What Is Ulcerative Colitis
Ulcerative colitis is a chronic disease in which abnormal reactions of the immune system cause inflammation and ulcers on the inner lining of your large intestine.
Ulcerative colitis can begin gradually and become worse over time. However, it can also start suddenly. Symptoms can range from mild to severe. In between periods of flarestimes when people have symptomsmost people have periods of remissiontimes when symptoms disappear. Periods of remission can last for weeks or years. The goal of treatment is to keep people in remission long term.
Talking To Your Doctor
No matter how long youâve had UC, talking about it can feel difficult. Use our quiz to help you take a fresh look at life with UC, then talk to your GI about your disease and the different opportunities available to you for your treatment plan.
Please see full Prescribing Information, including BOXED WARNING and Medication Guide.
You are encouraged to report adverse events related to Pfizer products by calling .
If your doctor has prescribed XELJANZ and you need help paying for it, XELSOURCE may be able to assist, depending on eligibility, terms and conditions.
This site is intended only for U.S. residents. The products discussed in this site may have different product labeling in different countries. The information provided is for educational purposes only and is not intended to replace discussions with a healthcare provider.
XELJANZ is a registered trademark of Pfizer Inc. The brand names included throughout are the properties of their respective owners.
XELJANZ is available in 5 mg and 10 mg tablets.
XELJANZ XR is available in 11 mg and 22 mg extended-release tablets.
XELJANZ Oral Solution is available in 1 mg/mL oral solution.
© 2022 Pfizer Inc. All rights reserved.
© 2022 Pfizer Inc. All rights reserved.
Indications
XELJANZ/XELJANZ XR is used to treat adults who have tried TNF blockers with:
XELJANZ/XELJANZ Oral Solution is used to treat patients 2 years of age and older with:
It is not known if XELJANZ XR is safe and effective in children.
XELJANZ & Pregnancy
Is Ulcerative Colitis Serious
Unfortunately ulcerative colitis, or UC as its often referred to, does have the potential to be a serious illness due to some of the complications it can cause.
However, its important to remember that most people with ulcerative colitis dont experience some of the more serious complications that can occur due to receiving effective treatment. To help minimise your risk of complications you should follow the treatment prescribed by your doctor.
Some of the things that can cause serious complications include…
You May Like: What To Eat If You Have A Bleeding Ulcer
Does Ulcerative Colitis Make You Immunocompromised
Ulcerative colitis doesnt make you immunocompromised. Some of the medicines that treat it may change the way your immune system responds. This change is different for each medication. Some of these changes may increase the risk of certain infections or other issues. A discussion with your health care team before starting a medication is the best way to understand these risks and ways to prevent them.
Emotional Impact Of Ulcerative Colitis
Living with a long-term condition that is as unpredictable and potentially debilitating as ulcerative colitis, particularly if it is severe, can have an emotional impact. In some cases anxiety and stress caused by ulcerative colitis can trigger depression.
You may find it useful to talk to others affected by ulcerative colitis, either face to face or via the internet.A good resource would be your local patient association. This website, operated by the UKs leading charity for people affected by ulcerative colitis, contains details of local support groups. The site also contains a large range of useful information on ulcerative colitis and related issues.
Don’t Miss: Ulcerative Colitis Pain After Eating
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
When To Contact A Medical Professional
Contact your provider if:
- You develop ongoing abdominal pain, new or increased bleeding, fever that does not go away, or other symptoms of ulcerative colitis
- You have ulcerative colitis and your symptoms worsen or do not improve with treatment
- You develop new symptoms
There is no known prevention for this condition.
Don’t Miss: Ulcerative Colitis Iv Infusion Treatment
National Experts In Inflammatory Bowel Diseases
The Penn State Health Inflammatory Bowel Disease Center experts are national leaders in the IBD field. Our team has been awarded top honors for exceptional IBD care, including being named on Castle Connollys list of Americas Top Doctors. We are proud to provide our patients with the latest in diagnostic testing, as well as a wide range of medical, dietary and surgical therapy options.
Preparing For An Appointment
Symptoms of ulcerative colitis may first prompt you to visit your primary care doctor. Your doctor may recommend you see a specialist who treats digestive diseases .
Because appointments can be brief, and theres often a lot of information to discuss, its a good idea to be well prepared. Heres some information to help you get ready, and what to expect from your doctor.
Recommended Reading: Ldn For Ulcerative Colitis Reviews
You May Have An Increased Risk Of Osteoporosis
The reason undertreated and untreated ulcerative colitis can lead to osteoporosis is twofold, according to Bonthala. One is that active inflammation steals from the bones. Patients are in the bone-building phase of their life until their mid-30s, so if you have active inflammation, youre depleting nutrients from your bones, and youre not absorbing a lot of the nutrients your bones need, she explains.
The second reason: Flares that arise from poorly managed ulcerative colitis are often treated with steroids, which themselves can lead to osteoporosis. I get a lot of referrals for bone density tests in ulcerative colitis patients in their early 20s, she says.
How Is Colitis Diagnosed
Your healthcare provider will begin by asking you about your symptoms, when they began and what you were eating and drinking at the time. Theyll ask you about your current medications and any health conditions that youve been recently treated for. Theyll physically examine you, then move on to medical tests. These are likely to include blood tests, stool tests and imaging tests to look at your colon.
Blood tests involve drawing a small amount of your blood through a needle and sending it to a lab to analyze. Stool tests involve taking a sample of your poop and sending it to the lab. Proteins in your blood and stool can show evidence of inflammation and sometimes indicate a particular type of infection. Imaging tests can confirm inflammation and give more detailed information about your condition.
In particular, endoscopic tests that visualize the inside of your colon with a lighted scope can be helpful in diagnosing the type of colitis you have. Endoscopic exams, including colonoscopy and flexible sigmoidoscopy, allow healthcare providers to take tissue samples from the inside of your colon . Healthcare providers can learn important information by examining tissue samples in the lab.
Recommended Reading: What To Avoid Eating If You Have An Ulcer
Outlook For People With Ulcerative Colitis
If you have UC, a doctor will need to monitor your condition, and youll need to carefully follow your treatment plan throughout your life.
The only true cure for UC is removal of the entire colon and rectum. Your doctor will usually begin with medical therapy unless you have a severe complication that requires surgery. Some people will eventually require surgery, but most do well with nonsurgical therapy and care.
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Read Also: Icd 10 Code For Ulcerative Colitis With Bleeding
You May Have An Increased Risk Of Colorectal Cancer
When theres inflammation in the colon, the cells in the lining of the colon continuously turn over to try to repair the damage, explains the Crohns & Colitis Foundation. This constant turnover can increase the odds of a mutation occurring that can lead to cancer.
If there are any irregular polyps or growths in your colon, unchecked inflammation can make it difficult for your doctor to spot them during a colonoscopy. You really want to have a clean slate when you do a colonoscopy, so your doctor can be sure everything looks good, Bonthala says.
The Risks Of Untreated Ulcerative Colitis
Treating ulcerative colitis is important to prevent complications
Ulcerative colitis is a chronic illness that is a type of inflammatory bowel disease . Ulcerative colitis is usually characterized as causing inflammation in the lining of the colon, but it is an immune-mediated condition. This means that it involves the bodys immune system, which can lead to effects in organs and body systems other than the digestive tract.
A diagnosis of ulcerative colitis is difficult to receive for many reasons. Often people have not even heard of the disease before their diagnosis. Learning that it will probably mean taking medication for the rest of their lives can be upsetting and daunting.
In addition, ulcerative colitis goes through periods of active disease and less active or no activity . Little is currently known about why ulcerative colitis might flare-up, though some people living with the disease are able to identify their personal triggers.
Don’t Miss: How To Heal A Bleeding Ulcer
Remember Tell Your Doctor Right Away If You Have An Infection Or Symptoms Of An Infection Including:
- Fever, sweats, or chills
- Warm, red, or painful skin or sores on your body
- Diarrhea or stomach pain
- Urinating more often than normal
- Feeling very tired
HUMIRA is given by injection under the skin.
This is the most important information to know about HUMIRA. For more information, talk to your health care provider.
Uses
HUMIRA is a prescription medicine used:
- To reduce the signs and symptoms of:
- Moderate to severe rheumatoid arthritis in adults. HUMIRA can be used alone, with methotrexate, or with certain other medicines. HUMIRA may prevent further damage to your bones and joints and may help your ability to perform daily activities.
- Moderate to severe polyarticular juvenile idiopathic arthritis in children 2 years of age and older. HUMIRA can be used alone or with methotrexate.
- Psoriatic arthritis in adults. HUMIRA can be used alone or with certain other medicines. HUMIRA may prevent further damage to your bones and joints and may help your ability to perform daily activities.
- Ankylosing spondylitis in adults.
- Moderate to severe hidradenitis suppurativa in people 12 years and older.
US-HUM-210186
Reference: 1. HUMIRA Injection . North Chicago, IL: AbbVie Inc.
Living With Ulcerative Colitis
Ulcerative colitis, a disease that causes inflammation and sores in the digestive tract, affects everyone in a different way. About 10% of people get better after one attack, but its more likely that youll have flares that come and go throughout your life.
You may go weeks or years without any symptoms. Thats called remission. The longer you go without a flare, the better your overall health will be.
Your doctor will likely give you medicine to control inflammation and other symptoms.
If you dont feel like your UC is under control, talk to your doctor. They may want to change your medicine dose or switch you to a different drug. If that doesnt work, you may need surgery.
Read Also: What Foods Do You Eat When You Have An Ulcer
Don’t Miss: Can You Take Imodium If You Have Ulcerative Colitis
Ulcerative Colitis Vs Crohns Disease
Ulcerative colitis and Crohns disease share similar symptoms and they are both types of inflammatory bowel disease , but they are not the same illness and they affect different areas of the GI tract.
- Can affect the entire thickness of the bowel wall
- Only the colon and rectum are affected
- Affects the inner-most lining of the large intestine
- What is Ulcerative Colitis?
Common Symptoms Of Ulcerative Colitis
While UC symptoms can vary over time and from person to person, the most common symptoms are diarrhea with blood and abdominal discomfort.
However, your symptoms may vary depending on where inflammation occurs in your GI tract and how severe it is.
Other signs and symptoms include:
- An urgent need to have a bowel movement
- Nausea or loss of appetite
- Anemiaa condition in which the body has fewer red blood cells than normal
Recommended Reading: Diet To Heal Ulcerative Colitis
Why Ulcerative Colitis Needs Treatment
Ulcerative colitis needs ongoing treatment, and the options available will vary depending on a number of factors, including if the disease is considered mild, moderate, or severe.
In many cases, the disease will respond to treatment but it may take some trial and error, as well as time, to find the right regimen. People with ulcerative colitis will use a variety of methods to keep the disease under control including medication, diet, supplements, and lifestyle modifications.
However, its now known that while keeping symptoms at bay is important for quality of life, there can be inflammation in the colon even though someone with ulcerative colitis feels well. Having inflammation, even if it causes few or no symptoms, has effects on the body that can be far-reaching.
For this reason, gastroenterologists who treat IBD are becoming increasingly focused on working to calm that inflammation. Without treatment, the inflammation from ulcerative colitis can lead to complications.
In some cases, especially when feeling better, people living with ulcerative colitis may consider stopping treatment. This is a decision that should be made while working closely with a gastroenterologist. Stopping treatment without discussing it first can have unintended consequences that go beyond the disease coming back. In addition, if there is inflammation that is not being managed, it could lead to consequences.
Lifestyle And Home Remedies

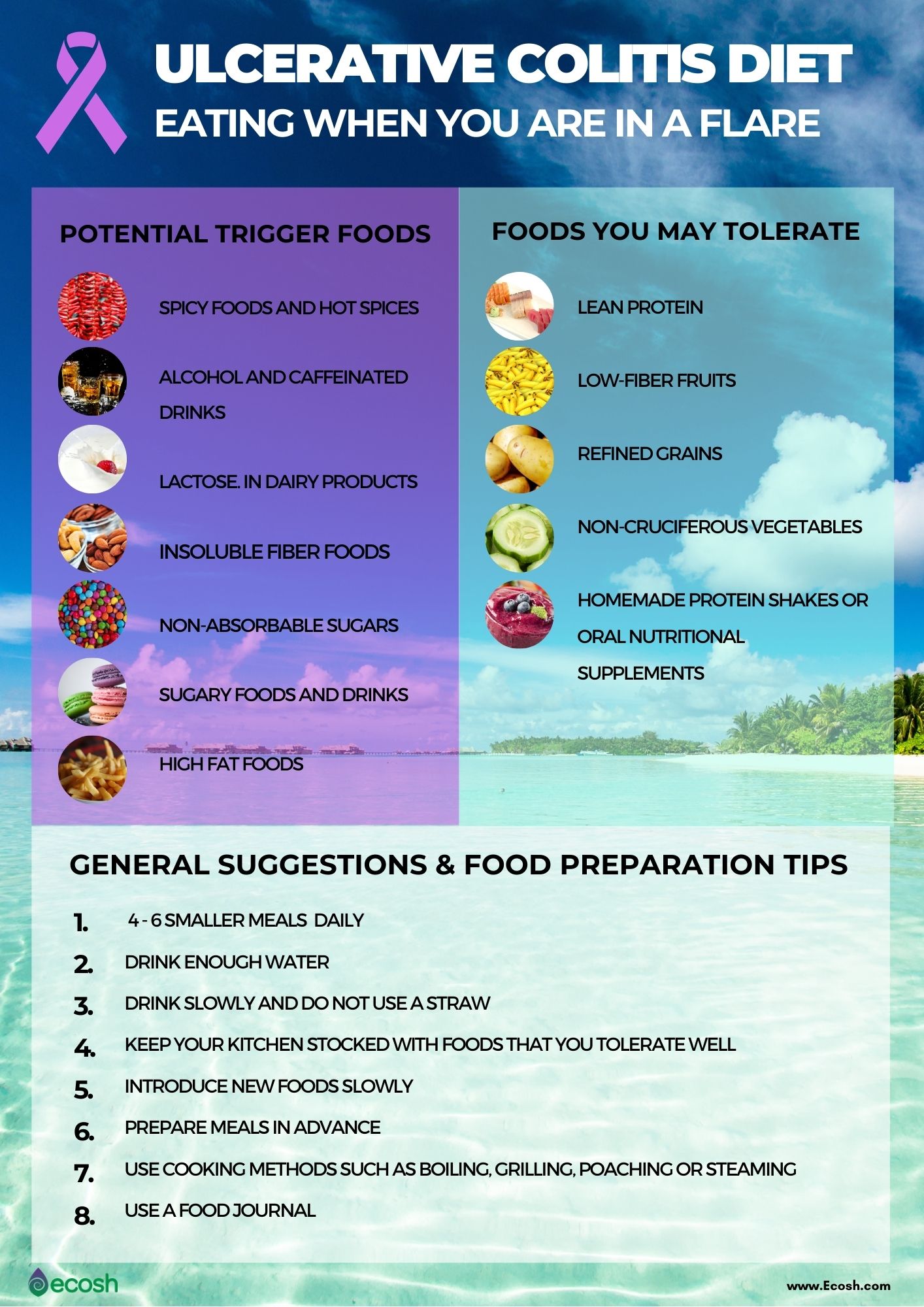
Sometimes you may feel helpless when facing ulcerative colitis. But changes in your diet and lifestyle may help control your symptoms and lengthen the time between flare-ups.
Theres no firm evidence that what you eat actually causes inflammatory bowel disease. But certain foods and beverages can aggravate your signs and symptoms, especially during a flare-up.
It can be helpful to keep a food diary to keep track of what youre eating, as well as how you feel. If you discover that some foods are causing your symptoms to flare, you can try eliminating them.
Here are some general dietary suggestions that may help you manage your condition:
- Limit dairy products. Many people with inflammatory bowel disease find that problems such as diarrhea, abdominal pain and gas improve by limiting or eliminating dairy products. You may be lactose intolerant that is, your body cant digest the milk sugar in dairy foods. Using an enzyme product such as Lactaid may help as well.
- Eat small meals. You may find that you feel better eating five or six small meals a day rather than two or three larger ones.
- Drink plenty of liquids. Try to drink plenty of liquids daily. Water is best. Alcohol and beverages that contain caffeine stimulate your intestines and can make diarrhea worse, while carbonated drinks frequently produce gas.
- Talk to a dietitian. If you begin to lose weight or your diet has become very limited, talk to a registered dietitian.
You May Like: What To Do For Mouth Ulcers
You May Like: Ulcer In Colon Found In Colonoscopy
Types Of Ulcerative Colitis
The type of ulcerative colitis you have depends on where it is in your body:
- Ulcerative proctitis is usually the mildest form. Itâs only in the rectum, the part of your colon closest to your . Rectal bleeding may be the only sign of the disease.
- Proctosigmoiditis happens in your rectum and the lower end of your colon . Youâll have bloody diarrhea, belly cramps, and pain. Youâll have the urge to poop, but you wonât be able to.
- Left-sided colitis causes cramps on that side of your belly. Youâll also have bloody diarrhea, and you might lose weight without trying. Youâll have inflammation from your rectum up through the left side of your colon.
- Pancolitis often affects your entire colon. It can cause severe bouts of bloody diarrhea, belly cramps, pain, fatigue, and major weight loss.
- Acute severe ulcerative colitis is rare. It affects your entire colon and causes severe pain, heavy diarrhea, bleeding, and fever.
What Are The Complications Of Ulcerative Colitis
Ulcerative colitis may lead to complications that develop over time, such as
- anemia, a condition in which you have fewer red blood cells than normal. Ulcerative colitis may lead to more than one type of anemia, including iron-deficiency anemia and anemia of inflammation or chronic disease.
- bone problems, because ulcerative colitis and corticosteroids used to treat the disease can affect the bones. Bone problems include low bone mass, such as osteopenia or osteoporosis.
- problems with growth and development in children, such as gaining less weight than normal, slowed growth, short stature, or delayed puberty.
- colorectal cancer, because patients with long-standing ulcerative colitis that involves a third or more of the colon are at increased risk and require closer screening.
In some cases, ulcerative colitis may lead to serious complications that develop quickly and can be life-threatening. These complications require treatment at a hospital or emergency surgery. Serious complications include
Severe ulcerative colitis or serious complications may lead to additional problems, such as severe anemia and dehydration. These problems may require treatment at a hospital with blood transfusions or intravenous fluids and electrolytes.
Read Also: Chia Seeds For Horses With Ulcers