Summary Of Main Results
We have successfully conducted a network metaanalysis of dressings and topical agents for healing pressure ulcers. Alongside the analysis we have applied a new method of GRADE assessment , which allows us to view the results in the light of our certainty in their findings. Using this approach, we found the majority of the evidence to be of low or very low certainty, and was mainly downgraded for risk of bias and imprecision . This level of uncertainty within the totality of the dataset impacts on all subsequent interpretation of its outputs.
This review includes 51 RCTs involving a total of 2964 participants, comparing 39 different dressings or topical agents for the healing of pressure ulcers. Most of the studies were in older participants, but four included participants with spinal cord injuries and one was in younger people said to be chronically ill or physically disabled. Seventeen studies included participants mainly with Stage 2 pressure ulcers and 15 mainly had Stage 3 pressure ulcers 13 studies investigated treatment of ulcers with a mean duration of less than three months.
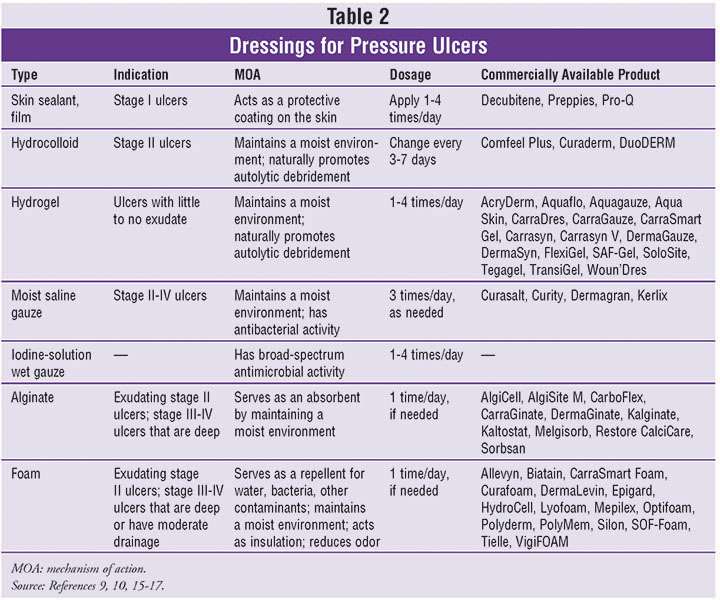
We treated each topical agent as a separate intervention, but initially grouped dressings by class as described in the . The network involved 39 studies in 2116 participants, encompassing 21 different interventions in 27 direct contrasts and these informed 210 mixed treatment contrasts.
When Using Medihoney Will I Need Any Extra Supplies
To properly apply MEDIHONEY, youll need:
-
Your desired MEDIHONEY product
-
Sterile scissors
-
Absorbent secondary bandages, a gauze pad, or a compression garment
MEDIHONEY calcium alginate dressings can be safely worn for up to seven days. Change the dressing as soon as the secondary bandage reaches its absorbent capacity, or as prescribed by your loved ones primary care physician.
Caring For A Pressure Sore
Stage I or II sores will often heal if cared for carefully. Stage III and IV sores are harder to treat and may take a long time to heal. Here’s how to care for a pressure sore at home.
Relieve the pressure on the area.
- Use special pillows, foam cushions, booties, or mattress pads to reduce the pressure. Some pads are water- or air-filled to help support and cushion the area. What type of cushion you use depends on your wound and whether you are in bed or in a wheelchair. Talk with your health care provider about what choices would be best for you, including what shapes and types of material.
- Change positions often. If you are in a wheelchair, try to change your position every 15 minutes. If you are in bed, you should be moved about every 2 hours.
Care for the sore as directed by your provider. Keep the wound clean to prevent infection. Clean the sore every time you change a dressing.
Avoid further injury or friction.
- Powder your sheets lightly so your skin doesn’t rub on them in bed.
- Avoid slipping or sliding as you move positions. Try to avoid positions that put pressure on your sore.
- Care for healthy skin by keeping it clean and moisturized.
- Check your skin for pressure sores every day. Ask your caregiver or someone you trust to check areas you can’t see.
- If the pressure sore changes or a new one forms, tell your provider.
Take care of your health.
Recommended Reading: Can Ulcerative Colitis Lead To Crohn Disease
Side Effects And Restrictions
Most people choose MEDIHONEY for wound care since the product line has almost no side effects. The product is also safe and gentle enough for use on patients of any age. While it is certainly true that MEDIHONEY helps heal wounds faster than traditional wound dressings, the product isn’t free of side effects. The primary side effect reported with the use of MEDIHONEY is a slight stinging sensation that is the result of the slightly acidic pH of the medicine. Most patients find that the ability to heal wounds faster is worth any stinging that accompanies the initial application of the dressing. Children might find the stinging intolerable, but doctors suggest an analgesic before application of the dressing to help limit the stinging sensation.
Contributing Factors Of Pressure Ulcers
Many different issues can lead to a pressure ulcer or bedsore forming on the body. Its important for patients and caregivers to keep these in mind to avoid an ulcer from forming:
- Friction When the skin is rubbed by any material, friction may occur. If a patients skin is sensitive due to injury or other factors, friction can be very high-risk. Wearing soft clothes and changing bed linens regularly can help reduce the amount of friction that occurs when moving.
- Pressure Prolonged periods of pressure on a single part of the body can cause ulcers to form. Patients who cannot get out of bed or out of their chair for many hours need to regularly adjust and move their bodies to place pressure on different areas. The frequency of movement depends on the patient, but laying on a different side every two hours is a common remedy to ensure regular pressure changes.
- Shear When two surfaces move in different directions, shear may occur. This can happen if a patient is improperly seated or sliding down on an elevated bed. Caregivers should be aware of the patients positioning and the possibility of this extra pressure that could exist.
Avoiding these factors can help reduce or eliminate the chance of pressure ulcers from occurring. Every patients body will be different, so a variety of remedies should be considered when trying to stop pressure ulcers from forming.
Read Also: Natural Ways To Heal Stomach Ulcers
You May Like: How Would You Know If You Have An Ulcer
Quality Of The Evidence
We have explored the application of a new approach to GRADE analysis, alongside NMA in STATA . We applied the GRADE approach separately to effect estimates for different contrasts and to the ranking of interventions, but the two aspects are closely interrelated and, in this review, are a consequence of the sparse network and the high risk of bias through much of the network. The effect estimates were exemplified by contrasts of interventions versus saline gauze.
Across the network as a whole, the evidence was of very low certainty. There was overall high risk of bias and overlap of the ranking probability distributions, and no clearcut results. The evidence was of such poor quality that we consider it inappropriate to focus on which treatments had the highest probabilities of healing .
How Are Pressure Injuries Treated
Pressure injuries can be treated in many ways depending on the stage. Once the stage and severity of the wound is determined, it must be cleaned, usually with a saline solution. After the wound is cleaned, it needs to be kept clean, moist, and covered with an appropriate bandage. There are several different types of bandages your doctor may use to dress the wound. These include:
- Water-based gel with a dry dressing
- Foam dressing
- Hydrocolloid dressing
- Alginate dressing
Sometimes debridement is needed. This is a process of ridding the wound of dead tissue. Debridement is an important part of the healing process. It changes the wound from a long-lasting one to a short-term wound. There are several types of debridement. These methods include:
- Ultrasound: Using sound waves to remove the dead tissue.
- Irrigation: Using fluid to wash away dead tissue.
- Laser: Using focused light beams to remove the dead tissue.
- Biosurgery: Using maggots to eliminate bacteria from the wound.
- Surgery: Using surgery to remove the dead tissue and close the wound.
- Topical: Medical-grade honey or enzyme ointments.
Don’t Miss: What To Drink With Ulcerative Colitis
Which Cream Can I Use To Treat Pressure Ulcers Stage 2
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
How Do I Use Medihoney
Before applying a MEDIHONEY product to your loved ones wound, carefully read the instructions on the packaging. Once you do, follow these simple steps:
-
Thoroughly clean the wound with a saline solution. . Then, if necessary, apply a barrier cream around the edges of the wound. Barrier cream prevents skin breakdown and infection.
-
Apply the MEDIHONEY gel or paste directly to the wound. If youre using a calcium alginate dressing, use sterile scissors to resize it, and then gently apply the dressing to the wound bed.
-
Cover the MEDIHONEY gel, paste, or alginate dressing with an absorbent sterile, secondary bandage or a compression garment.
-
When its time to change the dressing, thoroughly clean the wound with a saline solution. Once you do, repeat the same steps.
This video by YouTuber Alyssa McTavish demonstrates the entire process:
Keep in mind that its best that MEDIHONEY be on the skin for 12-24 hours at a time for maximum effectiveness. If you or your loved one is having a hard time keeping the dressing intact, soak a gauze dressing in the MEDIHONEY and apply it directly on the wound, then top with an abdominal pad dressing.
Also Check: Does Ulcerative Colitis Increased Risk Of Colon Cancer
Risk Of Bias In Included Studies
Risk of bias for all included studies is summarised in . In order to represent ‘very high’ risk of bias, we have used two columns so very high risk of bias occurs when the cell is red in the final column .
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study
We judged only one of the 51 studies to be at low risk of bias and ten to have unclear risk of bias . We judged 14 studies to be at very high risk of bias, that is, to have high risk of bias for two or more domains . We assessed the rest of the studies at high risk of bias. We grouped the low and unclear categories together.
*Studies marked with an asterisk were not included in the individual network.
What Is Medihoney Wound Dressing Used For
Medihoney dressings with ALH offers a moist environment that is helpful for wound healing and is indicated for lightly to moderately exuding wounds such as:
- Diabetic foot ulcers
- Pressure ulcers/sores
- Donor sites, and traumatic and surgical wounds
- First and second-degree partial thickness burns
- Leg ulcers
Also Check: How To Treat Skin Ulcer On Leg
Why It Is Important To Do This Review
The diversity of dressings and related materials available to health professionals for treating pressure ulcers makes evidencebased decisionmaking difficult when determining the optimum treatment regimen for a particular patient . With increasingly sophisticated technology being applied to wound care, practitioners need to know the relative effectiveness and costeffectiveness of these sometimes expensive dressings. Even where cost is not an issue, the most effective treatment may not be available or may be difficult or to use, so that information on the second and third best treatments is important too .
Current evidence syntheses include four Cochrane Reviews , two other systematic reviews , and two recent clinical guidelines . Each of these consists of a series of pairwise comparisons. No review finds clear evidence of any effect of one dressing compared to another in terms of assessed outcome measures, including complete wound healing.
In the absence of an overview or network metaanalysis, decisionmakers have to consider the findings of multiple pairwise randomised controlled trials simultaneously and qualitatively to judge, in the face of uncertainty, which dressing they might decide to use. It is extremely difficult to do this effectively, and this difficulty is compounded when the evidence comprises single small trials, about which decisionmakers may have little confidence.
A glossary of NMA terms is given in .
Medihoney Calcium Alginate Dressing
MEDIHONEY® Calcium Alginate Dressing contains 100% active Leptospermum honey impregnated onto a calcium alginate pad. Supports removal of necrotic tissue and aids in wound healing. For wounds with moderate to heavy amounts of exudate or when light packing is needed. Non-traumatic removal.
As wound fluid enters the dressing, the honey is released while the dressing forms a gel Maintains effectiveness even in the presence of wound fluid, blood and tissue Easy to use with potential for extended wear times depending on exudate Promotes a moisture-balanced environment conducive to wound healing Can be used before, during and after negative pressure applications Can be used as a cover dressing for skin grafts or substitutes Helps stalled wounds progress toward healing Osmotic potential draws fluid through the wound to the surface, helping to liquefy non-viable tissue Low pH of 3.5-4.5 – maintaining more acidic pH levels within the wound environment can help to keep a wound on track towards healing Non-toxic, natural and safe
MEDIHONEY® Calcium Alginate Dressing is indicated for moderately to heavily exuding wounds such as: diabetic foot ulcers, leg ulcers , pressure ulcers , first- and second-degree partial-thickness burns, donor sites and traumatic or surgical wounds.
Contraindicated for use on individuals with an allergy to honey, on third-degree burns or to control heavy bleeding.
Store at 50°F-77°F.
Also Check: Eye Drops For Eye Ulcer
How To Use It On The Wound:
Clean: Clean the wound with saline water. Apply: Directly apply the honey gel to the wound bed. Ensure it is in full contact with the wound bed and has approximately 3mm thickness. It is recommended to pair MEDIHONEY® with XTRASORB®, which is a super absorbent cover dressing. Its osmotic gradient pulls exudate to the back of the dressing and converts it into a gel, locking it away even under compression!Whatever you choose, the secondary dressing should be sufficiently absorbent to accommodate the volume of wound exudate. Change: Periodically change the dressing. Do it gently. If the dressing is dry and sticking to the wound bed, moisten it first with normal saline or sterile water. Generally, this antibacterial gel can be left on the wound for up to 7 days depending on the exudate levels. The frequency of changing depends a lot of the amount of drainage coming from your wound. If there is a lot of fluid and the dressing becomes saturated, it may need to be changed more frequently.
The 7 Most Asked Questions About Medihoney
MediHoney® dressings are made with a special honey that is derived from the nectar of the Leptospermum plant. This type of honey has unique properties that have been scientifically verified and shown in clinical trials and by other clinical evidence to be effective for the management of wounds and burns.1-3
In one randomized controlled trial, the mean healing time of wounds treated with MediHoney dressings was significantly faster than the mean healing time of wounds treated with conventional dressings.4
Unlike regular honey, MediHoney is controlled against a rigorous set of systems and standards, including independent monitoring and auditing, to guarantee quality and batch-to-batch consistency. It is also ultra-filtrated and sterilized by gamma irradiation, removing any bacterial spores without loss of product effectiveness.3 MediHoney comes from a traceable source and is free of pesticides and antibiotics.3
Here are the 7 most asked questions about this dressing:
MediHoney dressings aids and supports autolytic debridement and a moist wound healing environment in acute and chronic wounds and burns,5-8 through two key mechanisms high osmolarity and low pH. The high sugar content of honey facilitates movement of fluid from an area of higher concentration, across a membrane, to an area of lower concentration. Osmotic potential draws fluid through the wound, to the surface, helping to liquefy non-viable tissue.
Read Also: Aip Diet For Ulcerative Colitis
Potential Biases In The Review Process
This was a sparse network and there may have been smallstudy effects which impacted on the network . The STATA routines have largely been developed for and tested on larger networks, and our work has contributed to modifications for sparse networks in the netweight routine. Other STATA routines can be modified by the user to take into account smallstudy effects, but we did not explore these approaches because there was too much uncertainty in the network for us to be confident of interpreting the results. Instead, we used the standard routines for NMA and adapted the recent approach to GRADE to bring in sparseness when assessing evidence certainty.
A further effect of the sparseness of the network may have been to hide any inconsistencies. The various statistical tests for inconsistency were generally not significant, but this may have been due to a lack of sensitivity of the tests and the wide CIs around the measures. Despite this, we found inconsistencies in the network for contrasts involving phenytoin. We cannot be sure that there are no other inconsistencies, but this may not matter given the already identified large uncertainties.
How Should A Comprehensive Skin Assessment Be Conducted
The first step in our clinical pathway is the performance of a comprehensive skin assessment. Prevention should start with this seemingly easy task. However, as with most aspects of pressure ulcer prevention, the consistent correct performance of this task may prove quite difficult.
3.2.1 What is a comprehensive skin assessment?
Comprehensive skin assessment is a process by which the entire skin of every individual is examined for any abnormalities. It requires looking and touching the skin from head to toe, with a particular emphasis over bony prominences.
As the first step in pressure ulcer prevention, comprehensive skin assessment has a number of important goals and functions. These include:
- Identify any pressure ulcers that may be present.
- Assist in risk stratification any patient with an existing pressure ulcer is at risk for additional ulcers.
- Determine whether there are other lesions and skin-related factors predisposing to pressure ulcer development, such as excessively dry skin or moisture-associated skin damage .
- Identify other important skin conditions.
- Provide the data necessary for calculating pressure ulcer incidence and prevalence.
Additional Information
It is important to differentiate MASD from pressure ulcers. The following articles provide useful insights on how to do this:
3.2.2 How is a comprehensive skin assessment performed?
- Temperature.
Detailed instructions for assessing each of these areas are found in Tools and Resources .
Also Check: Where Is Stomach Ulcer Pain