Food Preparation And Meal Planning
While there is no one-size-fits-all for meal planning, these tips can help guide you toward better daily nutrition:
-
Eat four to six small meals daily.
-
Stay hydrated drink enough to keep your urine light yellow to clear with water, broth, tomato juice, or a rehydration solution.
-
Drink slowly and avoid using a straw, which can cause you to ingest air, which may cause gas.
-
Prepare meals in advance, and keep your kitchen stocked with foods that you tolerate well .
-
Use simple cooking techniques boil, grill, steam, poach.
-
Use a food journal to keep track of what you eat and any symptoms you may experience.
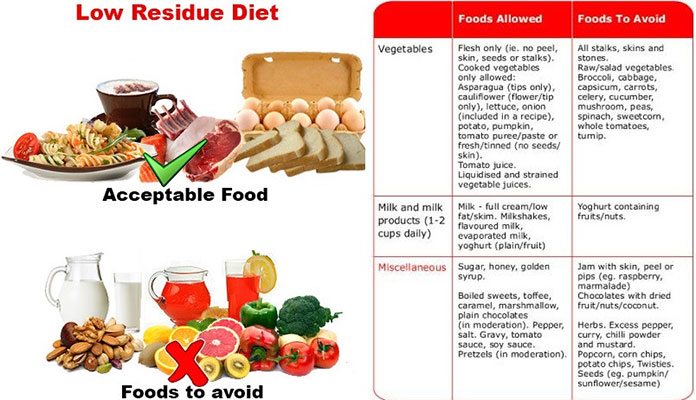
Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
- Diluted juices
Diet Is A Difficult Topic With Crohns And Uc
We dont talk about it because having a conversation about diet is difficult. You know what I mean how often have you tucked into something and been asked should you be eating that with your illness? Or perhaps youve turned down a very fibrous salad even when you are told itll do you good.
If we talk about the food we eat or the food we dont, we sometimes end up feeling ashamed or guilty. We can be made to feel as if were not doing enough to help our bodies or have our disease dismissed as one that is all to do with our lifestyle choices.
Dont Miss: Early Stage Venous Leg Ulcer
Recommended Reading: Can You Develop Ulcerative Colitis Later In Life
Dietary Fibre In Animal Models Of Inflammatory Bowel Diseases
So far, many studies in experimental animal models of IBD have been conducted, evaluating the anti-inflammatory effect of different fractions of fibre. In most studies the therapeutic effect has been linked with an increased luminal production of SCFA after the administration of appropriate sources of dietary fibre. These studies are summarised in the next sections.
In the trinitrobenzenesulfonic acid model of rat colitis, administering a fibre-supplemented diet for two weeks prior to TNBS-colitis induction, and thereafter for 1 week, contributed to a significant reduction of intestinal inflammation. The anti-inflammatory effect was associated with lower tumour necrosis factor levels and lower nitric oxide synthase activity in the large intestine as compared with non-treated colitic rats. Furthermore, it was observed that the study group had higher concentrations of the SCFA in the intestinal contents . In HLA-B27 transgenic rats, administering a diet enriched with Plantago ovata seeds for 13 weeks resulted in a significant decrease in some of the pro-inflammatory mediators, such as NOS, leukotriene B4, and TNF-. As in previous studies, fibre-treated colitic rats had higher concentrations of butyrate and propionate in the intestinal contents than the control group .
Nutritions Role In Treating Uc
Your health care provider can help you make up for these nutritional deficits by identifying foods to help control your UC symptoms and provide you a well-balanced, nutritious diet.
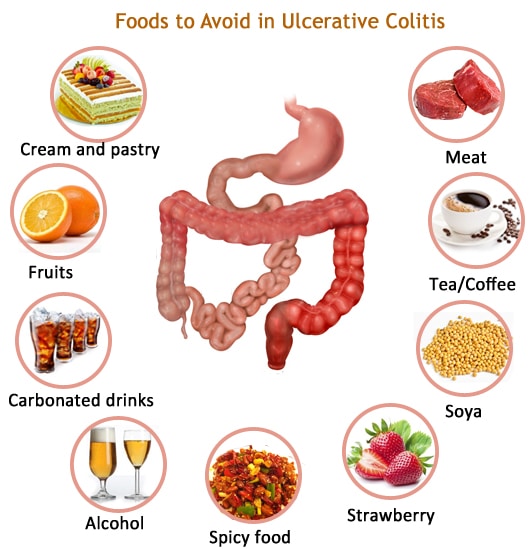
Certain foods or beverages may irritate your digestive tract and trigger flare ups of UC symptoms. Your health care provider will help you identify these foods, so you can avoid them and identify substitute foods that provide the same nutrients, without flare ups.
Foods more likely to trigger UC symptoms include:
-
Plant foods that contain insoluble fiber, such as fruits with skin or seeds raw green vegetables, especially cruciferous vegetables, such as broccoli or cauliflower whole nuts or whole grains and anything with a peel
-
Lactose, a sugar in dairy products, such as milk, cream, and soft cheeses
-
Sugary foods such as pastries and juices
-
Non-absorbable sugars: sugar alcohols found in sugar-free gum, candy, ice cream, and certain types of fruits/juices such as pear, peach, and prune
-
High-fat foods, including fried or greasy foods, butter, coconut, margarine, and cream
Recommended foods for UC include:
-
Refined grains, such as sourdough, potato, or gluten-free bread, white pasta, white rice, and oatmeal
Your health care provider may also recommend:
Don’t Miss: Things To Eat When You Have An Ulcer
Uc And Nutrition: What Is Your Diet Missing
What you eat doesn’t cause or cure ulcerative colitis. But eating a diet thatâs good for you is always a wise idea. It may even help you spend more time in remission and feel better.
Malnutrition isnât usually a problem. Your small intestine is where you absorb vitamins, minerals, and proteins. And UC usually doesnât affect that part of your body.
Still, it can be tricky to eat a well-balanced diet. Many people with UC find certain foods don’t agree with them. And loss of appetite or fear of eating can cause you to lose weight or miss out on nutrients.
The best time to think about nutrition is when you’re not having a flare.
It Can Be Challenging To Differentiate Between Crohns And Uc
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohns Disease here.
|
Our summary of the two conditions is below. You can also read a more detailed explanation about the differences between Colitis and Crohns Disease here.
Read Also: Best Thing To Take For Stomach Ulcer Pain
Foods Allowed On The Spc Diet
- All fresh and unprocessed fruit, organic is preferred
- Non-starchy unprocessed vegetables like mushrooms, asparagus, and brussel sprouts
- All fresh and frozen meats, organic preferred
- Plant-based milk like almond, coconut, or oat milk
- Hard cheeses aged over 90 days
- Nuts and seeds like pumpkin seeds, almonds, walnuts, pecans, and cashews
- Dried navy beans, lima beans, black beans, green string beans, and lentils
Foods To Avoid On The Spc Diet
- Canned or dried fruit processed with additional sugar
- Starchy vegetables like white potatoes, yams, or any canned tomato products
- Processed meats like deli meat, hot dogs, bacon, sausages, and spam
- Processed and breaded products, like chicken nuggets and canned products
- No dairy products like yogurt or butter
- No soft cheeses like feta, cream cheese, or ricotta cheese
- No refined grains or grains of any kind
- No canned beans or soy in any form
You May Like: Ulcerative Colitis Colon Cancer Screening
How Can I Track Foods That Cause Flare
The Crohn’s and Colitis Foundation of America recommends people with ulcerative colitis keep a food journal to keep track of what they eat. Note what you eat and drink, and how you feel afterward, noting any symptoms that arise. Start to keep a list of any foods you suspect may trigger or aggravate your ulcerative colitis symptoms. A food diary will also help you figure out if you are getting adequate nutrition, and can help your doctor or dietician determine the right diet for you to manage your symptoms and prevent flares.
The Crohn’s and Colitis Foundation of America also has an interactive food tracking tool. It is available online or as a mobile app. www.ccfa.org/gibuddy
The Best Diet For Ulcerative Colitis: Splitting Fact From Fiction
Many people claim to have cured ulcerative colitis with diet or supplements.
Unfortunately, there is no diet or pill that can cure the disease.
However, certain diet changes have shown tremendous promise in reducing symptoms and easing discomfort, helping patients live a normal life once more.
This article explains what we currently know about the role of diet in ulcerative colitis.
Contents
Read Also: How Do You Treat A Duodenal Ulcer
Diet During Remission Periods
The nutritional model presented above for patients with exacerbated IBD remains undisputed. However, recommendations addressing the diet of patients in remission are not unambiguous. According to Zallot et al, as many as 2/3 of IBD patients employ an elimination diet to avoid disease exacerbation. Such behavior affects their social life by limiting the occasions when meals are eaten outside the home or in eating different meals to other household members. In spite of such phenomena, numerous official recommendations do not address the subject of nutrition of IBD patients. This is additionally complicated by the fact that investigations carried out by various authors present contradictory results. The next section of this report discusses recommendations presented by various scientific societies as well as the results of studies that may be helpful in planning a diet for IBD patients.
Dont Miss: Vsl 3 And Ulcerative Colitis
Energy And General Health
If youre following a restricted or relatively bland diet to help cope with a flare of ulcerative colitis symptoms, or youre on a liquid-only diet as your body heals from surgery, you may be getting fewer calories and nutrition. As a result, you might not have as much energy as you typically do.
Its important that you try your best to eat enough each day to meet your bodys nutrition and energy needs. Not only to help manage ulcerative colitis but to maintain your overall health.
Complications from IBD, such as infections, may be more likely if your body is weakened from malnourishment, vitamin deficiencies, and dehydration.
Preventing nutritional deficiencies may help prevent flares: In 2017, research from Beth Israel Deaconess Medical Center indicated that people with ulcerative colitis who are in remission may be more likely to experience a relapse of symptoms if they are deficient in vitamin D.
Also Check: Do Enemas Help Ulcerative Colitis
Eating Healthy With Ulcerative Colitis
05.23.2016
When you suffer from ulcerative colitis, one common form of inflammatory bowel disease, you will face nutritional side effects. In this video, Stanford Health Care digestive health nutrition expert Neha Shah, MPH, RD, shares her advice on how to get enough calories and nutrients, despite your ulcerative colitis. Shah offers ideas on avoiding the pain that ulcerative colitis can cause when you eat high fiber or dairy foods. She also has advice on how often and how much to eat.
CARE AT STANFORD
Offering a range of advanced therapies, our experts help patients with gastrointestinal disorders optimize nutrition and improve their quality of life.
Specific Carbohydrate Diet Recipes
With the SPC diet, since youre limiting a lot of carbs, it can be difficult to find recipes with easily accessible ingredients or time to prepare your meals. The Turkey Burger Bowl and Oven-Roasted Whole Chicken recipes are quick and easy to prepare, and youre only eating good carbs!
Turkey Burger Bowl
Ingredients:
1 teaspoon of garlic powder1 teaspoon of onion powder1/2 cup of sliced grape tomatoes1/2 cup of pickles1/2 of sliced small red onion1/2 cup of pitted kalamata olives1 sliced avocado1/2 tablespoon of ghee
Cooking instructions:
Step 1. Heat a large skillet on medium heat with 1/2 a tablespoon of ghee Toss ground turkey into your skillet and drizzle in some garlic powder, onion powder, and salt.
Step 2. Saute the ground turkey until it becomes brown. Meanwhile, divide your lettuce into 2 bowls.
Step 3. Wash and slice your grape tomatoes, red onion, and avocado.
Step 4. Divide the veggies and ground turkey into your two bowls. Drizzle with some melted ghee and condiments of your choice and enjoy!
Oven-Roasted Whole Chicken
Ingredients:
1 whole chicken, 2-3 lbs1 bunch of fresh thyme1 lemon, halved2 tablespoons ghee
Cooking instructions:
Step 1. Preheat oven to 425°F. Remove the insides of the whole chicken and rinse the chicken inside and out. Pat chicken dry after. After dried, place the whole chicken in a baking dish.
Step 4. Allow the chicken to roast for 1.5 hours, or until the juices run clear.
Also Check: How Do You Heal A Bleeding Ulcer
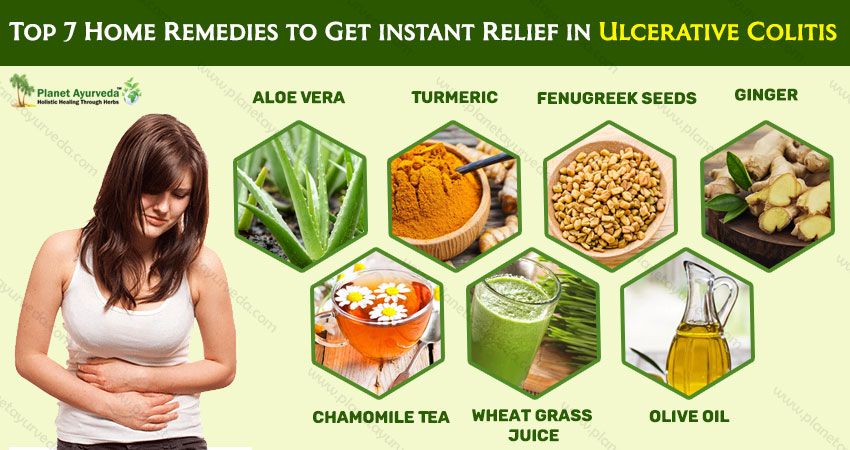
Ulcerative Colitis Diet: What To Eat To Manage Symptoms
A tailored diet for ulcerative colitis may provide you with some relief
Ulcerative colitis is a type of inflammatory bowel disease in which the immune system is thought to attack the gut lining, failing to recognise it as part of the body. A focused ulcerative colitis diet may therefore help with the management of symptoms. With the guidance of an IBD team or a dietician, those suffering from ulcerative colitis can be put on an elimination diet in order to identify potential trigger foods, or may be encouraged to keep a food diary in order to track links between certain foods and symptoms.
Those who have undergone surgery or are struggling with an ulcerative colitis flare up may be put on a low residue diet or a low fiber diet in order to manage symptoms and lessen the burden of their disease.
However, ulcerative colitis diets are often unique to the individual, so some experimentation under medical supervision may be necessary to find the right eating pattern for you. An ulcerative colitis diet may not work at all either, so it is important to collaborate with your medical team in order to properly manage your condition.
Not A Substitute For Conventional Drugs
Seidner says the supplement isnt intended to replace prescription drugs. Generally speaking, individuals do need medication to maintain their disease in remission, he says.
This product is meant to be a complement to standard medical therapy, Seidner continues. People may be able to take a little less medication as a result of this. We dont want people to stop taking their pills.
His study notes that corticosteroids, such as prednisone, are highly effective in moderate to severe ulcerative colitis. Unfortunately, adverse effects are a concern and more than a quarter of patients will relapse when corticosteroid treatment is discontinued, the study notes.
The supplement is a drink containing omega-3 fatty acids from fish oil soluble fiber, which produces short-chain fatty acids and antioxidants. The ingredients were chosen to fight inflammation and improve nutrition.
The supplement is meant to replace a portion of daily calories. If someone were to take the supplement without decreasing their food calories, they would definitely get fat, says Seidner.
For six months, patients ate one-third fewer calories in order to drink about two daily 8-ounce cans of the supplement or placebo . Otherwise, they were told to follow their normal diet.
Supplement and placebo patients had a similar improvement in symptoms, such as stool frequency and rectal bleeding. But the supplement group was able to reduce their need for prednisone much more than the placebo group.
Read Also: What Is An Ulcer Diet
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohns Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohns disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
Foods Allowed On The Mediterranean Diet
- Fruits and vegetables of all kinds
- Whole grains like brown rice, quinoa, oats, whole grain pasta, and bread
- Nuts and seeds, beans and legumes
- Seafood and fatty fish like salmon, shrimp, sardines, and herring
- Omega-3 fats and healthy fats like avocados and olives, ghee
Recommended Reading: What Foods Not To Eat If You Have An Ulcer
Structures And Compositions Of Dietary Fibres
Following many years of debate, the Codex Alimentarius Commission defined dietary fibre as follows:
Dietary fibre means carbohydrate polymers below) with ten or more monomeric units below), which are not hydrolysed by the endogenous enzymes in the small intestines of humans and belong to the following categories: edible carbohydrate polymers naturally occurring in the food as consumed carbohydrate polymers, which have been obtained from food raw material by physical, enzymatic or chemical means and which have been shown to have a physiological effect of benefit to health as demonstrated by generally accepted scientific evidence to competent authorities and synthetic carbohydrate polymers which have been shown to have a physiological effect of benefit to health as demonstrated by generally accepted scientific evidence to competent authorities.
When derived from a plant origin, dietary fibre may include fractions of lignin and/or other compounds associated with polysaccharides in plant cell walls. These compounds also may be measured by certain analytical method for dietary fibre. However, such compounds are not included in the definition of dietary fibre if extracted and re-introduced into a food.
2.2.1. Non-Digestible Oligosaccharides
Also Check: What To Do When Ulcerative Colitis Flares
Diet Types To Consider For Ulcerative Colitis
What diet type is best for those who suffer from Ulcerative Colitis? This is a question many have pondered on and struggled with throughout the history of irritable bowel diseases. There is no single diet proven to aid in decreasing UC symptoms. We definitely know its NOT a diet filled with inflammatory foods, but a diet filled with easily digestible nutritious food for your gut. There are a plethora of recommended diet types for those who suffer from UC. Theres the Mediterranean diet, the Low-FODMAP diet, the gluten-free and dairy-free diet. The only way to know what works best for you is to try an elimination diet or stick with a diet that prevents flare-ups and doesnt upset your gut. How do you know what foods dont upset your gut, you ask. Simply put, going through a period following one diet, meal planning, tracking your symptoms, and food intake with a food diary or food journal tracker will help you pinpoint what foods make you feel good , and what foods make you feel bad.
You mightve read food diary, and immediately gotten anxious at the complexity of tracking your food and figuring out what your body can tolerate. Dont be worried, or scared! Logging your food with a food diary isnt as complex as it sounds.
These tips should not be used for anything other than educational purposes. To develop a safe, personalized meal plan, you MUST work with your doctor or a dietitian.
Read Also: What Causes Ulcers In Your Mouth