Colectomy Linked To Increased Risk For Gallstone Disease In Uc
We were unable to process your request. Please try again later. If you continue to have this issue please contact .
Patients with ulcerative colitis may have an increased risk for gallstone disease after undergoing colectomy, according to the results of a Danish national cohort study.
This finding led researchers to call for further studies to identify high-risk patients to minimize the negative effects of gallstones after colectomy.
For years, we have known that a colectomy induces changes to the composition of bile, but it has been unclear whether these changes are reflected in a greater risk of gallstone disease,Anders Mark-Christensen, MD, of the department of surgery, section of coloproctology, Aarhus University Hospital, Denmark, told Healio Gastroenterology. We found that individuals with ulcerative colitis who had a colectomy had a 63% higher risk of being hospitalized for gallstone disease compared to those with ulcerative colitis without colectomy.
Anders Mark-Christensen
Sensitivity analyses showed the adjusted HR for cholecystectomy after colectomy was 1.55 .
Getting The Right Diagnosis
Your doctor will ask about the type and timing of your symptoms. Theyâll probably feel your belly to see if itâs tender. Let them know about any medications that you take and if anyone in your family has ever had IBD or other digestive issues.
Everything you tell your doctor gives them clues about other tests you might need, such as:
Stool samples and bloodwork. Your poop and blood can reveal signs of infection or inflammation. Blood tests can also show low levels of iron. Thatâs called anemia. It can happen when colitis causes a lot of bleeding in your colon.
Imaging. Your doctor may take pictures inside your colon or rectum. They might use a special liquid called barium for some tests. Thatâs a substance thatâll coat your colon to help it show up better on X-rays.
You may also need:
- Magnetic resonance imaging scans
- Computed tomography scans
Endoscopic tests. An endoscope is a camera attached to a thin, bendy tube. Your doctor can use it to look at your lower colon and rectum or entire colon .
Tissue biopsy. Your doctor may remove some tissue during a colonoscopy or sigmoidoscopy. A lab technician will use a microscope to check for signs of inflammation or other abnormal cells.
What You Can Do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there’s anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you’re experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, vitamins or supplements that you’re taking. Be sure to let your doctor know if you’re taking any herbal preparations, as well.
- Ask a family member or friend to come with you. Sometimes it can be difficult to remember all the information provided to you during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your doctor.
Your time with your doctor is limited, so preparing a list of questions ahead of time can help you make the most of your time. List your questions from most important to least important in case time runs out. For ulcerative colitis, some basic questions to ask your doctor include:
Read Also: Ulcerative Colitis What Vitamins Can I Take
When To Contact A Medical Professional
Contact your provider if:
- You develop ongoing abdominal pain, new or increased bleeding, fever that does not go away, or other symptoms of ulcerative colitis
- You have ulcerative colitis and your symptoms worsen or do not improve with treatment
- You develop new symptoms
There is no known prevention for this condition.
When To See A Healthcare Provider
If you have any symptom that is troubling you, you should speak to a healthcare provider.
In particular, you should see a healthcare provider if you have symptoms like:
- Abdominal pain that does not improve
- Blood in the stools
- Diarrhea that does not go away
- Vomiting that does not go away
- Distended abdomen
Persistent abdominal pain is not normal, and bleeding from the rectum is not normal. If you have any doubts about your health, you should speak with your healthcare provider.
Donât Miss: Quantitative Research On Pressure Ulcer Prevention
Read Also: Is Soy Milk Good For Ulcerative Colitis
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Lifestyle And Home Remedies
Sometimes you may feel helpless when facing ulcerative colitis. But changes in your diet and lifestyle may help control your symptoms and lengthen the time between flare-ups.
There’s no firm evidence that what you eat actually causes inflammatory bowel disease. But certain foods and beverages can aggravate your signs and symptoms, especially during a flare-up.
It can be helpful to keep a food diary to keep track of what you’re eating, as well as how you feel. If you discover that some foods are causing your symptoms to flare, you can try eliminating them.
Here are some general dietary suggestions that may help you manage your condition:
- Limit dairy products. Many people with inflammatory bowel disease find that problems such as diarrhea, abdominal pain and gas improve by limiting or eliminating dairy products. You may be lactose intolerant that is, your body can’t digest the milk sugar in dairy foods. Using an enzyme product such as Lactaid may help as well.
- Eat small meals. You may find that you feel better eating five or six small meals a day rather than two or three larger ones.
- Drink plenty of liquids. Try to drink plenty of liquids daily. Water is best. Alcohol and beverages that contain caffeine stimulate your intestines and can make diarrhea worse, while carbonated drinks frequently produce gas.
- Talk to a dietitian. If you begin to lose weight or your diet has become very limited, talk to a registered dietitian.
You May Like: What To Do For Mouth Ulcers
Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
How Serious Is Ulcerative Colitis
The life expectancy of patients with ulcerative is usually the same as the general population. Ulcerative colitis is a lifelong disease with periods of flare-ups and remissions. The longer the periods of remission, the better will be the general condition of the patient and lower will be the risk of complications. About 10% of patients improve after one attack, and the rest may have multiple flares throughout life. Appropriate treatment, diet, and lifestyle modifications are necessary to prevent complications some of which could be life-threatening. The doctor would advise a treatment plan even during the periods of remission. Regular screening with colonoscopy is required, the frequency of which would be planned by the doctor. It may be done once every one to three years.
You May Like: What Causes Venous Stasis Ulcers
Chronic Inflammatory Bowel Disease The Telltale Symptoms
Symptoms also include fatigue, which manifests itself as severe tiredness with no cause and has a profound impact on the patients personal, social and working life.
Joint, skin, eye and liver problems can also be associated with these diseases: these are immune-mediated extra-intestinal manifestations, which in some cases can even anticipate the typical symptoms of the disease by a few years.
Complications Of Ulcerative Colitis
Complications of ulcerative colitis include:
- primary sclerosing cholangitis where the bile ducts inside the liver become damaged
- an increased risk of developing bowel cancer
- poor growth and development in children and young people
Also, some of the medications used to treat ulcerative colitis can cause weakening of the bones as a side effect.
You May Like: Can Pregnancy Cause Ulcerative Colitis
Preparing For An Appointment
Symptoms of ulcerative colitis may first prompt you to visit your primary care doctor. Your doctor may recommend you see a specialist who treats digestive diseases .
Because appointments can be brief, and there’s often a lot of information to discuss, it’s a good idea to be well prepared. Here’s some information to help you get ready, and what to expect from your doctor.
How Can I Tell If I Have Ulcerative Colitis Or Crohns Disease
Its important that you, your healthcare provider, and a GI specialist work together closely to figure out whats causing your symptoms. This is especially important since the symptoms of Crohns disease and ulcerative colitis can be similar. Your providers may check blood work and a stool sample. To get an accurate diagnosis, your GI specialist may do a colonoscopy, where a camera is pushed into the colon. Your provider will look at the inside of the colon and take tissue samples, which are important for making the right diagnosis. Your providers might get a CT scan or an MRI of your abdomen to check for complications related to your condition.
Read Also: Stage 4 Decubitus Ulcer Treatment
Put Your Health First
If you need to shift your work hours because UC tires you out by the afternoon, let your employer know. Take breaks when you need them so you donât feel overwhelmed.
You know your body. Speak up if you need help or some changes to your work situation so you can get the job done. Make sure you have enough energy to do your work and enjoy your life, too.
Symptoms Of Stones In The Common Bile Duct
Stones lodged in the common bile duct can cause symptoms that are similar to those produced by gallbladder stones. But they may also cause symptoms such as:
- Jaundice .
- Dark urine, lighter stools, or both.
- Fever, chills, nausea and vomiting, and severe pain in the upper right abdomen. These symptoms suggest an infection in the bile duct .
- Rapid heartbeat and abrupt blood pressure drop.
As in acute cholecystitis, patients who have these symptoms should seek medical help immediately. They may require emergency treatment.
Read Also: What Desserts Can I Eat With Ulcerative Colitis
Also Check: Is Avocado Good For Ulcerative Colitis
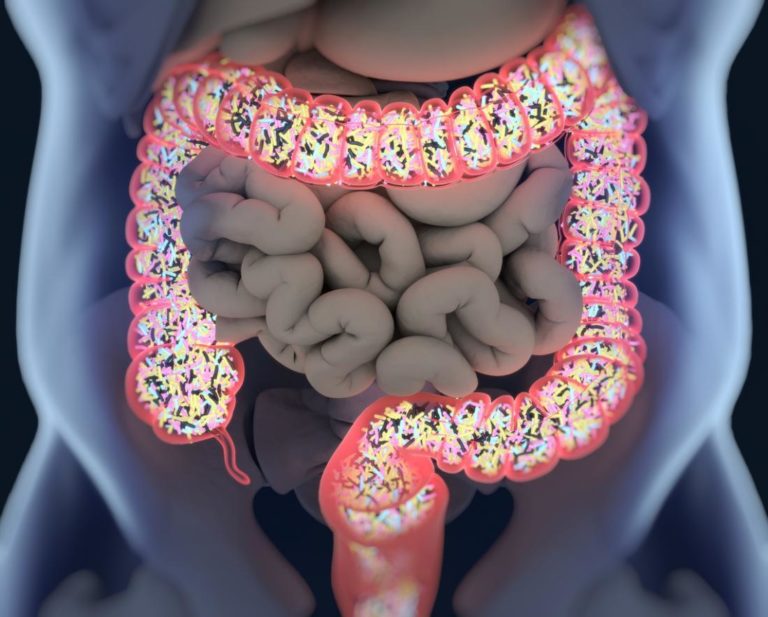
Stanford Scientists Link Ulcerative Colitis To Missing Gut Microbes
Bacteria normally inhabiting healthy peoples intestines and the anti-inflammatory metabolites these bacteria produce are depleted in ulcerative colitis patients, a Stanford study shows.
Aida Habtezion is the senior author of a study that describes how people with ulcerative colitis have insufficient amounts of a metabolite produced by a family of gut-dwelling bacteria.Steve Castillo
About 1 million people in the United States have ulcerative colitis, a serious disease of the colon that has no cure and whose cause is obscure. Now, a study by Stanford University School of Medicine investigators has tied the condition to a missing microbe.
The microbe makes metabolites that help keep the gut healthy.
This study helps us to better understand the disease, said Aida Habtezion, MD, associate professor of gastroenterology and hepatology. We hope it also leads to our being able to treat it with a naturally produced metabolite thats already present in high amounts in a healthy gut.
When the researchers compared two groups of patients one group with ulcerative colitis, the other group with a rare noninflammatory condition who had undergone an identical corrective surgical procedure, they discovered that a particular family of bacteria was depleted in patients with ulcerative colitis. These patients also were deficient in a set of anti-inflammatory substances that the bacteria make, the scientists report.
Ulcerative Colitis And Colonoscopy
Doctors can use a colonoscopy to diagnose UC or determine the severity of the condition.
Before the procedure, a doctor will likely instruct you to reduce solid foods and switch to a liquid-only diet. Then youll fast for a period of time before the procedure.
Typical colonoscopy prep involves taking a laxative the evening before the procedure, too. This helps eliminate any waste still in the colon and rectum. Doctors can examine a clean colon more easily.
During the procedure, youll lie on your side. Your doctor will give you a sedative to help you relax and prevent any discomfort.
During the exam, the doctor will look for signs of inflammation and check for precancerous growth called polyps. The doctor may also perform a biopsy. The tissue can be sent to a laboratory for further examination.
If youve been diagnosed with UC, a doctor may conduct periodic colonoscopies to monitor inflammation, damage to your intestines, and healing progress.
These symptoms are sometimes associated with UC complications.
If you havent been diagnosed with UC, see a doctor if you experience multiple symptoms of the condition. They can help determine whether you may have UC or another bowel disease.
Read Also: Alternative To Sulfasalazine For Ulcerative Colitis
What Should I Ask My Doctor
If you have ulcerative colitis, you may want to ask your healthcare provider:
- How much of my large intestine is affected?
- What risks or side effects can I expect from the medication?
- Should I change my diet?
- Will ulcerative colitis affect my ability to get pregnant?
- What can I do at home to manage my symptoms?
- What are my surgical options?
Whats The Difference Between Ulcerative Colitis And Crohns Disease
UC and Crohns disease are the most common forms of IBD. Both conditions are thought to be the result of an overactive immune system.
They also share many symptoms, including:
However, UC and Crohns disease do have distinct differences. Understanding the key differences between them can help you obtain a proper diagnosis.
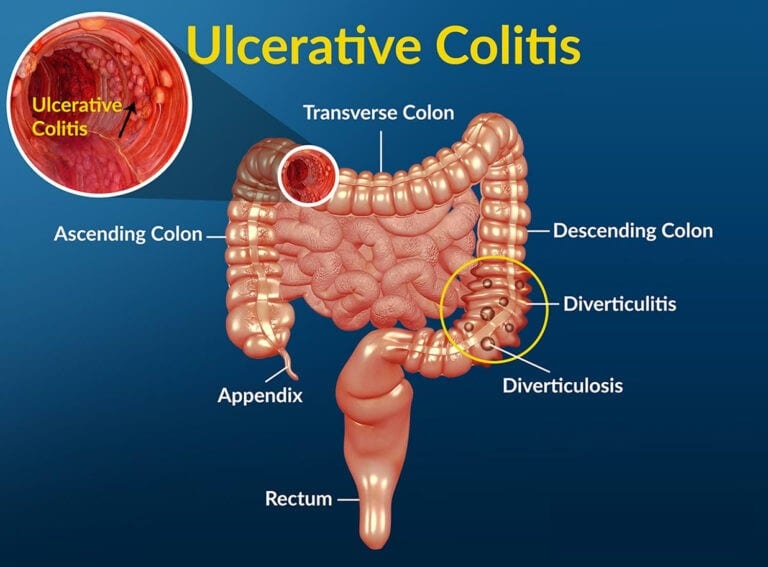
Location
These two conditions affect different portions of the GI tract.
Response to treatment
Similar medications are prescribed to treat both conditions. Surgery is also a treatment option. Its a last resort for both conditions, but it can be a cure for UC, whereas its only a temporary therapy for Crohns.
Dont Miss: Sand Beds For Pressure Ulcers
Recommended Reading: Difference Between Colon Cancer And Ulcerative Colitis Symptoms
Signs Of Possible Colitis
General signs of colitis can include:
- Intense pain
- Swelling of the colon tissue
- Erythema of the surface of the colon
- Ulcers on the colon which may bleed
- Mucus and/or blood in stool and rectal bleeding
- Diarrhea, which may occur, although some forms of colitis involve constipation so the stool and bowel movements may appear normal.
Other symptoms may include gas, bloating, indigestion, heartburn, gastro esophageal reflux disease, cramps, bowel urgency and many other uncomfortable aches in the gastrointestinal system.
Main Difference Colitis Vs Ulcerative Colitis
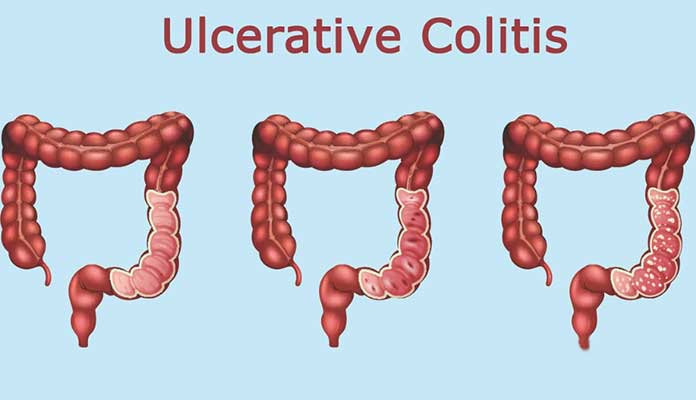
Colitis and ulcerative colitis are two medical conditions which affect the colon. These two terms often used interchangeably since they share similar signs and symptoms. But, it is important to distinguish the difference between them in order to make an accurate diagnosis and treatment. The main difference between colitis and ulcerative colitis is that ulcerative colitis is one form of colitis which results in the chronic inflammation of colonic mucosa and rectum giving rise to ulceration and bleeding.
1. What is Colitis ? Causes, Signs and Symptoms, Diagnosis, and Treatment
2. What is Ulcerative Colitis? Causes, Signs and Symptoms, Diagnosis, and Treatment
3. What is the difference between Colitis and Ulcerative Colitis?
Don’t Miss: Best Dressing For Venous Stasis Ulcer
Expectant Management Of Asymptomatic Gallstones
Guidelines from the American College of Physicians state that when a person has no symptoms, the risks of both surgical and nonsurgical treatments for gallstones outweigh the benefits. Experts suggest a wait-and-see approach, which they have termed expectant management, for these patients. Exceptions to this policy are people at risk for complications from gallstones, including those at risk for gallbladder cancer, such as Pima Native Americans and patients with porcelain gallbladder or with stones larger than 3 cm.
Very small gallstones may increase the risk for acute pancreatitis, a serious condition.
There are some minor risks with expectant management for people who do not have symptoms or who are at low risk. Gallstones almost never spontaneously disappear, except sometimes when they are formed under special circumstances, such as pregnancy or sudden weight loss. At some point, the stones may cause pain, serious complications, or both, and require treatment. Some studies suggest the younger the patient is at diagnosis, the higher the probability of future surgery.
The slight risk of developing gallbladder cancer might encourage young adults who do not have symptoms to have their gallbladder removed.