Be Consistent With Treatment Drugs
Take your medications consistently. Dont miss or skip a dose even when in remission. Dont try to wean yourself off of a treatment drug as these changes can all lead to flares.
Contact Digestive Health Services at if you have any changes to your flares, or if you think you might have ulcerative colitis.
I Take Medication Regularly Can A Flare
Unfortunately, yes. Ulcerative colitis is a chronic condition. Medications and lifestyle changes can help reduce the intensity and frequency of ulcerative colitis flare-ups, but not stop them completely.
Regular flare-ups may indicate a problem with your current treatment. If you are taking your medications as prescribed and still experiencing flare-ups, you should contact your physician who may adjust your medication or suggest other treatment options.
Why Working With A Qualified Care Team Is So Important When It Comes To Managing Ulcerative Colitis
People being treated for UC typically arent getting dietary or lifestyle advice, which is a huge disservice, says Cohen. But managing ulcerative colitis and preventing flare-ups can be done! You just might need a little help from the experts.
Because UC isnt one-size-fits-all and triggers are highly individual, enlisting the help of a care team like the clinicians at Parsley Health is wise. Providers can provide individualized supplement protocols based on lab testing, customized eating plans for periods of remission and flares, and communicate with your current GI doctor if necessary to streamline care.
Read Also: Cpt Code For Ulcerative Colitis
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Understanding The Stress Response
If someone asked you to describe what it feels like to be stressed, you might describe being on edge or like any minute, the other shoe will drop. But stress is more than an emotional reactionthere are important physiological changes that happen when you are feeling stressed, too, says Lindsay Bottoms, Ph.D., head of the Center for Research in Psychology and Sports Science at Hertfordshire University in Hertfordshire, U.K. Our body responds to stress by releasing hormones which increase our heart rate and our breathing and tense our muscles, she says. Stress essentially prepares us to fight or run away, which is why it is known as the flight or fight response. In cases of imminent danger, this stress response is invaluable, providing the energy to get away from dangerous situations.
Recommended Reading: Are All Ulcers Caused By H Pylori
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
What Are The Symptoms Of Ulcerative Colitis
Ulcerative colitis symptoms often get worse over time. In the beginning, you may notice:
- Diarrhea or urgent bowel movements.
- Abdominal cramping.
- Liver disease.
- Loss of fluids and nutrients.
Symptoms are similar in pediatric ulcerative colitis and may also include delayed or poor growth. Some ulcerative colitis symptoms in children can mimic other conditions, so it is important to report all symptoms to your pediatrician.
Recommended Reading: Can Ulcerative Colitis Lead To Crohn Disease
What Are Some Practical Steps To Take When A Flare
The first thing to do if a flare up occurs is to make sure you are eating a healthy diet which is low in fibre and contains plenty of water. Avoiding dairy products and cutting down carbohydrates may also help. The vast majority of people will requite adjustments to their medication, so you should seek medical advice from your GP or specialist.
Find New Stress Management Techniques
Stress can trigger a colitis flare-up, so practice stress management techniques to reduce as much external stress on your body as possible.
Why does stress affect irritable bowel diseases so easily? Cortisol can increase inflammation in your body, and learning to manage stress can help you reduce that inflammatory response.
Reduce your stress levels through:
- Daily exercise
- Practicing deep breathing
- Prioritizing self-care
Self-care includes getting enough sleep each night, following a well-balanced diet, and setting aside time for your favorite activities each day.
Recommended Reading: How To Treat An Ulcer In Your Esophagus
Who Gets Ulcerative Colitis
Anyone at any age, including young children, can get ulcerative colitis. Your chance of getting it is slightly higher if you:
- Have a close relative with inflammatory bowel disease .
- Are between 15 and 30 years old, or older than 60.
- Are Jewish.
- Use frequent nonsteroidal anti-inflammatory drugs like ibuprofen .
Diet Recommendations For Crohn’s Disease Flare
- Follow a low residue diet to relieve abdominal pain and diarrhea.
- If you have strictures, it is especially important to avoid nuts, seeds, beans and kernels.
- Avoid foods that may increase stool output such as fresh fruits and vegetables, prunes and caffeinated beverages. Cold foods may help reduce diarrhea.
- If you have lactose intolerance, follow a lactose-free diet. Lactose intolerance causes gas, bloating, cramping and diarrhea 30 to 90 minutes after eating milk, ice cream or large amounts of dairy. A breath hydrogen test may confirm suspicions of lactose intolerance.
- If you have oily and foul-smelling stools, you may have fat malabsorption. Treat fat malabsorption by following a low-fat diet. Discuss these symptoms with your doctor or nutritionist.
- Smaller, more frequent meals are better tolerated and can maximize nutritional intake.
- If your appetite is decreased and solid foods not tolerated well, consider taking nutritional supplements .
You May Like: What Does A Stomach Ulcer Feel Like
Now I Can Go About My Day Normally Without Many Preparations
Rosanne Mottola, 36, dealt with excruciating pain when she was diagnosed with ulcerative colitis while in college in 2006. I was living with debilitating gut pain and having urgent and severe bowel movements 20 times a day, she tells SELF. Most of the time there was blood present.
Mottola was officially diagnosed with ulcerative colitis a few months before she graduated from college. I had to arrange for several of my finals to be given virtually since I couldn’t sit in a classroom for an hour to take my exams, she says. In addition to the gut symptoms, I was exhausted and anxious.
Mottola learned to manage her condition by taking extreme measures to try to avoid symptoms when she needed to be away from a bathroom. Anytime I had to go anywhere, I would wake up hours before I had to leave just to settle my stomach, she says. Often, prior to an eventsuch as my weddingI would load up on Imodium A-D to prevent having to go to the bathroom.
How To Reduce Ulcerative Colitis
Without treatment, people with UC tend to relapse.
For many people with mild or moderate symptoms, things improve somewhat after diagnosis. This is thanks to medication, along with identifying and avoiding triggers.
More aggressive cases are less common, and only a small number of severe cases will require hospitalization.
Repeated flare-ups can indicate problems with your current treatment, so speak with your doctor and discuss adjusting your medication.
Several classes of medication now exist that can help you get into and stay in remission. Your doctor may need to add another type or increase your dosage.
The only way to prevent UC flare-ups is to have surgery. The most common type of UC surgery is the proctocolectomy, which involves the removal of the rectum and colon.
Candidates for UC surgery include people who:
- have sudden or severe disease
- have a perforated colon
- are at risk for colorectal cancer
- are unable to tolerate their UC medications due to side effects
- have stopped responding to their UC medications
In addition to knowing how to manage flare-ups, its also helpful to recognize factors that can trigger your flare-ups.
Read Also: In Order To Prevent Pressure Ulcers
Do Any Medications Have Nutritional Side Effects
Moderate to severe flares of IBD are often treated with corticosteroids , cholestyramine and 5-ASA compounds . These medications have nutritional side effects that should be addressed. If you use any of these medications, talk to your doctor or registered dietitian for treatment advice.
- Prednisone causes decreased absorption of calcium and phosphorus from the small intestine. It also causes increased losses of calcium, zinc, potassium and vitamin C. With continual use of high doses of prednisone, the result may be bone loss and development of bone disease. People on prednisone may need up to 1200 milligrams a day. Protein needs also are increased for people taking prednisone because it increases protein breakdown in the body.
- Cholestyramine decreases absorption of fat-soluble vitamins , as well as folate, vitamin B-12, calcium and iron.
- Sulfasalazine interferes with folate absorption. People taking this drug also should take a 1 milligram folate supplement each day.
Prevention Is Key: Know Your Triggers
We know youve heard it before: Prevention really is key when you have UC. While flares are, unfortunately, unpredictable, there are known factors that may worsen your UC symptomscommon ones include missing a dose of your UC meds, stress, antibiotics, nonsteroidal anti-inflammatory drugs, smoking, and food choices, according to the Crohns and Colitis Foundation.
Work with your GI doctor to get on a treatment plan to manage your UC and remember: The perfect time to build other positive UC habits are when youre feeling good, says Dr. Nandi.
- Dehydration and UC: Crohns and Colitis UK. . Dehydration. crohnsandcolitis.org.uk/about-crohns-and-colitis/publications/dehydration
- Mindfulness and Pain Study:Frontiers in Human Neuroscience. . Pain Perception Can Be Modulated by Mindfulness Training: A Resting-State fMRI Study. ncbi.nlm.nih.gov/pmc/articles/PMC5102902
- Managing IBD Flares and Symptoms: The Crohns and Colitis Foundation. . Managing Flares and IBD Symptoms. crohnscolitisfoundation.org/sites/default/files/2019-07/managing-flares-brochure-final-online.pdf
Don’t Miss: What Does An Ulcer Look Like
Adjusting Your Diet To Reduce Ulcerative Colitis Pain
There isnt one diet thats best for everyone with UC. It’s best to focus on getting balanced and diverse nutrition from a variety of foods. Cutting out whole food groups is unnecessary unless you have known food allergies or intolerances . For some people, following the guidelines of the Mediterranean diet is helpful.
Work With Your Doctor
Youâll need to see your doctor regularly. It may be every 6 months while youâre in remission. Youâll have routine procedures like colonoscopies and bloodwork to check on your UC.
If youâre having a flare-up, make sure to check in with your doctor. UC isnât the only thing that causes digestive symptoms. They may need tests to rule out something else, like an infection. Or you may need your prescriptions adjusted.
Certain symptoms mean you need help right away. Call your doctor if you:
- Canât keep liquids down
- Have severe diarrhea
- Have a fever
You May Like: Aloe Vera Gel For Horses Ulcers
Find Ways To Chill Out
All of the stress-busting suggestions above are extra important when youre in the midst of a flare-up. Cohen also recommends implementing deep breathing exercises before every meal, as this relaxes your body and mind allows you to digest more optimally. And, since youll be eating 4-6 smaller meals, this is a great way to get a dose of calm at multiple points in the day.
Managing Ulcerative Colitis Flares: The Most Important Step
The key to managing an ulcerative colitis flare is to get a confirmed diagnosis and begin treatment as soon as possible. But doing so can be tricky, because people with the condition may attribute their symptoms to other GI problems, says Oriana Mazorra Damas, MD, an assistant professor of gastroenterology at the University of Miami Miller School of Medicine in Miami.
The goal for remission is to feel well enough that you forget that you have the condition for most of the day in other words, you experience few, if any, symptoms, Dr. Damas explains.
Read Also: Blood Clots In Stool With Ulcerative Colitis
Ways To Naturally Treat Ulcerative Colitis
Is yoga the key to soothing ulcerative colitis? Will an herb provide relief? Natural remedies for ulcerative colitis may not be your primary treatment approach, but they can help you manage symptoms and reduce the frequency of flares.
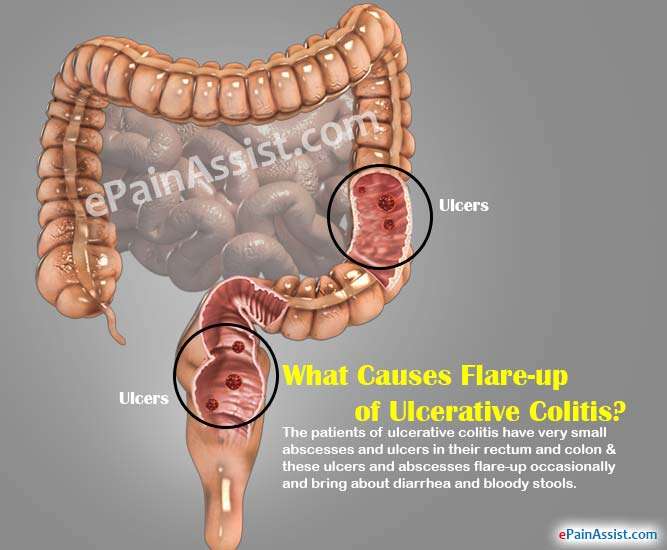
To date, there is no cure for UC, a chronic disease of the large intestine in which inflammation brought on by a faulty immune response creates sores or ulcers in the lining of the colon.
The chronic condition affects nearly 1 million Americans and tends to run in families. Epidemiological research shows that Westernized populations and people with diets high in fat are at higher risk for UC, as well as Caucasians and Ashkenazi Jews. But no one has yet uncovered the main cause of the disease.
Although the official cause of ulcerative colitis has evaded the medical community, its important to understand that it results from an interaction of genetic, environmental, and lifestyle factors, says Benjamin Snider, ND, a naturopathic doctor in private practice in Kitchener, Ontario.
Treatments for ulcerative colitis include medications such as nonsteroidal anti-inflammatory drugs, immune system suppressors, and steroids to control inflammation and other symptoms of the condition. Surgery to remove the colon and rectum is another form of treatment if medication doesnt prove effective.
- Wheatgrass juice
- Curcumin
Read on to learn about some different kinds of natural therapies.
Talk With Others Who Understand
MyCrohnsAndColitisTeam is the social network for people with ulcerative colitis and their loved ones. On MyCrohnsAndColitisTeam, more than 138,000 members come together to ask questions, give advice, and share their stories with others who understand life with ulcerative colitis.
Are you living with ulcerative colitis pain? What has helped you to manage it? Share your experience in the comments below, or start a conversation by posting on your Activities page.
You May Like: Low Dose Naltrexone Ulcerative Colitis
Limit Intake Of Animal Products
Especially meats/red meats. I have read in many articles that because many people have low stomach acidity and poor digestion, meats tend to rot in our guts, thus producing pus and contributing to inflammation . This rotting can produce more intestinal gas and overall slower digestion. I personally try to limit my meat intake to 1-2 meals per week !
Consider Therapy To Help Manage Stress And Pain
Working with a therapist on certain mind-body techniques can help you control ulcerative colitis symptoms.
Cognitive behavioral therapy and a technique called biofeedback may be useful, as these processes teach skills to cope with stress and pain. In CBT, you learn to recognize and change behaviors and emotions that affect you physically. According to an article in Therapeutic Advances in Gastroenterology, CBT can ease abdominal pain for some people. Biofeedback will teach you how to identify and control some bodily processes, such as heart rate or tension in your muscles, and it can be effective in helping manage chronic pain.
Don’t Miss: Best Diet For Ulcerative Colitis Flare Up
The Leaky Gut Autoimmune Connection
If youâve been keeping up with our autoimmune series articles, you already know itâs nearly impossible to ignore a leaky gut as part of the cause and solution to autoimmunity.
Alessio Fasano, M.D. has been on the forefront of recent autoimmune disease research and published a paper titled âLeaky Gut and Autoimmune Diseases.â
His findings present the idea that in order for an autoimmune disease to develop, 3 conditions must all exist together:
For those with Ulcerative Colitis, healing the gut means so much more than just physical healing it means overcoming the mental and emotional symptoms as well.
Healing a leaky gut is one factor thatâs in our control and it can be done step-by-step with the right plan.
Soothe Skin Irritation And Pain
Bouts of diarrhea often can bother your skin. Use moist towelettes for wiping. Follow up with a petroleum jelly ointment. Need more relief? Soak in a saltwater bath, which may ease soreness. Try acetaminophen for pain, but avoid NSAIDs, such as ibuprofen and naproxen. They can trigger flares and cause other problems.
3
Also Check: Best Feed For Ulcer Prone Horses
Is Ulcerative Colitis A Genetic Disease
Nearly 15% of those with Ulcerative Colitis have a first degree relative who also suffers from the condition. In identical twins, the rate of UC is about 16%, whereas in non-identical twins that number drops to 4%.
The exact genes are yet to be determined, but the following highlights some of the newest research on genetics and Ulcerative Colitis:
- A total of163 at-risk genes/loci have been identified in UC. A large study of 29,838 IBD patients recently identified three new loci in association with inflammatory bowel disease: NOD2, MHC, and MST1 3p21.
- IL-13 is the main interleukin responsible for the inflammation and chronic symptoms of UC. It causes epithelial barrier damage, reduces the speed of mucosal repair, and contributes to alterations of the tight junctions in the gut. The addition of IL-13 to cell cultures increases the flux of large molecules such as mannitol and lactulose and also affects the speed of mucosal repair by 30%.
- IL-10 is an anti-inflammatory cytokine which has a positive effect on UC. It inhibits the production of certain players that cause inflammation and the inactivation of IL-10 was shown to cause chronic ileocolitis in mice, indicating a protective role within the mucosal layer.
So, what does this all mean?
Genetics certainly play a role when it comes to UC, but genetics alone arenât enough to explain why IBD has jumped from 2 million people in 1999 to over the 3 million mark weâre seeing today.