How Can People With Ibd Manage Their Pain
The first step in developing a pain management approach for a patient with IBD is to determine what is causing the pain. If active IBD is causing the pain, then the first strategy is generally for healthcare providers to change or increase the medication that the patient is taking to manage the disease, such as aminosalicylates, corticosteroids, antibiotics, immunosupressants, or biologics. In many cases, treating the disease and its symptoms can be effective in reducing pain.1
However, some people may continue to experience pain despite the change in medication, or they may have pain that is not due to active IBD but some other cause. In those cases, healthcare providers may recommend trying some kind of pain relievers.
What Are The Treatment Options For A Flare
When you first develop ulcerative colitis it is usual to take medication for a few weeks until symptoms clear. A course of medication is then usually taken each time symptoms flare up. The medicine advised may depend on the severity of the symptoms and the main site of the inflammation in the colon and the rectum .
Topical treatments applied locally by an enema or suppository are widely used for treating ulcerative colitis, particularly aminosalicylate and steroid medicines – see below. They are a treatment option if ulcerative colitis affects only the lower part of the bowel .
Medication options include the following:
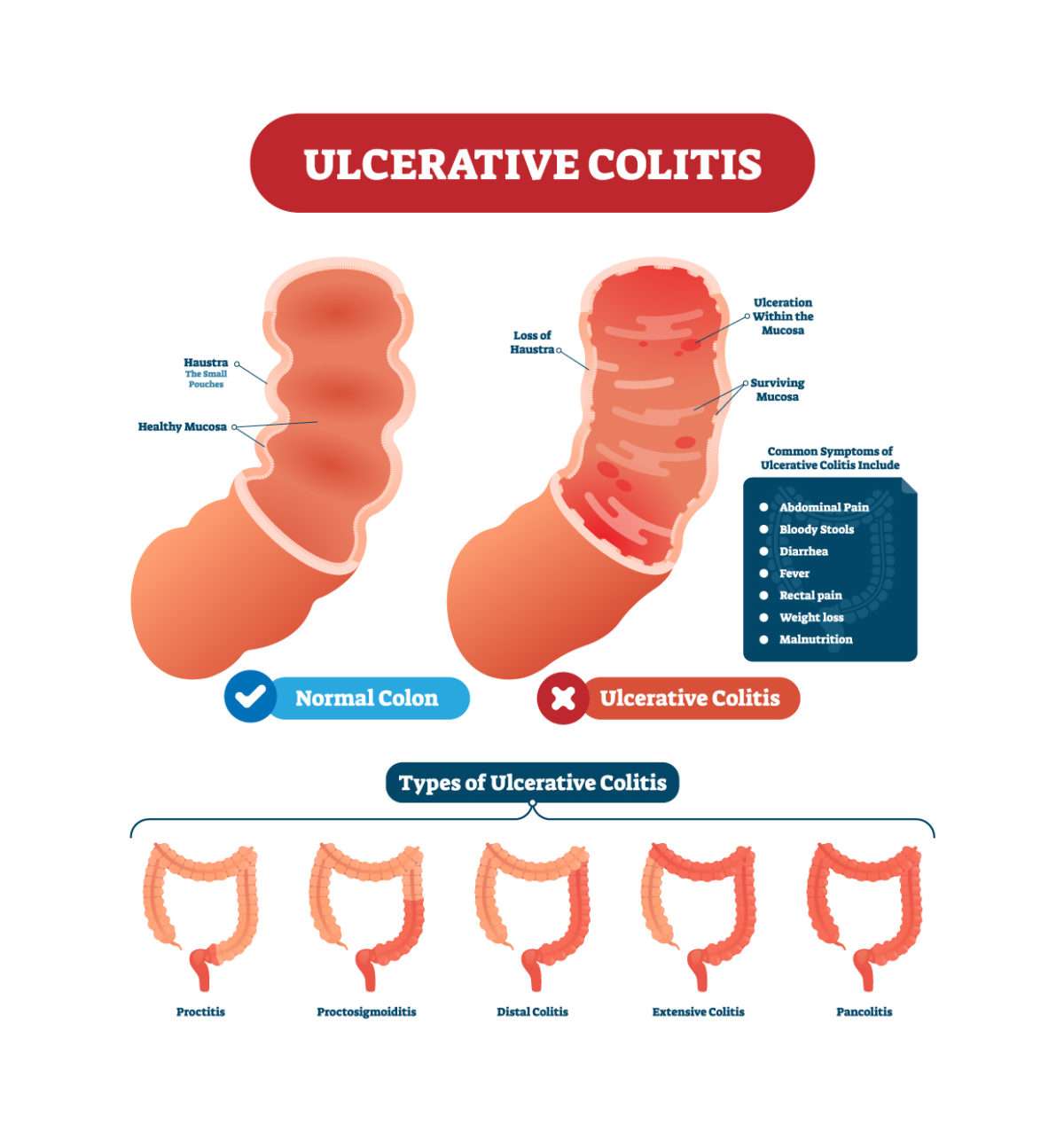
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Recommended Reading: Can Ibuprofen Help Ulcerative Colitis
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
What To Look For
The key is to pay attention to your specific symptoms. The more youre aware of them, the better able you are to spot changes.
And there are lots of ways your symptoms can change. You might get new ones. Or the ones you have may get worse, last longer, or come on more often.
Usually, a flare-up brings at least:
- An urgent need to poop
- Blood or mucus in your stool
- Cramps in your lower belly
If it spreads to more areas of the colon, everything gets more intense. You have more diarrhea. Cramps get more severe. You have more mucus, pus, and blood in your stool. Pain in your belly gets worse and more widespread, especially up the left side. It can also affect your desire to eat and cause you to lose weight.
And some of those symptoms may just be signs of a stronger flare-up. Youll need to see your doctor to find out for sure. Read more on ulcerative colitis symptoms to look for.
You May Like: What Helps With Ulcerative Colitis Pain
What Is The Outlook
With modern medical and surgical treatment, there is just a slight increase in the risk of death in the first two years after diagnosis, compared with the general population. After this there is little difference in life expectancy from that of the general population. However, a severe flare-up of ulcerative colitis is still a potentially life-threatening illness and needs expert medical attention.
As mentioned, if you do not take medication to prevent flare-ups, about half of people with ulcerative colitis have a relapse on average once a year. This is much reduced by taking regular medication. However, even in those who take regular medication, some people have frequent flare-ups and about a quarter of people with ulcerative colitis eventually have an operation to remove their colon.
A year from diagnosis, about 9 in 10 people with ulcerative colitis are fully capable of work. So, this means that, in the majority of cases, with the help of treatment, the disease is manageable enough to maintain a near-normal life. However, the condition can cause significant employment problems for a minority.
Treatment for ulcerative colitis is an evolving field. Various new medicines are under investigation. These may change the treatment options over the next ten years or so and improve the outlook .
Daily Life For People With Ibd
People with IBD lead useful and productive lives, even though they need to take medications. When they are not experiencing a flare-up of their disease, they feel quite well and are often free of symptoms.People with IBD can marry, enjoy sexual activity and have children. They can hold down jobs, care for families and enjoy sport and recreational activities.Even though there is currently no cure for IBD, medical therapy has improved the health and quality of life of most people with Crohns disease and ulcerative colitis. Research underway today may lead to further improvements in medical and surgical treatment, and even a cure.
Recommended Reading: Ulcerative Colitis Shortness Of Breath
Ulcerative Colitis In Children
According to one study of IBD in the United States, 1 in 1,299 children between ages 2 and 17 years old were affected by the condition in 2016. Crohns disease was twice as common as UC, and boys were more likely to have IBD than girls.
For children with IBD, a diagnosis is more likely after 10 years old.
UC symptoms in children are similar to symptoms in older individuals. Children may experience bloody diarrhea, abdominal pain and cramping, and fatigue.
In addition, they may experience issues compounded by the condition, such as:
- anemia due to blood loss
- malnutrition from poor eating
- unexplained weight loss
UC can have a significant effect on a childs life, especially if the condition isnt treated and managed properly. Treatments for children are more limited because of possible complications. For example, medicated enemas are rarely used as a treatment method in children.
However, children with UC may be prescribed medications that reduce inflammation and prevent immune system attacks on the colon. For some children, surgery may be necessary to manage symptoms.
If your child has been diagnosed with UC, its important that you work closely with their doctor to find treatments and lifestyle changes that can help. Check out these tips for parents and children dealing with UC.
What Should I Ask My Doctor On Behalf Of My Child Or Teenager
Ask your healthcare provider the following questions in addition to the ones listed above:
- What vitamins should my child take?
- Will my other children have pediatric ulcerative colitis?
- Is my child at risk for other conditions?
- Can you recommend a psychiatrist or therapist to help my child with emotional issues related to pediatric ulcerative colitis?
- Is my child growing at a normal rate?
- What can I do to help my child cope at school?
A note from Cleveland Clinic
When you have ulcerative colitis, its essential to work closely with your healthcare team.
Take your medications as prescribed, even when you dont have symptoms. Skipping medications youre supposed to take can lead to flareups and make the disease harder to control. Your best shot at managing ulcerative colitis is to follow your treatment plan and talk to your healthcare provider regularly.
Recommended Reading: Ulcerative Colitis And Back Pain
How Can I Help My Child Live With Ulcerative Colitis
Children with this condition need long-term care. Your child may have times when symptoms go away . This can sometimes last for months or years. But symptoms usually come back.
Your child should learn what foods trigger his or her symptoms and avoid these foods. You and your childs healthcare provider should make sure your child gets enough nutrients to grow and develop well. Support groups can help you and your child. Work with your childs healthcare provider to create a care plan for your child.
Symptoms Of Ulcerative Proctitis
The presenting symptoms of ulcerative proctitis all relate to the rectum. Blood in the stool occurs in almost everyone with the disease. Diarrhea is a common symptom, although constipation can also develop as the body struggles to maintain normal bowel function.
Inflammation of the rectum may cause a sense of urgency to have a bowel movement, discomfort after having a bowel movement, and a sensation of incomplete emptying of the bowels. Systemic symptoms such as fever, tiredness, nausea, and weight loss are rare.
Ulcerative proctitis has very few complications but with increased irritation to the anal and rectal area, hemorrhoids may occur. Only rarely do other complications occur, such as abscesses and extra-intestinal manifestations. Individuals with ulcerative proctitis are not at any greater risk for developing colorectal cancer than those without the disease.
Dont Miss: Can I Take Imodium If I Have Ulcerative Colitis
Recommended Reading: Diet When You Have An Ulcer
Living With Ulcerative Colitis
Ulcerative colitis, a disease that causes inflammation and sores in the digestive tract, affects everyone in a different way. About 10% of people get better after one attack, but it’s more likely that you’ll have flares that come and go throughout your life.
You may go weeks or years without any symptoms. That’s called remission. The longer you go without a flare, the better your overall health will be.
Your doctor will likely give you medicine to control inflammation and other symptoms.
If you don’t feel like your UC is under control, talk to your doctor. They may want to change your medicine dose or switch you to a different drug. If that doesn’t work, you may need surgery.
Treatments For Ulcerative Colitis
Treatments for ulcerative colitis wont cure the condition, but it can help to regulate the immune system and manage symptoms. Patients may use one type of treatment or a combination of them depending on their unique condition.
Certain medications can treat inflammation and symptoms such as diarrhea, bleeding, and abdominal pain. Medication may also be prescribed to lower the frequency of flare-ups. Alongside medication, it can be helpful for patients to alter their diet and nutrition.
Experts have found that certain foods can aggravate symptoms in UC patients. This includes spicy, high-fibers, or dairy foods. Instead, eating a healthy diet that involves softer and blander food can cause less discomfort.
In some cases, medicine and diet changes arent enough to treat UC. Surgery may be required to remove the colon and rectum completely with the creation of an ileostomy or external stoma. The type of surgical procedure for UC will greatly depend on the patients age, overall health, and symptoms.
Recommended Reading: Do You Still Have Ulcerative Colitis After Colectomy
Who Develops Ulcerative Colitis
About 2 in 1,000 people in the UK develop ulcerative colitis. It can develop at any age but most commonly first develops between the ages of 10 and 40. About 1 in 7 cases first develop in people over the age of 60 years. Non-smokers are more likely than smokers to develop ulcerative colitis. However, smoking brings other dangers to health which far outweigh this benefit.
Ibd And Changing Your Diet
Some dietary changes that may help a person with IBD include:
- Low-fibre diet when IBD is active, most people find a bland , low-fibre diet helps to ease diarrhoea and abdominal cramping. People with Crohns disease who have a narrowed small intestine may need to eat a low-fibre diet most of the time.
- Low-fat diet people with Crohns disease who experience steatorrhoea may benefit from a low-fat diet.
- Low-lactose diet the milk sugar lactose is broken down by the enzyme lactase, commonly found in the lining of the small intestine. Some people with Crohns disease lack this enzyme, so should avoid milk and other dairy products. Lactose intolerance can be diagnosed with a simple test ask your doctor.
- Liquid diet a person with severe Crohns disease may need a nutritionally balanced liquid diet.
- Plenty of water people with IBD need to drink plenty of fluids to prevent dehydration.
Recommended Reading: Foods To Avoid If You Have A Stomach Ulcer
Ulcerative Colitis And Cancer Of The Colon
The chance of developing cancer of the large intestine is higher than average in people who have had ulcerative colitis for several years or more. It is more of a risk if you have frequent flare-ups affecting the whole of the large intestine. For example, about 1 in 10 people who have ulcerative colitis for 20 years which affects much of their large intestine will develop cancer.
Because of this risk, people with ulcerative colitis are usually advised to have their large intestine routinely checked after having had the condition for about 10 years. This involves a look into the large intestine by a flexible telescope every now and then and taking small samples of bowel for examination. It is usually combined with chromoscopy – this is the use of dye spray which shows up suspicious changes more easily. Depending on the findings of this test and on other factors, you will be put into a low, intermediate or high risk category. ‘Other factors’ include:
- The amount of intestine affected.
- Whether you have had complications such as polyps. These are small, non-cancerous growths on the inside lining of the colon or rectum.
- Whether you have a family history of cancer.
The National Institute for Health and Care Excellence recommends the next colonoscopy/chromoscopy should depend on the degree of risk of developing colon or rectal cancer. After the next test, your risk will be calculated again.
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Don’t Miss: Can Ulcerative Colitis Cause Low Testosterone
How Are Causes And Risk Factors The Same And Different
Doctors arenât sure what causes you to get UC or diverticulitis, but the two conditions have some common risk factors:
- Age. Your odds for either condition go up as you get older.
- Race. White people are more likely than those of any other race to have UC or diverticulitis.
UC might be caused by an abnormal immune response in your body. This means that if your immune system is fighting off a virus or bacteria, it may mistakenly attack cells in your digestive tract, too.
Genes might also play a role. If a close relative like your parent or sibling has UC, youâre more likely to have it, too. If you’re of Ashkenazi Jewish descent , your risk is even higher. Diet and stress donât cause UC, but they may trigger your symptoms and cause flare-ups.
As for what causes diverticulitis, experts believe bacteria found in your poop might get pushed into the bulging sacs as it passes through the colon. This causes the sacs to become infected or inflamed. Another theory is that your poop, especially if youâre constipated, might put a lot of pressure against the colon walls as it passes through. This can cause tears in the sacs and increase your chances of an infection.
Other risk factors for diverticulitis include:
- Diet low in fiber and high in animal fat
- Certain medications
How Is Acute Severe Ulcerative Colitis Treated
ASUC is a challenging condition to treat. Once youre admitted to the emergency room, youll get a series of tests, including blood tests, stool tests, and an exam of your bowel called a sigmoidoscopy. Youll also get intravenous fluids to boost hydration.
The average hospital stay for ASUC treatment ranges from 4.6 to 12.5 days. During this time, your health care providers may include a gastroenterologist, colorectal surgeon, dietitian, pharmacist, and stomal therapist. The goal of hospitalizing you is to end the flare, get your symptoms under control, and put the disease into remission. Your doctors will want to make sure that rectal bleeding and diarrhea have stopped and normal bowel movements have returned. Rehospitalization is common.
Intravenous steroid medications are the most common treatment for ASUC. For 30% to 40% of ASUC patients, steroid treatments donât work â and taking steroid medications for more than 10 days increases your risk of complications.
If the steroids donât help within 3 to 5 days, your health care team will start âmedical rescue therapyâ with immunosuppressive drugs like cyclosporine or infliximab.
You might get an operation to remove part of your colon, called a colectomy, if your ASUC doesnât respond to steroids, immunosuppressants, or other medical treatments.
Read Also: Can Ulcerative Colitis Cause Body Aches
Read Also: How To Prevent A Pressure Ulcer
What Causes Ulcerative Colitis Plus How To Treat It
- Ulcerative colitis is a type of inflammatory bowel disease that develops when your colon or rectum become inflamed.
- UC affects about 900,000 individuals in the U.S.
- The exact cause of ulcerative colitis is complex but experts believe it could be caused by an overactive immune system.
- Even though there is no cure, there are treatment options available that can help you manage the disease.
Do you need to take frequent trips to the bathroom? Perhaps youre suddenly feeling overly tired every day or experiencing unusual abdominal pain or cramping. If thats the case, you might be suffering from a type of inflammatory bowel disease known as ulcerative colitis.
Related Topics :
Roughly 900,000 individuals are living with ulcerative colitis in the United States. And while it often develops between the ages of 15 and 30, anyone can develop it at any age. Theres a lot more to know about it too. So, lets take a look at what ulcerative colitis is, what causes it, the signs to look out for, plus how to treat it.
You May Like: Psc Liver Disease Ulcerative Colitis