What You Need To Know
-
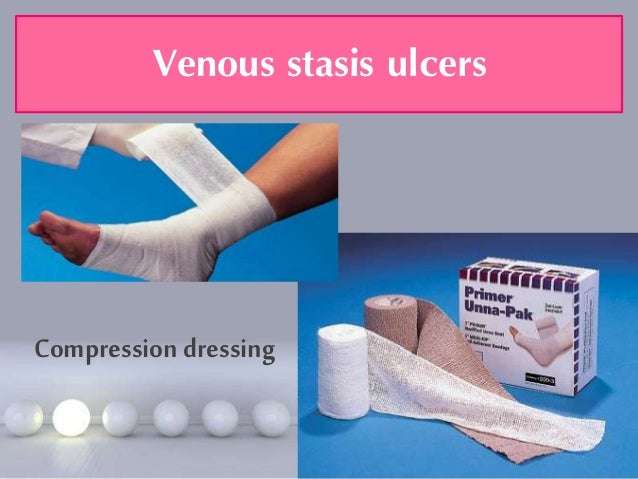
The cornerstone of treatment for venous leg ulcers is compression therapy, but dressings can aid with symptom control and optimise the local wound environment, promoting healing
-
There is no evidence to support the superiority of one dressing type over another when applied under appropriate multilayer compression bandaging
-
When selecting a dressing, look at the wound bed, edge and surrounding skin and decide on the goal of the dressing: for example, if there are signs of localised infection consider an antimicrobial dressing, if there is heavy exudate consider an absorbent dressing
A 65 year old man presents with a two month history of a wound in the gaiter area of his left leg. He has a history of a left leg deep vein thrombosis after a long flight but is otherwise fit and well. He had been self-managing with dressings bought over the counter, but the wound has gradually increased in size. The wound is not painful but is weeping serous fluid, causing irritation of the surrounding skin. Examination shows a 4×3×0.1cm wound above the left medial malleolus. There is haemosiderin deposition, venous flare, and moderate oedema in the limb. The ankle-brachial pressure index is normal at 1.0. He is diagnosed with a venous leg ulcer, which is managed with dressings and compression bandaging.
About 1% of the adult population in Westernised countries are affected by venous ulcers on the leg or foot.2 The prevalence increases with age to 1.7% in
What Happens After Unna Boot Therapy
Once the wound has healed, we often perform vascular studies to determine if there are additional opportunities to help speed recovery.
Depending on your condition, we may help you consider modern vein treatments like Closurefast RFA, Venaseal and Varithena, which when combined with a comprehensive treatment plan can help wounds close quicker and stay closed for longer when indicated.
Have a Wound or Venous Stasis Ulcerthat May Need Treatment?
At Inovia Vein Specialty Centers, we focus on managing issues related to venous insufficiency including venous stasis ulcers, varicose veins, DVTs and more.
Venous Leg Ulcers: 6 Things To Know When Treating Venous Disease
Lower extremity venous disease affects millions of Americans and may ultimately lead to open, draining wounds that adversely affect quality of life. However, there are exciting developments in early diagnosis, prevention and treatment of venous leg ulcers . On the treatment side, there are more choices now than ever before in compression products, which is greatly improving the patient experience. But proper treatment also comes from a better understanding of venous leg ulcers, and better understanding comes from more education. Luckily, were here to help provide education and support for you and your team, so here are six things to know when treating VLUs.
You May Like: Can Ulcers In The Colon Be Cancerous
How Often Should Unna Boots Be Changed
An Unna Boot can be left on for up to 7 days before it needs to be changed. Patients usually return to the clinic to have their boot changed once or twice per week until the wound or ulcer has healed.
At each clinic visit, the state of the wound will be assessed to determine if another Unna Boot needs to be applied.
Patients may need to use Unna Boots for a few weeks until their wound fully heals and stops draining. Usually, the Unna Boot needs to be applied multiple times until the patient can be transitioned to a dry compression wrap or graded compression stocking.
What Types Of Wounds Can Alginate Dressings Heal
Alginate dressings usually do best on wounds that are actively giving out bodily secretions as the gel forms a shield around the sore to help soak up the secretions while keeping all other foreign bodies out of the cut, which lowers risks of infections. Alginate is also useful for wounds that are bleeding profusely as there are calcium fibers in the bandages which can break down and help slow the bleeding of a sore is bleeding heavily. Alginate dressings have long been used to dress wounds including fissures, hyper granulating tissue, interdigital maceration, heloma mole, and other lesions. Alginate dressings have also successfully been used to cover wounds on the parts of the body that are utilized the most such as on the feet. When it comes to healing venous ulcers, more studies are needed to see if Alginate dressings are effective.
If you do have venous ulcers or varicose veins, take a look at our Vein Score tool! After entering your symptoms and zip code, you will receive and vein score and a list of local vein physicians.
Medically reviewed by Dr. Susanne Woloson on 5-01-2020.
*Disclaimer: We are a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for us to earn fees by linking to Amazon.com and affiliated sites.
Medically reviewed by Dr. Susanne Woloson on May 5, 2020
Also Check: Food For Ulcer Patient In Nigeria
The Role Of The Pharmacist In Educating Patients About Vsus
Since pharmacists are often perceived as one of the most accessible healthcare professionals, they have a critical role in the treatment and care of patients at risk of, or with, VSUs. This includes effective patient counseling and education, especially with regard to therapy for VSUs, proper use of medications used to treat VSUs, and reminders about preventive measures to decrease reoccurrence of VSUs. Since the incidence of VSUs is common in elderly and diabetic patient populations, pharmacists play a key role in identifying those patients at greater risk of developing VSUs. Pharmacists should also seize every possible opportunity to remind patients about the critical importance of adhering to therapy to enhance therapeutic outcomes and prevent further complications.
Pharmacists can also reinforce patient education with regard to the preventive measures for VSUs such as staying vigilant about oneâs overall health and adhering to the goals of therapy. Patients should be reminded of the importance of routine wound care and follow-up with their primary healthcare provider, monitoring the ulcer for signs of infection, and immediately seeking medical attention if the wound shows signs of worsening or not healing. Patients at risk for VSUs should be aware that with early diagnosis and implementation of and adherence to therapy, the condition can be effectively treated and healed to avoid complications.
How Can These Ulcers Be Prevented
Once an ulcer has developed, statistics show that another one will develop within 3-5 years. You know that preventing ulcers is well worth the effort if you have experienced the pain and frustration associated with healing wounds. Many patients will continue to wear some type of compression stocking every day while they are on their feet to help the circulation. While a Venous Stasis ulcer may have healed the poor circulation which caused the ulcer has not been corrected. Use AMERIGEL Care Lotion on your lower legs, particularly around the ankles daily. This helps the skin retain its natural moisture, promoting healthier skin that is less prone to problems.
AMERX Health Care Corporation164 Douglas Rd E, Oldsmar, FL 34677 | 448-9599 | AMERXHC.com
AMERX®, AMERIGEL®, HELIX3®, EXTREMIT-EASE®, Where Compression Meets Compliance®, Turn-Key DME®, and Oakin®, are registered trademarks of AMERX Health Care Corporation.
AMERX®, AMERIGEL®, HELIX3®, EXTREMIT-EASE®, Where Compression Meets Compliance®, Turn-Key DME®, and Oakin®, are registered trademarks of AMERX Health Care Corporation.
Also Check: How Do Stomach Ulcers Heal
Where Should Care Be Carried Out
Patients with venous leg ulcers are best managed in the community for two reasons:
-
Maintenance of independence and mobility is important in this elderly population
-
The number of patients would overwhelm hospital services.,
However, direct access to appropriate specialised hospital services is essential for the investigation of underlying vascular disease and for microbiology, histopathology, and dermatology. Having said that, leg ulcer services provided in hospitals often fail to appreciate how many patients with leg ulcers simply refuse to come to hospital, let alone consent to venous investigation or surgery., Few community patients are prepared to be referred for assessment of their underlying venous disease.,,
Rates of healing have been shown to be improved and costs to be reduced when a coordinated service using research based protocols was introduced.,,, Responsibility for patient care should not be removed from community nurses they should be provided with resources and training aimed at delivering an appropriate, high quality service in specialist leg ulcer clinics. Evidence from our own research in two large health authorities in the United Kingdom showed that standards could be maintained only with close supervision when a leg ulcer service was continued without the direct involvement of a leg ulcer nurse specialist, healing rates declined and costs increased.
Criteria For Considering Studies For This Review
Types of studies
We included published and unpublished randomised controlled trials , irrespective of language of report. We only included crossover trials that reported outcome data at the end of the first treatment period and prior to crossover. We excluded studies using quasirandom methods of allocation . We highlighted trials in which three or more interventions were randomised and included all relevant arms.
Types of participants
We included trials recruiting adults described as having venous leg ulcers, managed in any setting. We accepted study authors’ definitions of venous leg ulcers. Where wounds were described only as “leg ulcers” without information as to aetiology, we assumed that they were venous in origin. Trials in which a minority of leg ulcers are described as having a mixed or arterial pathology were included provided that these were fewer than 25% of participants. Trials including other types of mixed wound populations were not included. We included participants at any stage of their treatment process for example, participants with or without ulcers described as being hard to heal or clinically infected.
Types of interventions
* ‘combination dressings’ means two or more dressings applied sequentially over time , or a product containing two or more types of dressing material .
Some of the interventions we considered are as follows we used the categories listed below as the basis for grouping the treatments used in individual studies:
Data synthesis
Don’t Miss: Signs And Symptoms Of Peptic Ulcer
Swelling In The Legs And Ankles
Venous leg ulcers are often accompanied by swelling of your feet and ankles , which is caused by fluid. This can be controlled by compression bandages.
Keeping your leg elevated whenever possible, ideally with your toes above your hips, will also help ease swelling.
You should put a suitcase, sofa cushion or foam wedge under the bottom of your mattress to help keep your legs raised while you sleep.
You should also keep as active as possible and aim to continue with your normal activities.
Regular exercise, such as a daily walk, will help reduce leg swelling.
But you should avoid sitting or standing still with your feet down. You should elevate your feet at least every hour.
How Do I Care For The Wound
AMERIGEL Hydrogel Wound Dressing in indicated for venous stasis ulcers as well as other types of wounds. Apply the wound dressing to your wound along with proper dressing changes twice a day for the first week and then once a day thereafter. Cover the wound with a gauze moistened with AMERIGEL Saline Wound Wash. Next, place a dry piece of gauze over the wet gauze and secure it in place.
Also Check: How To Ease Stomach Ulcer Pain
What Is A Stasis Ulcer
Stasis ulcers, sometimes called venous skin ulcers, affect almost 1% of Americans. These wounds usually occur on the lower legs, especially around the ankles. They can be extremely painful and are very slow to heal, taking an average of six to 12 months to close completely. Worse still, for 70% of patients, ulcers will recur within five years of closure.
Dressings And Topical Agents For Treating Venous Leg Ulcers
What is the aim of this review?
The aim of this review is to find out which dressings and topical agents are most effective for treating a type of wound known as venous leg ulcers. These are longterm wounds in the lower leg caused by problems with blood flow back up the leg through the veins. Researchers from Cochrane found 78 relevant studies to answer this question. Randomised controlled trials are medical studies where patients are chosen at random to receive different treatments. This type of trial provides the most reliable evidence. We evaluated these studies using a method known as network metaanalysis , which allowed us to compare treatments across different studies and to rank them in terms of complete ulcer healing.
Key messages
We cannot be certain which dressings and topical agents are most effective for healing venous leg ulcers: over all studies there were not enough participants per treatment and there was high risk of bias this means that many of the studies were conducted or reported in a way that means we cannot be sure if the results are accurate. The main treatment for venous leg ulcers is compression bandages or stockings and the choice of additional dressings or topical treatments should take into account the review findings and their uncertainty, alongside factors such as patient preference and cost.
What was studied in the review?
What are the main results of the review?
How up to date is this review?
You May Like: Best Treatment For Diabetic Foot Ulcer
What To Expect After Treatment With Cvm
At CVM, we’re ready to help diagnose and treat your leg ulcers at our select wound care locations:
Our expert team will carefully consider all potential chronic pelvic pain causes, with a special emphasis of diagnosing any potential vascular disorders.
We provide complete chronic pelvic treatment for pain. Aside from implementing innovative techniques to treat your pain, including treatments for vascular issues, we’re committed to listening to your concerns and treating your pain seriously. Many of our patients go on to have significant improvement or resolution of their symptoms.
Foam Dressings For Venous Leg Ulcers
Venous leg ulcers are a common and recurring type of chronic wound. Compression therapy is used to treat venous leg ulcers. Dressings that aim to protect the wound and provide a moist environment to aid ulcer healing are applied beneath compression devices. Foam dressings are one of several types of dressing available. We evaluated the evidence from 12 randomised controlled trials that either compared different types of foam dressings, or compared foam dressings with other types of wound dressings. We found no evidence to suggest that polyurethane foam dressings are significantly better or worse than hydrocellular foam dressings in venous leg ulcer healing. Similarly, we found no evidence to suggest that foam dressings are significantly better or worse than other types of dressings , for the healing of venous leg ulcers. We found insufficient evidence to draw any conclusions regarding: adverse events, quality of life, costs, pain, or dressing performance. Overall, the current evidence is of low or unclear methodological quality. This limits the making of any specific recommendations regarding the use of foam dressings. Further, good quality evidence is required before definitive conclusions can be made regarding the role of foam dressings in the management of venous leg ulcers.
You May Like: Best Treatment For Stage 2 Pressure Ulcer
Signs And Causes Of Venous Ulcers
Venous ulcers are non-healing or slow-healing wounds that form as a result of blood pooling in the legs and feet. This happens when the walls or valves in the veins of the lower extremities dont work effectively. This is called venous insufficiency.
Venous ulcers are more common in women and older people. Several factors increase your risk of developing venous ulcers, including:
- Long periods of immobility, such as bed rest
- Older age
How Does It Happen
Gravity works well at getting the blood down to the feet, but when it comes to getting the blood back up the leg towards the knee and thigh, the ankle area becomes most vulnerable. The blood is pushed up the veins when your heart pumps and by your blood pressure. When it cant make it upwards, it pools and collects in the veins, expanding them like a small balloon. The valves in the veins cant open and close properly due to this distention. Tissues inside the skin depend upon the circulatory system to bring nutrients, and to remove waste products from the cells. When the circulation reduces the tissues discolor, devitalize and die. This causes an opening in the skin called ulceration.
You May Like: Can Diet Help Ulcerative Colitis
Best Practices For Venous Leg Ulcer Treatment
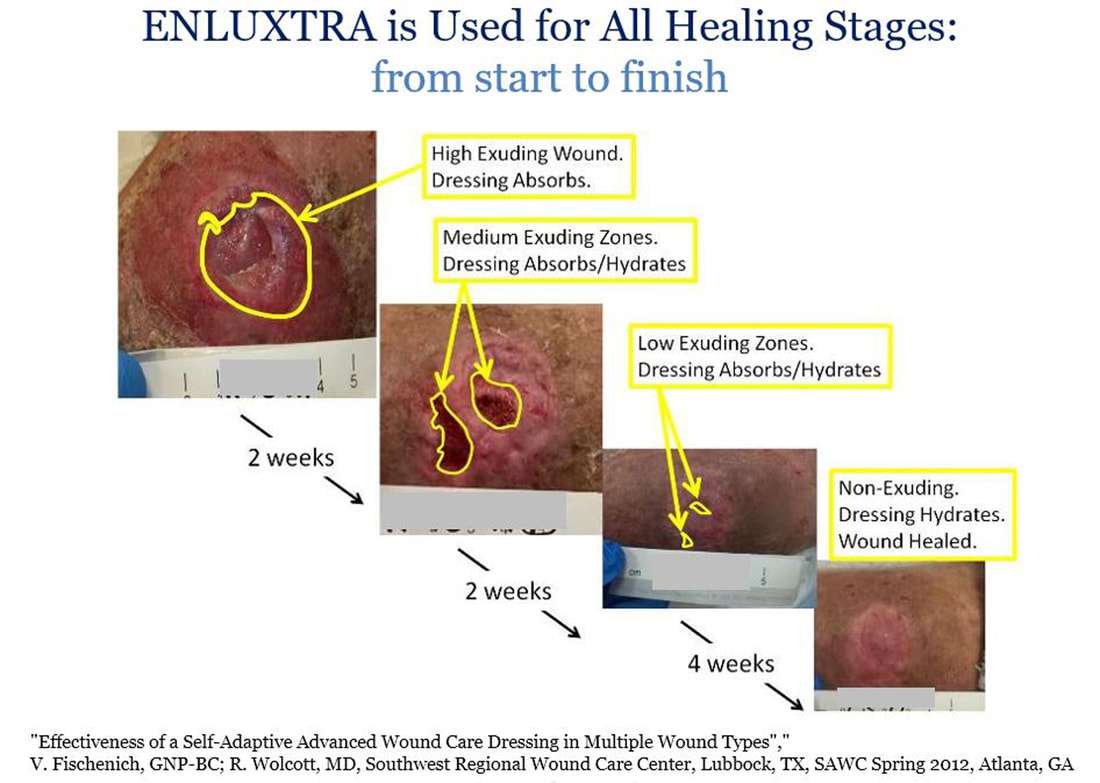
Venous leg ulcer treatment and management require frequent examination of at-risk patients and best practice wound care with a focus on prevention. Without effective treatment, venous leg ulcers can become extremely painful and result in cellulitis, osteomyelitis, and even death.1 To prevent these complications, health care professionals must actively work to identify venous leg ulcers, manage exudate, and choose wound dressings that enable an optimal healing environment. This can help promote rapid healing, reduce costs, and improve quality of life for patients.1
Identifying At-Risk Patients One of the most important components of venous leg ulcer management is prevention. Venous leg ulcers are caused by inflammatory processes that lead to endothelial damage, platelet aggregation, and intracellular edema. By taking steps to identify at-risk patients and regularly assessing them for signs of ulcers, health care professionals can reduce the incidence of the disease. Older adults, obese patients, those with mobility issues, and those who have previously had a venous leg ulcer are all significantly more likely to develop venous ulcers.1
Elevate Legs Leg elevation for 30 minutes three to four times a day can help reduce edema and thus may positively affect inflammation.1
Dress the Wound Dressings aid in the treatment of venous leg ulcers by protecting the wound, preventing adherence of compression bandages, and enabling an ideal healing environment.1,5
What Is The Best Treatment For Venous Ulcers
What is the recommended procedure for treating leg ulcers?
It depends on the cause. If the ulcers are due to varicose veins, then treatment of the varicosities can help significantly in conjunction with a wound care specialist. If due to deep venous reflux, compression stockings and wound care are the best choices.
It depends on the cause. If the ulcers are due to varicose veins, then treatment of the varicosities can help significantly in conjunction with a wound care specialist. If due to deep venous reflux, compression stockings and wound care are the best choices.
Correct any superficial venous reflux.
Correct any superficial venous reflux.
Venous stasis ulcers can be due to deep, superficial, and/ or perforatorvein incompetence deep vein thrombosis can also be involved in theetiology. Before recommending the “best” treatment, venous duplex scanning must be performed and acomprehensive history and physical must be taken by an expert in the field of complex venous disorders. Perforator vein surgery , superficial venous ablation, vein interruptions, or a combination of these treatments may be indicated.
The best treatment for venous ulcers consists of 2 parts, both applied assoon as possible. First, the underlying cause should be identified andtreated. Second, proper compression with edema reduction and specializedwound care is needed until the ulcer heals.
Don’t Miss: Low Residue Diet For Ulcerative Colitis