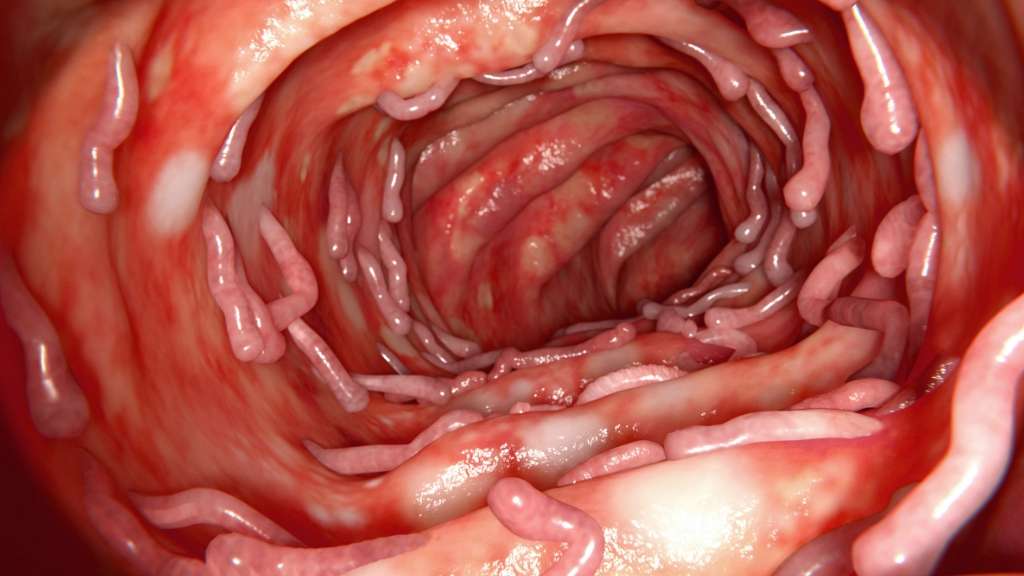
Symptoms Of Ulcerative Colitis
Ulcerative colitis can sneak up on you as the symptoms typically start slowly and can be brushed aside as something you ate or another stomach upset. But, if left to progress, ulcerative colitis can be a very debilitating disease with life-threatening complications.
If you are having any of the following symptoms, its important that you connect with your healthcare provider to determine what the cause is.
Frequent diarrhea often accompanied by blood
Abdominal pain and cramping
An urgency to defecate but an inability to do so completely
Unexplained weight loss
Regular fatigue
Fever
The cause of ulcerative colitis is unknown. Its been tied to diet and stress in the past, but its really not known if these are causes or if theyre aggravating factors.
Buyer Beware For Probiotics Users
In the U.S., probiotics are marketed as dietary supplements, so they havent gone through the same rigorous FDA testing as drugs.
This means we have no way of knowing for certain if a product has the bacterial strains or the concentration of bacteria that its label claims.
The higher-ups at the FDA are hoping to change this soon, but for now, we have to go by our own experience and hope for the best.
That Seems To Be A Theme Of Microbiome Research Everyone Agrees On Its Profound Effect On Our Health But Getting To Where You Could Change Something Meaningfully To Treat A Disease Is A Different Thing
Right, we are not there yet. Its very complicated. As we have said many times, the genome of the microbes is thousands of times more complex and more numerous than the human genome. When we are talking about personalized medicine, we are really talking about the microbiome: how to understand all the subtle interactions with the human host, and how to possibly exploit this for health reasons. Its an incredibly interesting area, and my colleagues here at the University of Chicago, David Rubin, MD, Eugene Chang, MD, Cathryn Nagler, PhD, Bana Jabri, MD, PhD and others are actively working on this. We arent there yet, but we will. I have great enthusiasm in this. I think this is the medicine of the future.
Matt Wood
You May Like: Eye Drops For Eye Ulcer
Probiotic Fact #: Probiotics Are Strain Dose & Duration Specific
When we evaluate the research on a probiotic in our practice, we always consider the strain name of a probiotic.
When identifying a probiotic, there are three parts to a name:
- The first part is the genus.
- The second part is the species.
- The third part is the strain.
The letters and numbers after that specify the STRAIN of probiotic which is the most important identifying factor when it comes to probiotics. In research on probiotics- the strain name is what differentiates it from the sometimes hundreds of others in its category.
However, many probiotics do not even list the strain name which makes it hard to even evaluate its effectiveness. Not understanding which strain is being used is one major reason why people disagree on the use of probiotics and why its so hard to find consistent information on probiotics for IBD.
The bottom line is: If the strain isnt listed, avoid it.
Beyond strains, the specific dose and how long you take a probiotic can also play a role in its effectiveness. For example, if the evidence shows that it takes 6 weeks to reduce symptoms while taking 10 billion CFUs, we cant expect that taking 1 billion of the same strain for 2 weeks will yield the same results.
Yet oftentimes people will assume probiotics work at every level and any time duration. Like most things- the quality and duration of use can really make a difference. Avoid experimenting on yourself and go with what we know works in research.
Also Check: Childrens Mouth Ulcers Treatment
Benefits Of Taking Probiotics

Not all probiotics are the same. Different strains of the bacteria have different effects. For example, one strain may fight against cavity-causing organisms in our mouths and don’t need to survive a trip through our guts.
Research has been promising for these friendly critters. Potential benefits of probiotics have been seen in the treatment or prevention of
- H. pylori
- vaginal infections
- infection of the digestive tract caused by Clostridium difficile
- pouchitis
- eczema in children.
Also Check: What Causes H Pylori Ulcers
How Will I Feel Taking Probiotics
Again, this really varies from person to person. Some people who take probiotics – whether they have IBD or not – report feeling bloated and gassy or have a short bout of diarrhoea at the beginning. This may be a reaction to the changes in bacteria in your gut. To help prevent this some probiotic companies recommend you start by taking a small dosage and build up to taking the full dose to allow your body to adjust. If you are concerned, or these symptoms persist, you should stop taking the probiotic and speak to your doctor.
Caution should be taken around taking probiotics when you are on immunosuppressant medications or are acutely unwell – always speak to your doctor before starting a probiotic to check it is safe for you to do so.
Choosing A Probiotic Supplement
Probiotics can also be taken as dietary supplements. Certain strains of bacteria are cultivated, then sold in powder, liquid, pill, or capsule form. Most probiotic supplements are not regulated or tested for effectiveness by the U.S. Food and Drug Administration . For this reason, finding probiotic supplements that actually work for ulcerative colitis may be difficult. Look for products that contain at least 1 billion colony forming units, or CFUs. The most researched types of probiotic strains are Lactobacillus and Bifidobacterium, which have both been studied as possible treatments for ulcerative colitis.
Don’t Miss: Ulcerative Colitis Unspecified Without Complications
Inflammatory Bowel Disease And The Gastrointestinal Microbiota
The causes of IBD have not been fully elucidated, but are thought to involve both genetic and environmental factors. More recently, a number of observations have suggested that the intestinal microbiota may drive intestinal inflammation. First, experimental animal models of IBD remain healthy when reared in a germ-free environment and develop inflammation only after colonisation with commensal bacteria . Second, higher concentrations of bacteroides and enterobacteria are found in regions of inflamed mucosa in CD . Third, in both CD and pouchitis disease activity deteriorates when the faecal stream is surgically restored to previously-defunctioned intestine, implying that the lumen contents are necessary for the development of inflammation. Finally, the association between ileal CD and mutations in the bacterial-sensing caspase-activating recruitment domain 15 gene implicate bacterial recognition as a central pathogenic process .
The present review aims to assess the evidence that these observations from in vitro experiments and animal models can be put into clinical practice. The evidence presented relates to trials that have assessed these therapies in terms of clinical outcomes in IBD, and the data extracted and presented are the clinical end points in each study.
What Are The Best Probiotics For Ulcerative Colitis
So, which of the probiotics being sold today can be considered as the best probiotics for ulcerative colitis? Most likely you are having a hard time deciding which one to get with all the options available. The good news is that we have rounded up probiotics that we think will help lessen the pain and symptoms associated with ulcerative colitis. Here are some that you should check out.
- Doctors Elite Nutrition Probiotic Complete Natural Dietary Supplement
- Our rating
- Hyperbiotics PRO-15 Natural Probiotic Supplement
- Our rating
- Culturelle Probiotics Kids Dietary Supplement Chewables
- Our rating
- Garden of Life Dr. Formulated Probiotics Raw Probiotic Supplement
- Our rating
Overview:
If you are looking for the best probiotic for ulcerative colitis, you might want to consider Doctors Elite Nutrition Probiotic for your needs. What makes this product worth looking into is that it helps replenish the good bacteria in your tummy for better digestion. It can provide relief from gas, bloating, and even irregularity in bowel movements. It might even help you lose weight because it can help with speeding up your metabolism. Both men and women can take this supplement for their gut health.
Read Also: How To Diagnose Gastric Ulcer
What Are The Causes And Risk Factors Of Lymphocytic Colitis
The exact cause of lymphocytic colitis is unclear. It can sometimes be related to autoimmune diseases or infection. Autoimmune conditions cause the immune system to attack healthy cells in the body, often causing inflammation, as is found in lymphocytic colitis. Some researchers believe it is caused by something unfamiliar in the digestive tract, such as bacteria, pollen, or foods previously foreign to the body.
Certain medicines are also known to occasionally cause the condition. These include antidepressants, anti-inflammatories found in certain pain medications excluding steroids, medications for high cholesterol, medications for acid reflux, and medications for diabetes. Smoking is also linked to the development of lymphocytic colitis, often occurring after the patient quits smoking. Other studies have found a connection between coffee drinking and lymphocytic colitis, but these findings are not well documented.
Dont Miss: Best Probiotic For Gut Healing
Probiotics Can Aid Digestion And Help Maintain Gut Health
What are the benefits of taking probiotics? Bacteria have a reputation for causing disease, so the idea of tossing down a few billion a day for your health might seem literally and figuratively hard to swallow. But a growing body of scientific evidence suggests that you can treat and even prevent some illnesses with foods and supplements containing certain kinds of live bacteria. Northern Europeans consume a lot of these beneficial microorganisms, called probiotics , because of their tradition of eating foods fermented with bacteria, such as yogurt. Probiotic-laced beverages are also big business in Japan.
Some digestive disease specialists are recommending probiotic supplements for disorders that frustrate conventional medicine, such as irritable bowel syndrome. Since the mid-1990s, clinical studies suggest that probiotic therapy can help treat several gastrointestinal ills, delay the development of allergies in children, and treat and prevent vaginal and urinary infections in women.
Self-dosing with bacteria isnât as outlandish as it might seem. An estimated 100 trillion microorganisms representing more than 500 different species inhabit every normal, healthy bowel. These microorganisms generally donât make us sick most are helpful. Gut-dwelling bacteria keep pathogens in check, aid digestion and nutrient absorption, and contribute to immune function.
Also Check: Stelara Indications For Ulcerative Colitis
Do Probiotics Help Ulcerative Colitis And Crohn’s Disease
Researchers are starting to think that imbalances in our gut microbiome are linked to many diseases, ailments and even our mental health.
There is increasing evidence that suggests intestinal microbiota plays a role in initiating, maintaining and determining the characteristics and development of IBD1, 2. And, some people with IBD do report that taking probiotics can help with easing some of their symptoms.
However, studies into the effectiveness of probiotics on people with IBD are limited. There have been a few studies into specific strains of bacteria and their effect on IBD and even fewer studies specifically testing probiotic products on IBD. Generally, at the moment, the research shows that some specific probiotics may be helpful for people with ulcerative colitis but the evidence in Crohns Disease is less convincing.
Some of these studies include:
Probiotic product specific
VSL#3 and pouchitis. The study concluded that high doses of the probiotic VSL#3 are effective in the treatment of mild pouchitis3.
VSL#3 and ulcerative colitis. The study demonstrated that VSL#3 is effective in achieving clinical responses and remissions in patients with mild-to moderately active UC4.
Some studies have also been carried out into Crohn’s disease and microscopic colitis.
Symprove and ulcerative colitis. The study found that 76% of those with ulcerative colitis taking part in the study had significant reductions in faecal levels of calprotectin5.
Bacteria strain specific
Probiotics For Ulcerative Colitis
The AGA doesnt recommend probiotics for treating ulcerative colitis outside of use in a clinical trial. As with Crohns disease, the limitations in the type of studies that have been done so far are the main factor in this decision.
The AGA found 11 studies done using probiotics for treating ulcerative colitis. They used various different strains of probiotics, which makes comparing these studies difficult.
There were four studies that compared the use of probiotics with the medications mesalamine or balsalazide. A few of the studies allowed co-therapy with steroids and one was done with the use of probiotic enemas in children.
While the evidence was considered low, the AGA does indicate that for some of the studies, the benefit was uncertain. There was one study that showed a potential for benefit. This appears to be in contrast to Crohns disease, where there doesnt seem to be much indication that probiotics might be beneficial.
Theres a call for more research and there are no recommendations for using probiotics for ulcerative colitis.
Read Also: Can Food Allergies Cause Ulcerative Colitis
How To Take Probiotics
When you take probiotics for UC, there are two key things to know.
To keep up the benefits, you have to keep taking the probiotics. If you stop, the balance of bacteria in your colon will change and you may get a flare-up. Talk to your doctor about a long-term probiotic plan.
Probiotic Foods And Supplements
It is always wise to consult your health care provider regarding the use of probiotics to help treat symptoms of Crohns disease. Probiotics generally do not have severe side effects and are usually safe to take to promote the health of your microbiome.
Probiotics can be ingested through drinks, food, or supplements. There are many different strains of probiotics. Lactobacillus, Bifidobacterium, and Saccharomyces boulardii are easily found at your grocery store.
Some foods and beverages rich in probiotics include:
- Yogurt
- Fermented pickles
- Kefir
As one MyCrohnsAndColitisTeam member said, I have been making my own milk kefir for three years now. Best natural probiotic there is.
Supplements containing probiotics such as Escherichia coli Nissle 1917, L. rhamnosus GG, Bifidobacterium longum, and Bifidobacterium breve are also available over the counter. These probiotic supplements include VSL#3, which some members report works well for Crohns. As one member said, My son has Crohns and his GI suggested VSL#3 because it is especially made for people with digestive diseases.
Another member shared, I have been taking VSL#3 probiotics for about three weeks now and I think it is really helping with my awful diarrhea.
Supplements are not regulated by the U.S. Food and Drug Administration, so consult your health care provider before trying them, and use them with care.
You May Like: What Causes Ulcers On The Feet
You May Like: Do Ulcers Cause Acid Reflux
What Are The Benefits Of Probiotics For Ulcerative Colitis
Is it worth getting the best probiotic for ulcerative colitis? Although probiotics should not be considered as a treatment for this digestive problem, it does have its benefits to your inflamed gastrointestinal tract. Here are some possible advantages to taking probiotics for your ulcerative colitis.
Treatments For Lymphocytic Colitis
What is lymphocytic colitis?
Lymphocytic colitis is a type of microscopic colitis, a condition characterized by chronic non-bloody watery diarrhea. People with lymphocytic colitis have a normal appearing bowel when assessed by an endoscope or an X-ray but have microscopic inflammation of the bowel when assessed by a biopsy . The cause of this disorder is unknown. This review is an update of a previously published Cochrane review.
What treatments have been tried for lymphocytic colitis?
Budesonide, mesalazine with or without cholestyramine, beclometasone dipropionate and bismuth subsalicylate have been tried as treatment for lymphocytic colitis. Budesonide is an immunosuppressive steroid drug that is quickly metabolized by the liver resulting in reduced steroid-related side-effects. It is taken by mouth. Beclometasone dipropionate is also a steroid drug. Steroid drugs are used to treat inflammation. Mesalazine is an anti-inflammatory drug which is often taken by mouth. Cholestyramine is a drug that helps the body remove bile acids. Pepto-Bismol®, is an antacid medication used to treat temporary discomforts of the stomach and gastrointestinal tract.
What did the researchers investigate?
The researchers investigated whether these drugs improve the symptoms of lymphocytic colitis or microscopic inflammation and whether any side effects result from treatment. The researchers searched the medical literature extensively up to 11 August 2016.
What did the researchers find?
You May Like: How Did I Get Ulcerative Colitis
Who Shouldnt Take Mesalamine
Mesalamine may not be safe if you have certain medical conditions, including:
- An allergy to aspirin or sulfasalazine
- Heart, liver, or kidney disease
- A blockage in your stomach or intestines
- Swelling of the heart muscle, called myocarditis
- Swelling of the sac around the heart, called pericarditis
- Skin problems like eczema or atopic dermatitis
Mesalamine may cause more liver, kidney, and heart risks in older adults. Your doctor might need to adjust the dose to prevent these problems.
Youll need to avoid Apriso if you have the inherited condition phenylketonuria . This medicine contains the artificial sweetener aspartame, which people with PKU must avoid.
Let your doctor know if youre pregnant, you could become pregnant, or youre breastfeeding. There havent been enough studies to show that mesalamine is safe to take during pregnancy. You can safely use this medicine while you breastfeed, but let your doctor know if your baby has diarrhea or other side effects.
Recommended Reading: Can You Get An Ulcer In Your Intestines