He Had Recurring Pain For Nearly A Decade
The pain woke the 52-year-old physician from a dead sleep. It was as if all the muscles in his right leg, from those in the buttock down his thigh to the very bottom of his calf, were on fire. He shifted slightly to see if he could find a more comfortable position. There was a jag of pain, and he almost cried out. He glanced at the clock: 4 a.m. In just three hours he would have to get up. He had a full day of patients to see. Massage didnt help. He couldnt get comfortable lying flat, so finally he moved to the living room, to a recliner. Only then, and only by lying completely still, did he manage to get the pain to abate. He drifted off, but never for long. The searing pain in his leg and buttock slowly eased, and by the time his alarm went off, he could stand and walk though his muscles still ached and he had to baby his right leg, causing a limp.
Between patients, he arranged to see his own doctor. Hed had pain off and on in his buttocks, one side or the other, for more than a year. The pain was in the middle of each cheek and was worse when he was sitting and at the end of the day. Walking to and from his car on the way home was brutal. And then, as mysteriously as it came, it would disappear only to come back a week or two later.
Recommended Reading: Does Ulcerative Colitis Make You Tired
Basics Of Inflammatory Bowel Disease
Arthritis means inflammation of joints. Inflammation is a body process that can result in pain, swelling, warmth, redness and stiffness. Sometimes inflammation can also affect the bowel. When it does that process is called inflammatory bowel disease . IBD is actually two separate diseases: Crohn’s disease and ulcerative colitis.
Routine Screening To The Rescue
When the physician turned 60, he scheduled a colonoscopy, a recommended test to screen asymptomatic individuals over 50 for colon cancer. He had one at 50 it was completely normal. When it was time for his next exam, the doctor who did it the first time had retired, so he asked a friend, Dr. Erick Chan, a gastroenterologist, to perform the test.
He was still a little foggy from the anesthesia when Chan came by with what the physician assumed would be the usual report of normal results. He was wrong. I took some biopsies, and well wait to see what they show, Chan said. But I have to tell you, it didnt look normal. The test had been routine until Chan got close to the spot where the colon and the small intestine connect, a structure known as the ileocecal valve. Chan noticed that the valve looked a little asymmetric.
As Chan advanced his scope, he could see that the valve was distorted by scar tissue so much so that the connection was too narrow for his instrument to enter. Bringing his scope as close to the opening as he could, he saw that the tissue on the other side was an angry red and dotted with ulcers. They would have to wait for the biopsies to come back, but Chan suspected Crohns disease. Thats impossible, the man responded. He had no G.I. symptoms at all. No pain, no diarrhea, no blood in his stools. How could he possibly have Crohns?
You May Like: Food Not Good For Stomach Ulcer
What Your Physician Isnt Telling You And What They Dont Know
Diagnosing tight hip flexors is tricky.
If youve seen a therapist or physician, chances are they werent able to pinpoint the issue.
Buried so deep within your abdomen, its no wonder identifying it as the root cause of any of your symptoms is difficult to do.
Its why tight hip flexors are left undiagnosed and untreated for far too long, as physicians look for a simpler explanation.
So understand that this its not your fault.
However, knowing this hands you the power to finally do something about it before its too late.
How Is Ulcerative Colitis Treated
Theres no cure for ulcerative colitis, but treatments can calm the inflammation, help you feel better and get you back to your daily activities. Treatment also depends on the severity and the individual, so treatment depends on each persons needs. Usually, healthcare providers manage the disease with medications. If your tests reveal infections that are causing problems, your healthcare provider will treat those underlying conditions and see if that helps.
The goal of medication is to induce and maintain remission, and to improve the quality of life for people with ulcerative colitis. Healthcare providers use several types of medications to calm inflammation in your large intestine. Reducing the swelling and irritation lets the tissue heal. It can also relieve your symptoms so you have less pain and less diarrhea. For children, teenagers and adults, your provider may recommend:
Children and young teenagers are prescribed the same medications. In addition to medications, some doctors also recommend that children take vitamins to get the nutrients they need for health and growth that they may not have gotten through food due to the effects of the disease on the bowel. Ask your healthcare provider for specific advice about the need for vitamin supplementation for your child.
You might need surgery that removes your colon and rectum to:
- Avoid medication side effects.
- Prevent or treat colon cancer .
- Eliminate life-threatening complications such as bleeding.
Don’t Miss: Best Supplements For Ulcerative Colitis
Diagnosing Back Pain In Ulcerative Colitis
Diagnosing back pain as a symptom of ulcerative colitis can be tricky. Back pain can be attributed to a number of causes, including injury and strain. Because of the other potential causes, some people may not think to mention their backaches when seeking care for their UC. Whats more, back pain may develop years before UC does, making it more challenging to note the connection between the two.
If your doctor suspects that your UC has led to axial arthritis or ankylosing spondylitis, they will likely ask you to come in for a physical exam and tests. During this exam, they may test the range of motion in your spine and gauge your ability to take a deep breath. The doctor may also try to pinpoint the location of your pain by moving your legs or pressing on certain areas of your pelvis.
Radiographic tests are also commonly used to diagnose axial spondyloarthritis. Your doctor may use an X-ray to check for damage to your bones or joints. If no inflammatory damage is visible on the X-ray, your doctor may also order an MRI scan to get a more detailed view of your soft tissue and bones. An MRI scan can be particularly helpful, as it can allow doctors to catch and start treating your axial arthritis or AS before damage becomes extensive.
Complementary And Alternative Remedies
Alternative treatments such as acupuncture may help reduce and regulate bowel inflammation, reducing UC pain.
Another form of alternative treatment called moxibustion may also have a positive effect on UC symptoms. Moxibustion is a type of heat therapy. It uses dried plant materials burned in a tube to warm the skin, often in the same areas targeted by acupuncture.
Don’t Miss: What Does A Colon Ulcer Feel Like
Ulcerative Colitis And Joint Pain
When you have ulcerative colitis , its normal to have pain in your abdomen, along with diarrhea and other gastrointestinal symptoms.
Up to 30 percent of people with UC also have arthritis, which is characterized by swollen, painful joints.
Heres a look at the connection between UC and joint pain, as well as what you can do to protect your joints if you have UC.
Trying Just About Anything
The acute pain went away after a few days, but the old pain, the usual pain, came and went with depressing regularity. Ibuprofen or naproxen helped but irritated his stomach. His primary-care doctor put him on Celebrex, which is easier on the gut. The medications, along with a cushion that he now had to carry with him everywhere, got him through the worst of the attacks. Every now and then, he would try a new specialist to see if anyone had anything new to offer. He saw a physical-medicine doctor, a neurologist, a pain specialist and finally an integrative-medicine doctor. They ordered imaging, physical therapy, massage therapy, injections, pills. He stopped his statin. He started yoga. Nothing really seemed to help much. So he stuck with his Celebrex and his cushion and his regular trips to the gym. He wasnt getting better, but he wasnt any worse either. The nighttime attacks of terrible pain were thankfully rare.
The doctor suffered for nearly a decade. Finally he found an answer and a treatment. But it didnt come through any of the experts he saw for his pain.
You May Like: How To Heal Stage 4 Pressure Ulcer
Believe It Or Not This Digestive Disorder Can Wreak Havoc On Your Elbowsand Knees Too We Asked The Experts For The Bottom Line
by Health Writer
Bowel inflammation may be the main characteristic of , but joint pain is far more common than many people realize. According to the Crohns and Colitis Foundation, as many as 30% of people with UC and Crohn’s disease may also experience . Most of the time, UC causes joints to feel stiff without inflammation, but other times you may also experience inflammatory arthritis that includes swelling in areas where two bones join, such as your knees, elbows, or wrists. Arthritis that is associated with UC doesnt just target your large joints in your arms and legs, thoughit can also affect your spine.
The good news? Joint pain usually disappears once the inflammation in your colon is treated. Still, it can seem a bit confusing to be experiencing joint aches when youve been diagnosed with a gastrointestinal disorder. How does it all relate? We asked the experts to break down the ways ulcerative colitis and joint pain are related.
Predictors For Impaired Muscle Strength And Poorer Physical Performance
Multivariate binary logistic regression results evaluating predictors for decreased muscle strength and impaired physical performance can be found in . In this analysis, in the total population of UC patients and controls, having the diagnosis of UC was independently associated with a decreased QS and a slower ST. No factor was independently associated with decreased HGS and HPA was found to be protective against an impaired GS.
Also Check: How To Treat Bleeding Ulcer In Stomach
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Reducing Your Arthritis Risk When You Have Ulcerative Colitis

Arthritis is the most common complication outside the gut for people with ulcerative colitis. These dos and donts will help you protect your joints.
As if gut pain from ulcerative colitis werent enough, as many as 30 percent of people with an inflammatory bowel disease , including ulcerative colitis, will develop problems with their joints, according to the Crohns and Colitis Foundation. Indeed, arthritis is the most common complication that occurs beyond the intestines.
Although its not fully understood, there seems to be a link between the gut and joints, says Harry D. Fischer, MD, the chief of rheumatology at Lenox Hill Hospital in New York City. For example, a bacterial infection in the digestive tract can cause a reactive type of arthritis, he notes. In addition, both arthritis and ulcerative colitis have a genetic component.
According to the Crohns and Colitis Foundation, people with ulcerative colitis tend to have one of three forms of arthritis:
- Peripheral arthritis , which affects large joints such as the knees, ankles, elbows, or wrists when IBD is properly treated and controlled, PA joint pain and symptoms typically improve
- Axial arthritis, which causes pain and stiffness in the spine and lower back
- Ankylosing spondylitis, a more severe type of arthritis that affects the spine and can lead to joint damage. Its an uncommon complication that affects between 2 and 3 percent of people with IBD.
Read Also: Is Oatmeal Good For Ulcerative Colitis
Research And New Developments
Previous research has shown that ankylosing spondylitis has a strong genetic component and were currently funding several research projects to further understand this. Previously, we part funded research that identified a specific gene, called IL23R, thats linked to the condition. Were now funding a follow-on project to investigate how changes in this gene lead to the development of ankylosing spondylitis.
Were also supporting a study thats investigating a gene called RUNX3. Researchers are investigating whether this molecule can be targeted with drugs. Results from this research may lead to the development of new and more effective drug treatments.
Were funding a project investigating the protein HLA-B27. This protein is found in over 90% of people with ankylosing spondylitis. Its thought that HLA-B27 proteins tend to fold incorrectly inside cells, which may lead to the immune system releasing chemicals that cause inflammation. This research aims to generate HLA-B27 specific treatments that overcome the problems associated with current treatment options.
Treating Back Pain In Ulcerative Colitis
Treating back pain in ulcerative colitis can be complicated. Research shows that treating the underlying UC can help lessen the severity of spondyloarthritis, but it will not resolve spondyloarthritis and back pain. Back pain must be addressed separately and in a way that does not make a persons UC symptoms worse.
People with ulcerative colitis may need to work with both a rheumatologist and a gastroenterologist to manage their gastrointestinal and spinal health properly. These doctors may prescribe or recommend the following treatments and therapies.
Don’t Miss: Best Fruits For Ulcerative Colitis
Ulcerative Colitis Symptoms You Should Never Ignore
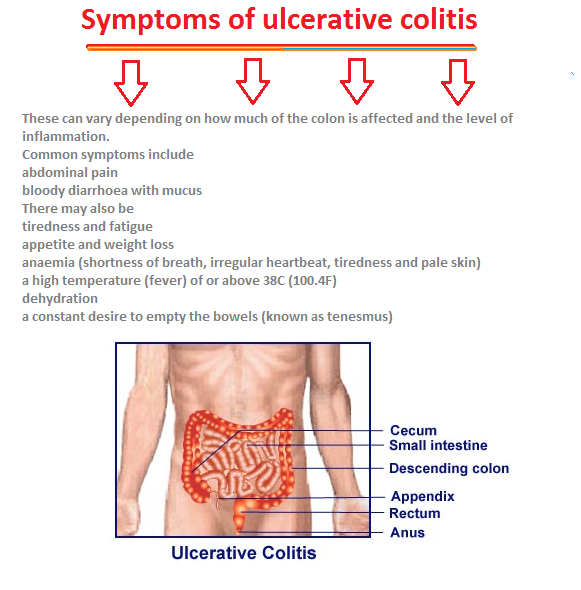
Ulcerative colitis is an autoimmune disease in which the immune system attacks the colon and causes a range of symptoms, both in the GI tract and around the body.
Symptoms of ulcerative colitis, a type of inflammatory bowel disease , can vary widely depending on how much inflammation a person has and where the inflammation is located.
Abdominal pain and bloody diarrhea are the most common warning signs of UC, and can range from mild and intermittent to severe and chronic. The pain of UC is quite common and can significantly impact quality of life. Ulcerative colitis symptoms tend to come and go, often with extended periods of time in between flares. These are called remission periods.
The disease tends to develop gradually over time, so you might not automatically think of ulcerative colitis or IBD if you have occasional abdominal pain or digestive distress.
Ongoing inflammation along with ulcers and abscesses in the intestines are additional common causes of pain. Scarring in the lining of the intestinal tract can lead to painful obstructions. Pain may occur in different areas such as the abdomen or rectal area, depending where the inflammation is located. For example, people may experience moderate to severe pain on the left side of the abdomen if the UC affects the rectum and the lower segment of colon.
UC symptoms might ebb and flow, but they wont go away unless you see a gastroenterologist and start treatment.
Sex Pregnancy And Ankylosing Spondylitis
Sex may be painful if you have ankylosing spondylitis. If it is, try taking some painkillers beforehand and experiment with different positions.
Ankylosing spondylitis can make you feel tired, so its important your partner understands how your condition affects you. Good communication can help you maintain an active sex life and counselling can sometimes benefit both partners.
Its fine to use the contraceptive pill if you have ankylosing spondylitis, but you should tell your doctor youre taking it.
If youre thinking of starting a family, its very important for both men and women with ankylosing spondylitis to discuss medication with a doctor beforehand.
Some drugs such as methotrexate should be stopped several months before a woman tries to get pregnant. Latest research suggests its safe for men to take methotrexate when trying for a baby with their partner.
Biological therapies seem to be safe in the earlier stages of pregnancy but are then stopped later in pregnancy.
If you become pregnant while using a conventional DMARD such as methotrexate or a biological therapy, discuss this with your rheumatology team as soon as possible.
Usually, pregnancy doesnt cause any special problems for the mother or baby, though the symptoms of ankylosing spondylitis may not ease during pregnancy. If your spine is very stiff, it may not be possible to have an epidural during childbirth. This is an injection into the back that stops people feeling pain in part of the body.
Don’t Miss: How Do I Know If I Have A Peptic Ulcer
To Treat Or Not To Treat
Because Crohns is usually painful and is associated with complications including bowel perforation, anemia and malnutrition, patients are usually treated with medications to calm down the immune system and reduce the inflammation. These are powerful drugs that suppress the immune system. They are very effective at controlling the pain and destruction but can leave a patient open to infection. Because of that, its less clear how to treat patients with asymptomatic disease. For those with no pain and no signs of inflammation, watchful waiting is a common strategy.
The same type of medications are used to treat the arthritis associated with inflammatory bowel disease. The physician wasnt sure if it made sense for him to use an immune-suppressing medicine while seeing sick patients. His rheumatologist, seeing him put the pad on his seat before gently lowering himself onto the chair, was much less uncertain. She had put many people on these medications, she told him some of them doctors. Most did fine. He agreed to start taking it. The effect was immediate and amazing. His pain a regular visitor for nearly a decade is gone. Even at the end of the day, his walk to and from his car is painless. He still uses the pad at times those bones are still a little tender. But the rest of him feels great.