Hepatology in May 2018 Dr Paul Moayyedi said: A small amount of observational case-series data, as well as several randomized, controlled trials , suggest that FMT may work in the setting of ulcerative colitis. There is less evidence that FMT works in patients with Crohns disease, but the same principle applies.4
At the moment FMT for IBD isn’t widely available.
Also Check: How To Treat Mouth Ulcers
The Gut Microbiota In Ibd
It has long been thought that the gut microbiota is likely to be key to the pathogenesis of IBD. Early investigators considered Crohns disease to be variant of Johnes disease, which is caused by Mycobacterium paratuberculosis and affects cattle. Indeed 30 years ago Mycobacterium avium paratuberculosis was isolated from the intestine of patients with Crohns disease and this was considered by many to be pathogenic. More recent careful review of the evidence suggests that it is simply a bystander and does not fulfil Kochs classical postulates. Patients with CD have been shown to respond well to antibiotics such as ciprofloxacin and rifaximin. Additionally UC often starts after an episode of infective gastroenteritis and it has been previously shown that infection with Campylobacter and non-typhoid Salmonella increases the risk of developing IBD. Using germ-free animal models predisposed to IBD it has been repeatedly shown that in the absence of gut microbiota, IBD does not develop.,, Furthermore, diverting the faecal stream in human patients with severe colonic Crohns disease has long been known to have a healing effect, with restoration of bowel continuity resulting in recurrent inflammation. The accepted position and much repeated mantra is no microbiota no IBD.
Can I Take Curcmin With My Current Treatment Or Medication
Yes! Its very safe when taken in combination with other medications. In fact, some studies show that gut-directed curcumin can enhance the efficacy of first-line medications through synergistic effects. Curcumin in particular has been found to enhance efficacy of 5-ASA and improve loss of response to medications such as Remicade.
In general, its best to continue your medications unless instructed otherwise by your doctor.
Read Also: Extra Virgin Olive Oil And Ulcerative Colitis
These Are Their Stories:
Suzy
I am completely blown away by my results! Evinature helped improved my quality of life. I am forever grateful and astonished at my results!
Sonya
A month in, I felt better. At two months, my blood tests were great, and at six months, I entered clinical and endoscopic remission. Now I rely solely on herbal treatment.
Almog
I was completely shocked that a plant had much stronger effects than very high dosages of steroids and very powerful medications. I started feeling much better!
Bosmat
The treatment exceeded all my expectations. I went back to living fully. And all this without any conventional medicine. Today, a year later, Im still in remission.
Shahar
It helped within 48 hours to subdue my flare up. Took about 2 more weeks to have complete remission. Treated with this for the last 7 years with great success.
Yael
On Sunday I started your natural treatment. On Monday morning, the bleeding stopped and everything looked normal. It acted like magic. Thank you!
Tomer
It allowed me to return to my normal activities. I gained weight, was more productive with my job, no longer depressed because my symptoms were down. I really recommend it, its really helpful.
Tamar
The change started from the first week. I recommend anyone with colitis to try it. I returned to function normally, and returned to the mother my children had known.
Tal
Bat-El
Hadar
Leah
Noa
Inon
Could You Have Ulcerative Colitis
Ulcerative colitis is an autoimmune condition, which means the immune system malfunctions and starts to attack healthy tissue. Scientists are unsure of the cause but many think it is a combination of genetic and environmental factors. The immune system appears to mistake harmless bacteria in the colon for pathogens and begin attacking the tissues of the colon, causing pain and inflammation.
There is no cure for ulcerative colitis so the aim is to relieve symptoms during flare-ups and prevent them from returning. Current treatments include
- aminosalicylates
- corticosteroids
- immunosuppressants
If you have been diagnosed with ulcerative colitis or have symptoms that may indicate you have the condition, talk to us.
We can arrange a diagnosis if necessary and talk to you about the range of options available to manage the symptoms.
Don’t Miss: How To Treat Leg Ulcers With Sugar