Whole Grain Breads Cereals And Pastas
Whole grain flour is high in fiber because it hasnt had the germ or bran removed.
Its important to avoid eating food made from any whole grain flour, such as:
, including beans, lentils, and peas, are high fiber, high protein foods. Because of the indigestible sugars in beans, theyre also notorious for causing gas. If you are experiencing a UC flare-up, youll want to pass on the following:
- all beans, including chickpeas
- soy nuts, including soybeans and edamame
Food Preparation And Meal Planning
While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
What Foods Should I Exclude While I Am Having A Flare
Although excluding certain foods whilst flaring can improve symptoms it is important to ensure you still maintain a balanced diet and replace any excluded food groups with suitable alternatives. Fibre is the only generally recommended food exclusion during a flare.
Fibre: Skins, seeds, and pith of fruits, vegetables, legumes and grains.
Excluding fibre during a flare is recommended to reduce symptoms such as diarrhoea, bloating, abdominal pain and bleeding. This is only a short term dietary change which should be changed once symptoms have resolved. Examples of high fibre foods include: beans, legumes, onions, peppers, broccoli, cauliflower, peas, sweetcorn, wholegrain breads, pastas and rice, raw/dried fruits and vegetables.
Dairy and gluten are also commonly excluded foods by those with ulcerative colitis. It is not generally recommended to exclude these foods unless you have a diagnosis of lactose intolerance or coeliac disease.
Dairy: Milk, cheese, yoghurt
Dairy foods can sometimes cause symptoms and are sometimes excluded. It is important to remember to replace excluded dairy produce with suitable fortified alternatives as they are a good source of calcium. Examples of non-dairy calcium containing foods include soya milk and yoghurt, breads, sardines, spinach, baked beans, orange, figs and orange juice.
Gluten: Bread, pasta, pastries and biscuits
Also Check: Foam Dressings For Treating Pressure Ulcers
Dietary Fat Intake As A Risk Factor For Ibd
There have been conflicting data on the association between dietary fat intake and the development of IBD, as many of the studies are retrospective and use small sample sizes. However, a very large, long-term, prospective study completed over 26 years did not observe a significant association with increased risk of developing CD or UC with total dietary fat intake, saturated fatty acids and monounsaturated fatty acids , which has been well supported by other research studies . A growing body of scientific evidence indicates that the Mediterranean diet pattern has been associated with significant improvements in health status and decreases in inflammatory markers in humans . The protective effect is hypothesized to be derived from the balance in fats, which includes incorporating MUFA, SFA and fish intake . While a few studies do show that MUFAs are beneficial during colitis, studies on the effects of SFA and PUFAs on gut health are controversial.
The Nurses Health Study cohorts reported high, long-term intake of trans-unsaturated fatty acids was associated with a trend towards an increased incidence of UC but not CD . An increased relative risk of developing IBD has also been associated with frequent intake of fast foods . The relative risk associated with the consumption of fast foods at least two times a week was estimated at 3.4 for CD and 3.9 for UC . Frequent fast food intake, defined as more than once a week, was significantly associated with a risk of UC and CD .
Best Foods For Ulcerative Colitis Patients
Ulcerative colitis is a health condition that is highly influenced by the diet of a person. Knowing which foods to eat can help avoid flares and make your symptoms better. Also, some foods can help avoid a ulcerative colitis flare. Here, we have mentioned a few food items that you can consider eating if you have this condition.
Here are the best foods for ulcerative colitis patients.
1. Refined GrainsPatients suffering from ulcerative colitis usually find it hard to digest whole grains. Hence, switching to cereal, bread, and pasta made from refined grains. You can also opt for bland items like cooked white rice if it is difficult to consume most foods.
2. ProbioticsYogurt is a good choice to add to your daily diet if you are suffering from ulcerative colitis. It contains live bacteria known as probiotics that help in digestion. Regular consumption of probiotics can reduce the symptoms and flares of ulcerative colitis. You can also choose probiotic supplements if you are lactose intolerant or do not prefer eating yogurt.
3. ApplesauceThis is one of the best foods for ulcerative colitis. However, try to avoid its consumption during a flare. Applesauce is soft, easily digestible, and a good source of nutrients. Make sure to choose unsweetened versions as the excess sugar can result in inflammation. It can be made at home by peeling and slicing up apples, cooking it in some water, and making a puree out of the mixture.
Dont Miss: Will Ulcers Cause Blood In Stool
Recommended Reading: Can I Eat Oatmeal With Ulcerative Colitis
What To Eat During Remission
Increase fiber and reintroduce whole grains — Slowly incorporate foods higher in fiber when gastrointestinal symptoms lessen.
Consume omega-3 fatty acids — Consider eating more fresh or canned fatty fish or taking a fish or flaxseed oil supplement.
Focus on wholesome foods in their natural state — This includes foods with minimal processing and minimum ingredients.
Dairy and lactose products will be better tolerated — If you have a lactose intolerance, avoid dairy or eat low-lactose or lactose-free products.
Added fats will be better tolerated — Continue to focus on using oils, such as olive oil or canola oil, instead of solid fats.
Continue to focus on protein foods — Consume beef, eggs, poultry and other lean meats or plant-based proteins, such as soy products.
Be sure to drink plenty of water — Drink water instead of fruit juices, soft drinks, alcohol and caffeinated beverages such as coffee or tea.
Can You Eat White Bread With Ulcerative Colitis
Low-residue diet
Temporarily eating a low-residue or low-fibre diet can sometimes help improve symptoms of ulcerative colitis during a flare-up. These diets are designed to reduce the amount and frequency of the stools you pass. Examples of foods that can be eaten as part of a low-residue diet include: white bread.
Dont Miss: Is Ulcerative Colitis An Inflammatory Bowel Disease
Don’t Miss: Do Stomach Ulcers Cause Gas
How To Calculate The Pucai Score
The PUCAI score ranges from 0 to 85 and is defined as:
- Remission : less than 10
- Predict the course of the disease over time
- Know when to recommend other treatments in severe cases
Experts recommend that doctors check a childâs PUCAI score during every visit and reevaluate treatment if their score is above 10.
You May Like: What Foods Are Good To Eat With Ulcerative Colitis
Vitamin And Mineral Supplementation
Nutritional supplements are great for patients with inflammatory bowel disease who may need a bit of extra help preventing a nutritional deficiency.
Your healthcare providers may also recommend a vitamin and/or mineral supplementation plan if your tests show you already have a nutritional deficiency.
You may be able to get all your necessary vitamins and minerals from eating a well-balanced, nutrient-rich diet. But flares, severe symptoms, surgeries, and other complications may make it difficult for some patients with Crohns disease or ulcerative colitis to get enough nutrients from food alone.
Check with your doctor or other healthcare providers before taking any supplements, including over-the-counter medications, herbs, and other complementary therapies.
-
Some supplements can cause gastrointestinal symptoms, including nausea and diarrhea.
-
Check the labels on your supplements for lactose, artificial colors, sugar alcohols, or preservatives, all which can aggravate your IBD, especially when you are in a flare.
-
Most supplements should not be taken on an empty stomach.
Video Length00:02:00
Vitamin and Mineral Supplementation in IBD Often times, when you have Crohn’s disease or ulcerative colitis, you may need to take vitamins or minerals to prevent or make up for a nutritional deficiency. Watch and listen this video to learn more about common vitamin and mineral supplements for IBD patients.
Read Also: How Do You Treat An Ulcer Naturally
Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
Nutritional Optimisation Before And/or After Surgery
Having good nutritional status before undergoing surgery is important to encourage good surgical outcomes, such as a short hospital stay, fast recovery of bowel function and reducing risk of post-surgical complications. Often, medical nutrition drinks are recommended for 7-10 days leading up to planned surgery to optimise nutritional status to improve surgical outcomes. In people with Crohns disease, a period of EEN before planned surgery may also be recommended to both improve nutrition and reduce active disease. This may be used in preference to corticosteroids.
After surgery, your surgeon will gradually allow you to restart oral intake. Some patients may have narrowing at the join of the bowel due to swelling, and require a short-term low fibre diet to allow the site to heal and bowel movements to start. Your surgeon and dietitian will guide the degree and timeframe for fibre restriction, if needed.
Please refer to the Surgery for IBD page for further information.
Also Check: Colon Cleanse For Ulcerative Colitis
Can Certain Foods Really Cause Inflammation
The link between what we eat and chronic inflammation in the body isnt fully understood. What is known is that there does seem to be some connection.
Lets jump into the science: The liver produces something called C-reactive protein as a response to inflammation in the body. In short, higher levels of CRP mean more inflammation, and certain foods have been shown to increase levels of CRP in the blood.
Now, the specifics of what foods cause this increase is somewhat up for debate, but its possible that things like processed sugar can trigger the release of inflammatory messengerslike CRPa sign that they may potentially be contributing to an inflammatory state.
On the other hand, foods like fruits and vegetables may help fight oxidative stress, which is a trigger for inflammation. Certain diets, like the Mediterranean diet, already include many foods that are considered to be anti-inflammatory such as whole grains, legumes, a rainbow assortment of fruits and vegetables, and fish.
How I Began My Journey Healing With Herbs
From age 11 to 20, I took various forms of medications and bled off and on. I remember being 14 and leaving class for the bathroom at least 6 times a day. One day, the bleeding intensified. My mom saw my pale face and brought me to the ER. This type of bleeding continued sporadically throughout my teens.
I finally gained some stability around age 18. My GI prescribed me an immunosuppressant that is often used in chemotherapy. I took the pills and they worked. They worked better than anything I had taken previously. But I couldnt stop getting infections. The first year I took them, I got an upper respiratory tract infection and coughed up blood. In the following years, I kept getting strep throat and horrible cases of the flu.
I was also old enough to do my own research. The side effects of the immunosuppressors alarmed me and included a dangerous form of lymphoma, bone loss, and possible liver damage.
After 3 years, a great surge of clarity and courage reminded me of how urgent it was to stop taking the immunosuppressant and begin healing with herbs and other holistic protocols. At age 21, I stopped taking medications for the first time in 10 years and began a journey healing with herbs and diet. I was no longer willing to harm the rest of my body with the medications in order to protect a single area: my colon.
Here are a few key things I realized during my transition to holistic healing:
Read Also: Is Ulcerative Colitis A Gastrointestinal Disease
What Can I Eat During Remission
When your UC is in remission, your instinct might be to reach for foods that are normally off-limits during a flare. But its still best to stick with generally trigger-free fare.
I would advise someone to eat plenty of diverse vegetables and fruits and consider following an anti-inflammatory style diet or Mediterranean diet, says Dr. Singh.
Though, fiber, in its many forms, may be better tolerated during remission, says Freuman. Go for the raw veggies, eat the salad, have a handful of whole nuts, or leave the skin on your fruits and vegetables, she says.
That said, Freuman adds that some people find that these types of foods bother them even in remission, and thats perfectly okay. Its not worth suffering or making yourself sick to push beyond the comfortable limits of tolerance, notes Freuman.
Ultimately, she encourages her clients to eat the greatest variety of plant-based foods they can comfortably tolerate as the foundation of their diets.
Read Also: Is Oatmeal Good For Ulcerative Colitis
Diet For People With A Stoma
Most people with a stoma have an acceptable output and do not need to modify their diet. Generally, the Australian Guide to Healthy Eating is recommended. One of the roles of the large intestine is to reabsorb water, so ensuring good hydration by having plenty of fluid is important. You may benefit from further consultation with a specialist dietitian if your stoma output is too much, too watery, or too gassy.
Please refer to the Complications with IBD page for further information.
You May Like: Can You Get Ulcers In Your Colon
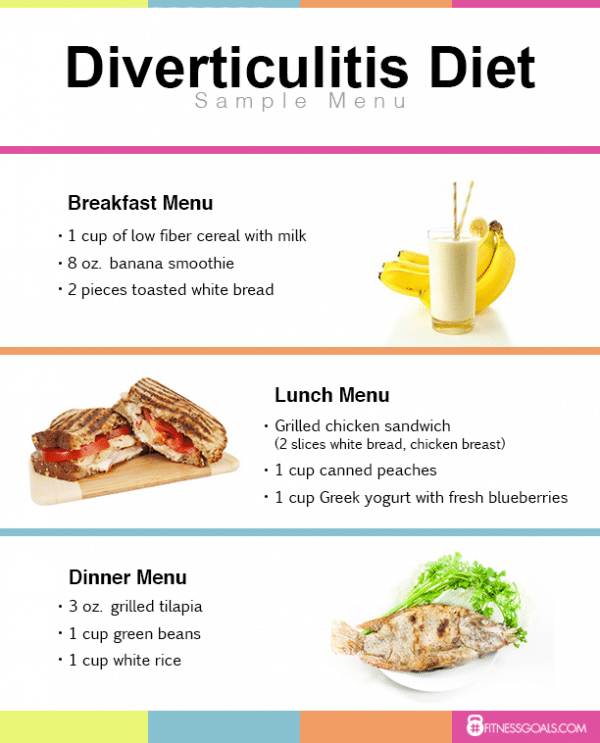
Ulcerative Colitis Diet: What To Eat In A Flare Up
A low residue diet is often recommended to manage symptoms of ulcerative colitis. The Canadian Society of Intestinal Research outlines residue as the solid contents that stay in the bowel after digestion, with the goal of reducing the number of bowel movements that happen in a day. Residue includes fiber, which is limited to 10-15g per day, but the low residue diet differs from the low fiber diet by including foods that may stimulate frequent bowel movement, such as dairy, caffeine, alcohol and gristly or fatty meat.
Dr Deborah Lee, of Dr Fox Online Pharmacy, recommends the following foods for a low residue diet:
- Low fiber fruit and veg such as melon and bananas, as well as stewed fruit
- Lean protein such as white meat, eggs and tofu
- Refined grains such as white bread, white pasta and oatmeal
- Cooked seedless and skinless vegetables such as cucumber, potato and squash.
Cooking your food may also break down some of the dietary fiber to make it more digestible, as seen in a study in the journal of Plant Foods for Human Nutrition , which indicates that the process of cooking decreases the amount of insoluble dietary fiber in some vegetables.
- Related: 4 dairy free diet benefits
Keeping A Food Journal
Everyones body is different, so its possible for two people who have UC to have different trigger foods.
Logging what you eat throughout the day and when digestive issues occur can help you and your doctor narrow down your personal food triggers.
A food journal can be especially helpful if youre trying a new diet.
Don’t Miss: Over The Counter Medicine For Ulcerative Colitis
Supplements And Other Lifestyle Changes To Try
Besides diet and medicine, there are a few other therapies that could be helpful for people with ulcerative colitis.
Dr. Singh suggests focusing on adequate sleep and reducing stress to prevent flares. One of the most common causes of flare can be stress, so stress reduction is probably the best medicine I talk about when I see patients, he says.
There is also limited research surrounding the use of certain supplements and probiotics as a therapy for IBD, but more evidence is needed before recommendations are made12,13.
Ulcerative Colitis Diet: Food Preparation And Meal Planning
While the idea of an elimination diet or restricting your intake of fiber, fat or other trigger foods may seem daunting, meal planning and preparing your food ahead of time can take some of the stress out of eating in a flare up. If your appetite is impacted as well, you can batch cook and eat what you want of a larger pre-prepared meal when you feel like eating, rather than preparing yourself a whole new meal from scratch.
The Crohns and Colitis Foundation indicates that rates of depression and anxiety are higher in those with IBD, so anything that can reduce stress for those with ulcerative colitis might be helpful for managing mental health. As such, pre-planned meals based around particular dietary needs can make the day-to-day experience of ulcerative colitis slightly less stressful, and may make the experience of a flare up more bearable.
This article is for informational purposes only and is not meant to offer medical advice.
Also Check: What Causes Ulcers In Your Stomach