What Is A Flare
When you have ulcerative colitis, your physician will try to find the right medications to control your symptoms. However, since there is no cure, the systemic disease is always there. When the symptoms arent present, you are in remission. If the symptoms return, especially if they are worse than before, it is a flare. This is why it is important to continue taking any medications your doctor prescribes, even if you feel better. If you stop taking your medication, then you can increase your chance of experiencing a flare and progression of the disease. Infections, stress, and taking antibiotics or NSAIDs can also make you more susceptible to a flare.
Read Also: Can You Take Imodium With Ulcerative Colitis
Heart Palpitations And Ibd Treatments
Some IBD treatments may cause palpitations. For example, corticosteroids can cause heart rhythm changes and other side effects. Medications that suppress the immune system like azathioprine can also affect heart rhythms, although this is unusual. If you notice palpitations after trying a new treatment plan, talk to your doctor to see if one of your medications may be a cause.
I had heart palpitations on prednisone. It is disconcerting, said one member. Another member ran into the same issue with one of their meds. I had to stop the azathioprine after two weeks. I was having joint pain, nausea, and palpitations, they remarked.
Some other health conditions or medications unrelated to Crohns disease or ulcerative colitis may cause palpitations. Additionally, many times doctors dont know what causes a persons heart rhythm to change.
Articles On Ulcerative Colitis Overview
Ulcerative colitis affects your colon, which is part of your digestive system. A lot of things can cause trouble in that general area, so how do you know what it feels like to have ulcerative colitis?
It depends on how severe it is, and on what part of your colon is affected.
Also, symptoms can come and go. You might not have any for weeks, months, or even years, and then they come back. Chances are about 50-50 that the effects will be mild.
Still, most people with the disease have a few common issues:
Recommended Reading: Foam Dressing For Pressure Ulcer
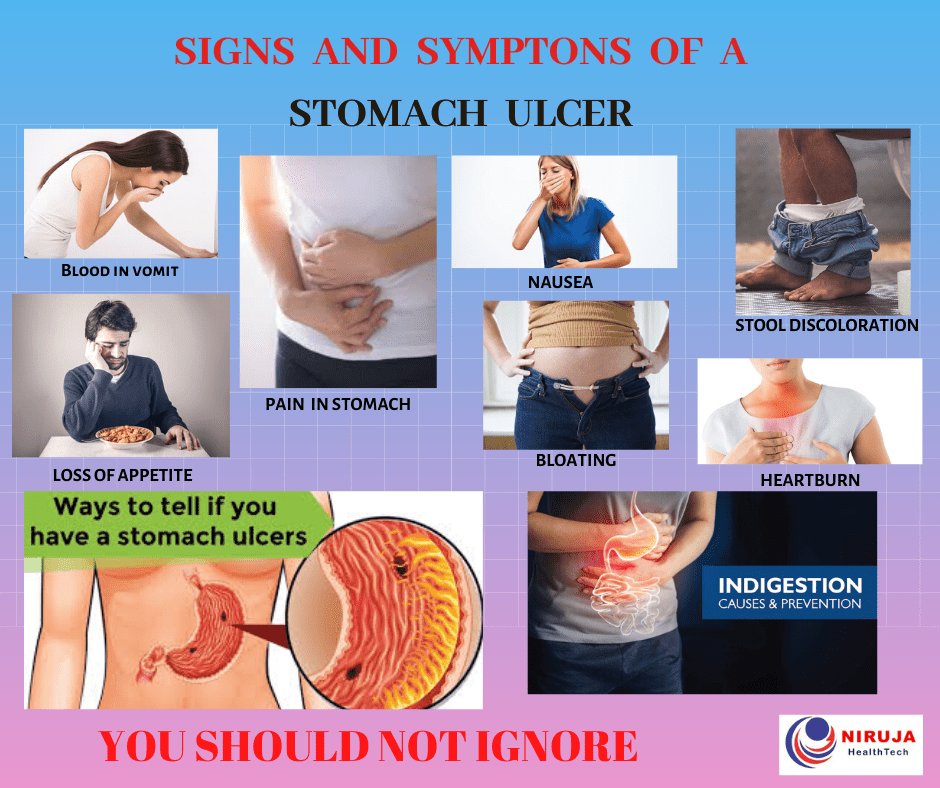
Outlook For Peptic Ulcers
With proper treatment, most peptic ulcers heal. However, you may not heal if you stop taking your medication early or continue to use tobacco, alcohol, and nonsteroidal pain relievers during treatment. Your doctor will schedule a follow-up appointment after your initial treatment to evaluate your recovery.
Some ulcers, called refractory ulcers, dont heal with treatment. If your ulcer doesnt heal with the initial treatment, this can indicate:
- an excessive production of stomach acid
- presence of bacteria other than H. pylori in the stomach
- another disease, such as stomach cancer or Crohns disease
Your doctor may offer a different method of treatment or run additional tests to rule out stomach cancer and other gastrointestinal diseases.
How Uc Affects The Entire Body
Medically reviewed by Matthew J. Hamilton, MD
Ulcerative colitis is a type of inflammatory bowel disease, or IBD, that causes chronic inflammation in the large intestine. This can lead to gastrointestinal symptoms ranging from abdominal pain and cramping to frequent bowel movements.
However, inflammation and associated symptoms can go beyond your gutits estimated that up to 40 percent of people with IBD experience one or more non-GI symptoms.
Ulcerative colitis can be more systemic in the way it affects the body, explains David T. Rubin, MD, professor of medicine and chief of gastroenterology at the University of Chicago, and chair-elect of the national scientific advisory committee for the Crohns and Colitis Foundation. Meaning, ulcerative colitis can affect the entire body. Find out what you should watch for, plus ways to take control of your health.
Read Also: How To Treat Pressure Ulcers On Buttocks
Don’t Miss: Diet For Venous Leg Ulcers
Ankylosing Spondylitis And Ulcerative Colitis
When bone fusion occurs, axial spondyloarthritis progresses into ankylosing spondylitis. AS is a specific type of axial arthritis that causes inflammatory back pain and limits range of motion. If a person has AS that causes significant fusing in their vertebral column and affects their rib movement, they may also struggle to take deep breaths.
According to the University of Washington, ankylosing spondylitis symptoms generally dont present alongside gastrointestinal symptoms in people with UC. Although doctors arent entirely sure what causes AS, some research suggests a genetic component contributes to the diseases development. Bowel or urinary tract infections are also believed to trigger the onset of AS in genetically susceptible people.
Treating Back Pain In Ulcerative Colitis
Treating back pain in ulcerative colitis can be complicated. Research shows that treating the underlying UC can help lessen the severity of spondyloarthritis, but it will not resolve spondyloarthritis and back pain. Back pain must be addressed separately and in a way that does not make a persons UC symptoms worse.
People with ulcerative colitis may need to work with both a rheumatologist and a gastroenterologist to manage their gastrointestinal and spinal health properly. These doctors may prescribe or recommend the following treatments and therapies.
Also Check: Xeljanz Vs Entyvio For Ulcerative Colitis
Ulcerative Colitis And Joint Pain
When you have ulcerative colitis , its normal to have pain in your abdomen, along with diarrhea and other gastrointestinal symptoms.
Up to 30 percent of people with UC also have arthritis, which is characterized by swollen, painful joints.
Heres a look at the connection between UC and joint pain, as well as what you can do to protect your joints if you have UC.
Joint Pain: The Most Common Non
About 30 percent of people with ulcerative colitis experience joint pain, according to the Crohns and Colitis Foundation, making it the most common non-GI symptom of the disease. Joint pain often occurs in the knees, ankles, elbows, and wrists. Its usually joint pain thats symmetrical, meaning both knees or both ankles, says Dr. Rubin. This type of joint pain tends to parallel bowel activityso if you fix the intestine, the joint pain goes away.
However, ulcerative colitis is also related to inflammatory joint conditions that affect your spine, like ankylosing spondylitis. This type of joint pain can be independent of your bowelso your bowel can be completely in remission, and your back or your pelvis is inflamed, and you can have joint damage, says Rubin.
The good news: Some medications used to treat ulcerative colitis are also used to treat inflammatory joint conditions like ankylosing spondylitis. Its not that fixing the bowel makes these joints betterits that the medication that works on the bowel also works on these joint conditions, says Rubin. So if youre experiencing joint pain, its important to work with your doctor to understand what type of joint pain you have and get proper treatment. In some cases it may be necessary to see a doctor who specializes in the joints, a rheumatologist, to work with your IBD doctor.
Read Also: What To Do When Ulcerative Colitis Flares
Reducing Your Arthritis Risk When You Have Ulcerative Colitis
Arthritis is the most common complication outside the gut for people with ulcerative colitis. These dos and donts will help you protect your joints.
As if gut pain from ulcerative colitis werent enough, as many as 30 percent of people with an inflammatory bowel disease , including ulcerative colitis, will develop problems with their joints, according to the Crohns and Colitis Foundation. Indeed, arthritis is the most common complication that occurs beyond the intestines.
Although its not fully understood, there seems to be a link between the gut and joints, says Harry D. Fischer, MD, the chief of rheumatology at Lenox Hill Hospital in New York City. For example, a bacterial infection in the digestive tract can cause a reactive type of arthritis, he notes. In addition, both arthritis and ulcerative colitis have a genetic component.
According to the Crohns and Colitis Foundation, people with ulcerative colitis tend to have one of three forms of arthritis:
- Peripheral arthritis , which affects large joints such as the knees, ankles, elbows, or wrists when IBD is properly treated and controlled, PA joint pain and symptoms typically improve
- Axial arthritis, which causes pain and stiffness in the spine and lower back
- Ankylosing spondylitis, a more severe type of arthritis that affects the spine and can lead to joint damage. Its an uncommon complication that affects between 2 and 3 percent of people with IBD.
Whats The Connection Between Ibd And Joint Pain
IBD and inflammatory arthritis are both thought to be autoimmune conditions, in which the bodys immune system mistakenly mounts an attack on its own healthy tissues. Its common for two or more autoimmune diseases to occur at the same time. For instance, rheumatoid arthritis is a typical comorbidity for people with IBD. Other types of arthritis, such as enteropathic spondylitis, are also associated with gastrointestinal disease.
Read Also: Tnf Alpha Inhibitors For Ulcerative Colitis
Recommended Reading: Best Treatment For Stage 3 Pressure Ulcer
Talk With Others Who Understand
MyCrohnsAndColitisTeam is a social network and online support group for people with IBD and their loved ones. Here, over 163,000 members come together to ask questions, offer advice and support, and share stories with others who understand life with IBD.
Have you experienced chest pain with Crohns disease? What was the cause, and how did you manage it? Share your experiences and tips in the comments below, or start a conversation by posting on your Activities page.
What Tests Diagnose A Peptic Ulcer
To confirm a person has an ulcer a diagnostic imaging test will usually be ordered. The two most widely used tests are:
- Upper GI series : This is a type of X-ray. The patient is given a chalky liquid to drink that increases the contrast on the X-ray, making certain features easier to see. Because this liquid contains barium, this test is sometimes called a barium swallow.
- Endoscopy : An endoscope is a thin, flexible tube with a tiny camera at the end. The patient is given a mild sedative, and then the tube is passed through the mouth into the stomach. The doctor can see the lining of the stomach to diagnose a peptic ulcer. Tiny samples of the tissue will be taken , which are examined under a microscope.
If a diagnostic imaging test reveals an ulcer, the patient will most likely have a test to see if H pylori bacteria are present.
- It is important to be certain about this, because treatment of the H pylori is likely to heal the ulcer.
- Ulcers caused by H pylori are treated differently than ulcers caused by medications.
Three types of tests are available to detect H pylori.
Also Check: Where Does It Hurt When You Have An Ulcer
What Kind Of Doctor Treats Peptic Ulcers
- If you suspect you may have a peptic ulcer, you may first be diagnosed by your family practitioner or internist.
- Children or teenagers may see a pediatrician.
- For further treatment you will likely be referred to a gastroenterologist, a specialist in disorders of the digestive tract.
- If you have an emergency such as vomiting or severe abdominal pain you will be seen by an emergency medicine specialist in an emergency room.
- In the rare case where surgery is needed, you may see a general surgeon.
How Does Ibd Affect Other Parts Of The Body
IBD can also cause problems outside the gut. Some people with IBD develop conditions affecting the joints, eyes or skin. These can be known as extraintestinal manifestations and often occur during active disease, but they can develop before any signs of bowel disease or during times of remission. Many of these are not very common.
JOINTS
Inflammation of the joints, often known as arthritis, is a common complication of IBD.
It is most common in those with Crohns Colitis and also affects about one out of 10 people with UC.
The inflammation usually affects the large joints of the arms and legs, including the elbows, wrists, knees and ankles. Fluid collects in the joint space, causing painful swelling, although pain may occur without obvious swelling. Symptoms usually improve with treatment of intestinal symptoms, and there is generally no lasting damage to the joints. A few people develop swelling and pain in the smaller joints of the hands or feet. This may be longer lasting and persist even when the IBD is in remission.
Sometimes, the joints in the spine and pelvis become inflamed a condition called ankylosing spondylitis . This can flare-up independently of IBD. It often causes pain over the sacroiliac joints, on either side of the lower part of the spine. Stiffness and pain in the spine itself may eventually lead to loss of flexibility.
SKIN
Some complications are related to the liver and its function.
BLOOD CIRCULATION
ANEMIA
You May Like: What Causes Ulcers On Your Feet
Health Conditions That Alter Heart Rhythms
Other conditions that can cause heart palpitations include:
- Hormone changes due to menstruation or menopause
- Thyroid problems
- Abnormally high or low levels of certain minerals, such as potassium
- Low blood sugar levels
Some MyCrohnsAndColitisTeam members have posted about having palpitations linked to these causes. If you experience ongoing palpitations, talk to your doctor and mention any other symptoms you might be experiencing. Discuss any supplements you are thinking about taking with your regular doctor or gastroenterologist . Some vitamins and supplements can actually lead to changes in your heart rhythm.
Perforation Of The Colon
Long-term inflammation and ulcers in the colon can weaken the intestinal wall. Over time, these weaknesses may develop into a perforation.
A perforation can allow bacteria and other intestinal contents to leak out into the abdomen, causing a serious condition called peritonitis.
Peritonitis is the inflammation of the peritoneum, which is the lining of the abdomen. This condition may cause the abdomen to fill with fluid. It can also lead to blood poisoning and sepsis, which is a whole-body inflammatory response to infection.
One in three people who develop sepsis die from the condition.
Symptoms
It is vital to know the symptoms of a perforated colon to help prevent peritonitis and sepsis. According to the , these may include:
- severe stomach pain
A perforated colon is a medical emergency that usually requires surgery to repair the hole in the intestines.
People who experience sepsis also require urgent treatment with antibiotics and fluids.
You May Like: What Foods To Eat If You Have A Stomach Ulcer
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
When To Seek Medical Attention
When pain is a part of your normal day-to-day life, it can be easy to minimize it. Pain can often be an indication of disease progression or a flare-up. When the pain is accompanied by other symptoms, it may be a sign of something serious. If youre ever unsure about the pain youre experiencing, ask your doctor.
Seek medical advice and inform your gastroenterologist if:
- Your pain worsens or suddenly becomes severe, occurs in a new area, or is noticeably different in any way
- You have persistent, abnormal bowel movements or notice blood in your stool in addition to your GI pain
- You experience nausea, vomiting, or fever
- You have joint pain in the back or hips, especially if the joint pain is accompanied by severe morning stiffness
There are several ways to help alleviate pain under the ribs thats associated with IBD.
You May Like: Wound Care For Stage 1 Pressure Ulcer
What Treatments Are There For Ulcers
Your treatment will depend on the cause of your ulcer. For example, if our tests indicate that an infection caused by helicobacter pylori is what created your ulcer, well give you antibiotics to eliminate the bacteria.
Regardless of the cause, medications that help reduce the level of acid in your stomach can help the ulcer heal. And different lifestyle changes can accelerate healing as well, such as eliminating certain foods, abstaining from alcohol, and practicing stress management.
In severe cases, surgery may be required. Your provider at Prima Medicine will work with you to create a treatment plan for your situation.
If you have a stomach ulcer or want to see if you do, we can help. To learn more, book an appointment online or over the phone with Prima Medicine today.
You Might Also Enjoyâ¦
Symptoms Of Ulcerative Colitis

The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to empty your bowels frequently
You may also experience extreme tiredness , loss of appetite and weight loss.
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is.
For some people, the condition has a significant impact on their everyday lives.
Also Check: What Do You Eat If You Have A Stomach Ulcer
Pulmonary Hypertension And Ulcerative Colitis
Pulmonary Hypertension is a rare but severe condition that causes high blood pressure in the lungs by damaging the pulmonary arteries. The vessels transport blood from the heart to the lungs, but because of the disease they become narrow and thick. When the normal blood flow becomes compromised, the heart is forced to work under stress to pump blood, which makes the heart weak and enlarged. There are numerous risks associated with this condition, including right heart failure and death.
When the cause of a specific case of pulmonary hypertension is unknown, the condition is known as idiopathic. When the disease is caused by a primary medical condition, it is called associated pulmonary hypertension. Common primary diseases include lung and heart diseases but inflammatory bowel disease ulcerative colitis which affects the digestive track, can also be a cause.