When Symptoms Get Severe
In some cases, UC can in some cases cause life-threatening complications including severe bleeding, perforated colon, and severe dehydration. If any of these conditions are present, its a medical emergency and the person should get immediate medical attention. UC can also cause an increased risk of colon cancer and blood clots in the veins and arteries.
Things No One Tells You About Life With Ulcerative Colitis
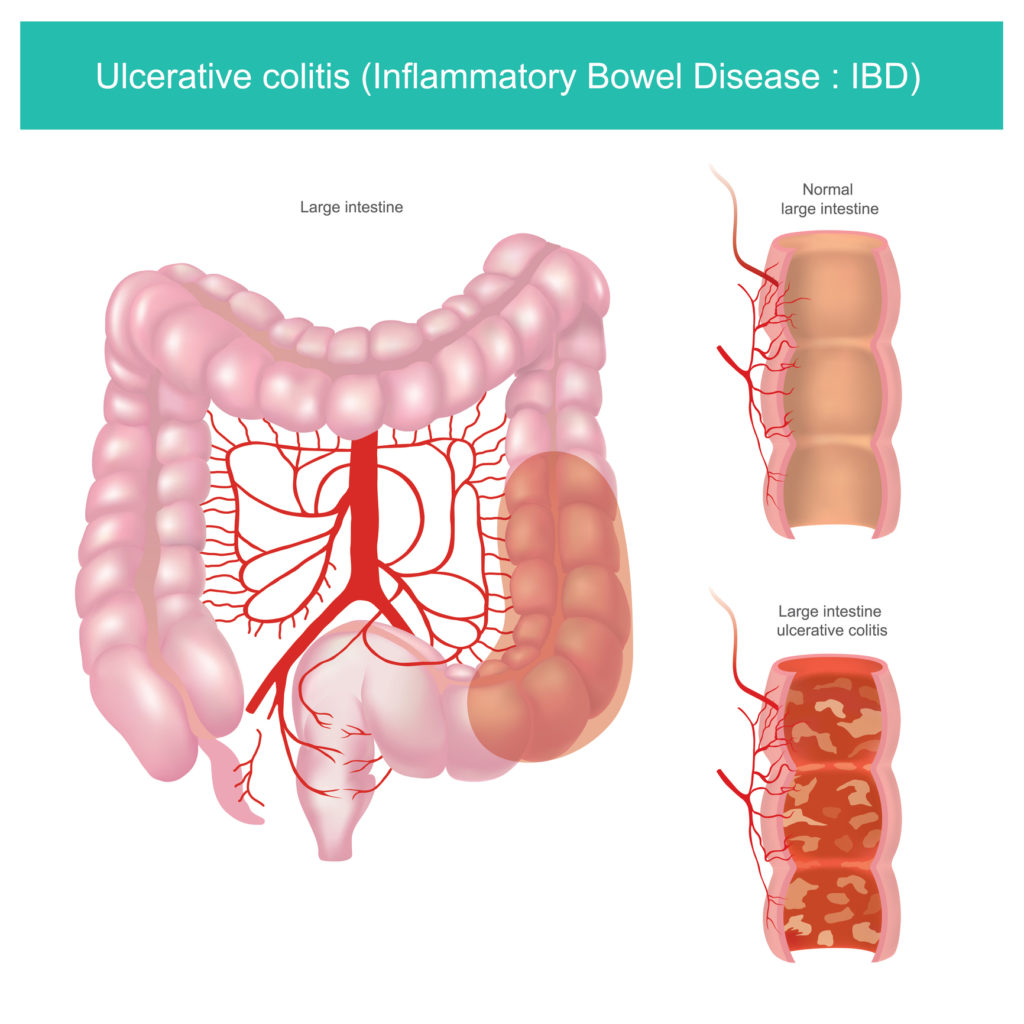
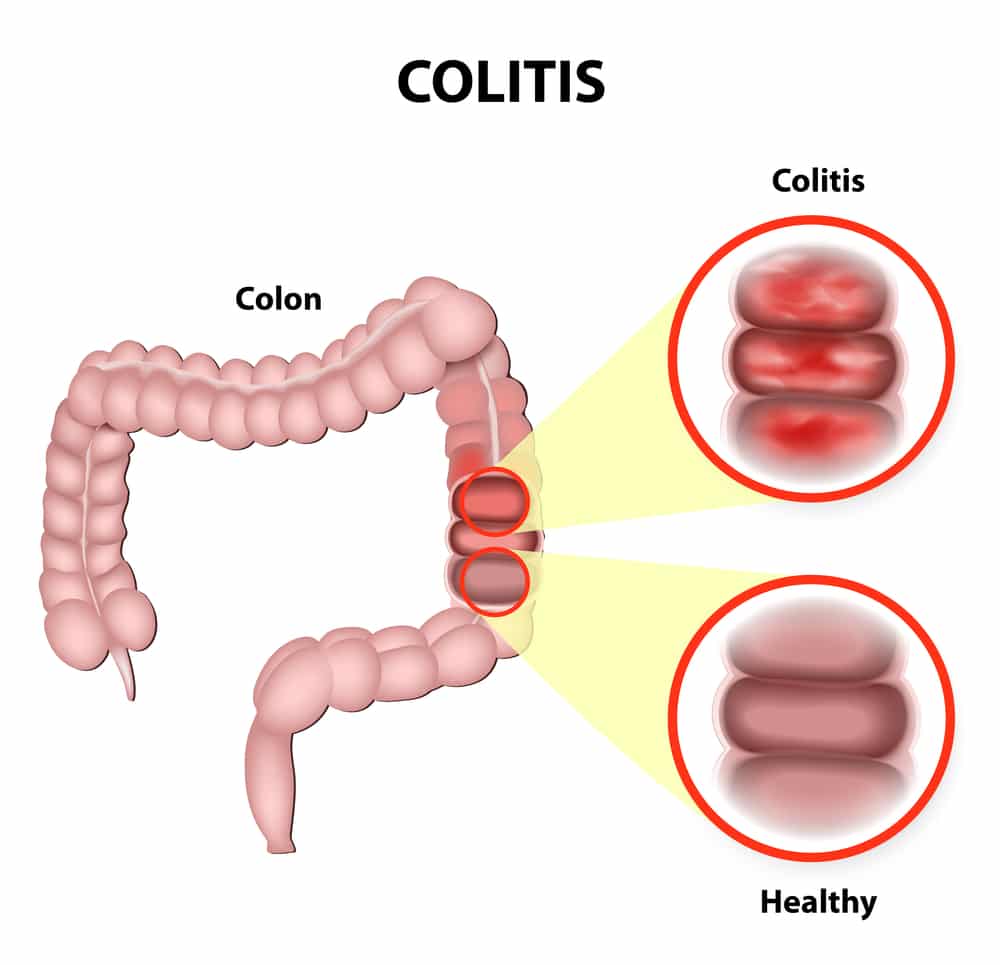
People who have never experienced ulcerative colitis may think it means getting the occasional bad stomachache or having a fussy gastrointestinal system. But as anyone with ulcerative colitis knows, the effects of this inflammatory bowel diseasein which sections of the large intestine develop inflammation and ulcerscan be severe and disrupt many aspects of your life. After a diagnosis of ulcerative colitis, it can be incredibly hard to navigate the reality of your new normal. Knowing the following seven facts about life with ulcerative colitis might help make the whole experience a little bit easier.
Stomach Pain After Eating Here Are 7 Things It Could Be
Home> Manhattan Gastroenterology Blog> Stomach Pain After Eating? Here Are 7 Things It Could Be
Recurring stomach pain after eating is not good and maybe a sign of chronic indigestion or an underlying medical condition that needs to be checked by a specialist. Gas, bloating, nausea, and abdominal pain can affect your routine life and eating habits to a large extent. The gastrointestinal specialists at Manhattan Gastroenterology use the latest technological advancements to find out what may be wrong with your digestive system and come up with the best treatment options for your specific symptoms. The top-rated gastro doctors diagnose and treat your ailment, provide quick relief to protect your gastrointestinal health, and help you feel better in the shortest possible time.
Stomach pain or gastrointestinal discomfort after eating a meal is not dangerous if you know what is causing it and subsides on its own. Most people report bloating, a swollen stomach, feeling full quickly, and diarrhea, which is quite normal if it is happening from overeating, consuming something undercooked, or contaminated. However, if you continue to experience ongoing discomfort despite making lifestyle and dietary changes, it may be some medical issue that needs to be checked.
Recommended Reading: Can You Get An Ulcer In Your Colon
Are Nutritional Needs Different For People With Ibd What Are The Specific Nutritional Needs For People With Crohn’s Disease And Ulcerative Colitis
Nutritional needs are specific to the individual and differ with disease state, body size and age. A nutritionist can help you estimate your individual needs. Calorie and protein needs are similar for Crohn’s disease and ulcerative colitis. In both diseases, needs increase during inflammation and immediately after to restore losses. The following are general statements about nutritional needs that may apply to you.
To Avoid: High Fiber Foods
Foods that are high in fiber might be a challenge during an IBD flare-up. Most Americans dont get enough fiber and need to eat more. During an IBD flare-up, however, fiber might not be tolerated well. High fiber foods include brown rice, wild rice, popcorn, barley, oats, and anything made with whole wheat. These foods could be added back into the diet when a flare-up is over but might need to be excluded for a time while a flare-up is going on.
Recommended Reading: Ulcerative Colitis And Lactose Intolerance
Recommended Reading: Ulcerative Colitis When To Go To Er
How Often Do I Need A Colonoscopy
Especially when you have symptoms or are just starting or changing medications, your doctor may want to periodically look at the inside of the rectum and colon to make sure the treatments are working and the lining is healing. How often this is needed is different for each person.
Ulcerative colitis also increases your chance of developing colon cancer. To look for early cancer signs, your healthcare provider may have you come in for a colonoscopy every one to three years.
Breast Lung Abdomen Colon Pancreas Gallbladder
These types of cancers can metastasize to the spine and cause back pain. Also with abdominal cancers, pancreatic and gallbladder cancers, you can get the referred visceral pain even before they metastasize, says Dr. Crooks. When cancers do spread to the spine, you can have severe spinal pain.
Depending on the type of cancer, treatments like intrathecal pain pumps can deliver medicine like an anesthetic, nerve pain medicine, or a narcotic in small doses straight to the spine without negative effects like tolerance, addiction, and overdose. Stimulation to the spinal nerve root and spinal blocks are also effective treatments for spinal pain.
Wheres the pain? Depending on the type of cancer, back pain can be in the upper, mid, or lower spine
What are the other possible symptoms? Fatigue that doesnt improve with rest, unexplained weight loss or gain, loss of appetite, nausea, vomiting, swelling or lumps, skin changes, hoarseness, persistent cough, change in bowel habits, vision or hearing problems, headache, and others
What does it feel like? Back pain can range from mild to severe depending on the type of cancer and location and may not respond to OTC pain relievers
While your primary care doctor or specialist helps keep your medical issue in check, a pain specialist can improve chronic musculoskeletal pain that stems from inflammation and overstimulated nerves that can occur when you have one of these conditions.
Recommended Reading: Ulcers In The Legs Or Feet
Do I Need To Be Screened For Colon Cancer
Yes. Everyone needs to be screened for colon cancer beginning at 50 years old. But if you have IBD, your risk of colon cancer is higher. You might need to be screened at a younger age or more often than people without IBD.
- Talk to your doctor about when to begin colon cancer screening, what tests to get, and how often to have them.
- Your doctor’s suggestions will depend on your family health history, how long you have had IBD, whether your colon is affected by your IBD, and how severe it is.
- If you have had IBD for 8 to 10 years, your doctor may recommend a colonoscopy with biopsies every 1 to 2 years. This test checks for early warning signs of cancer.
When Does Cramping Usually Happen
UC cramps can be exacerbated by food, so many people notice cramping after eating or before a bowel movement, says Ha. Cramping can also be tied to eating trigger foods, which often include high-fiber fruits and veggies, lactose, nonabsorbable sugars, high-fat or sugary foods, alcohol, and caffeine.
The hormone fluctuations that occur during a womans menstrual cycle may also trigger UC cramping, according to a study published in January 2018 in Inflammatory Bowel Diseases.
Cramping can occur at all times and throughout the night. Medication and other treatments can help reduce symptoms.
Don’t Miss: What Not To Eat When You Have Ulcerative Colitis
How Is Acute Bacterial Dysentery Differentiated From Acute Onset Of Ischemic Colitis
The degree of bloody diarrhea is variable in patients with ischemic colitis, and it may be difficult to distinguish between the two diseases. Clinically, the patient with ischemic colitis complains of sudden-onset abdominal pain, and an acute abdominal series may show thumbprinting of the colonic mucosa.
Flexible sigmoidoscopy is the mainstay of diagnosis for ischemic colitis. The rectum is usually spared because of its collateral blood flow. Above the rectum, the mucosa becomes friable and edematous, and there may be hemorrhagic areas and ulcerations resembling those of Crohns disease. Angiography is not generally helpful in the evaluation of ischemic colitis ischemic colitis is a small-vessel disease compared with mesenteric midgut ischemia of the small bowel, which involves thrombosis or embolism in the superior mesenteric artery . A barium enema is contraindicated in patients with suspected ischemic colitis, because colonic expansion during barium instillation may promote further ischemia.
Glenn T. Furuta, in, 2004
Stock Up On Nutritious Convenient Foods
People experiencing a UC flare may eat unhealthy junk foods for convenience rather than seeking out healthier alternatives.
Stocking cupboards and the refrigerator with quick, nutritious foods that are enjoyable can help people make food choices that are better for their health and prevent them from snacking on nonnutritious foods.
Read Also: Early Stage Venous Leg Ulcer
You May Like: Ulcerative Colitis And Alcohol Mayo Clinic
Inflammatory Bowel Disease And Colitis
Ulcerative colitis and Crohns disease are the two types of inflammatory bowel disease that cause colitis. Crohns disease and ulcerative colitis are considered autoimmune diseases .
- Ulcerative colitis always begins in the rectum and may spread to the rest of the rest of the colon, spreading from the rectum to the sigmoid, descending, transverse, and finally the ascending colon and cecum in that order. Ulcerative colitis is considered an autoimmune disease, and symptoms include abdominal pain, and bloody, diarrheal bowel movements.
- Crohns disease may occur anywhere in the gastrointestinal tract , including the esophagus, stomach, small intestine, and colon. In Crohns disease, there may be skip lesions, that is, abnormal segments of the GI tract interspersed with normal segments.
Both Crohns disease and ulcerative colitis may have other organ systems involved in addition to the gastrointestinal tract.
Either collagen or lymphocytes infiltrate into the layers of the wall of the colon, presumably as a result of inflammation. This is an uncommon illness and maybe an autoimmune disease. Diarrhea often is watery, and no blood is present in the stool.
Avoid Your Problem Foods
There is no rule for which foods can be a problem. How you feel after eating them is the best guide. You may need to avoid high-fiber foods and foods which are hard to digest. These can include fresh fruits and vegetables. High-fat foods, such as whole-milk dairy products and red meat, may also worsen symptoms.
Write down what you eat and how it affects you. If one kind of food often gives you trouble, stay away from it. Also note the foods that work well for you. Your doctor may have you see a nutritionist to come up with the best food choices for you. A nutritionist can help ensure that you eat foods that are safe while getting proper nourishment.
You May Like: Signs Of Having A Stomach Ulcer
How To Treat Ulcerative Colitis Pain
While there isnt a cure for ulcerative colitis yet, there are ways to treat the inflammation and discomfort. In most UC cases the pain is at its worst during a flare-up, and some peeps are completely pain-free outside of these times. Pain treatment involves a mix of reducing the risk of painful flare-ups and the discomfort experienced during them.
Some treatments are medical interventions, while others are lifestyle and self-management techniques. Here are some effective options:
Can You Gain Weight With Colitis
The best way to gain weight with colitis is to eat a balanced diet of carbohydrates, proteins and fats and to consume more calories than you have been eating. If your disease comes under control, there will be less fear of eating, and you should be able to put the weight back on.
Similarly, you may ask, how can I lose weight with colitis?
If you lose weight because of your ulcerative colitis, try to eat five or six small meals and snacks during the day instead of two or three large meals. When you have chronic diarrhea, drink plenty of water or other fluids to stay hydrated. A dietitian can make a plan diet that meets your calorie and nutrient needs.
One may also ask, why am I gaining weight with Crohns? The inflammation linked to Crohns can give you nausea and diarrhea, as well as curb your appetite. As a result, you may eat less, making it harder to keep weight on. Some Crohns medicines may also affect your weight. Corticosteroids such as prednisone can cause temporary weight gain.
Also Know, what is the life expectancy of someone with ulcerative colitis?
Most people with this condition can have a full life expectancy. However, complications can increase the risk of an early death , according to one 2003 Danish study. Very severe ulcerative colitis could impact your life expectancy, especially within the first couple of years after your diagnosis.
Which is worse colitis or Crohns?
You May Like Also
Recommended Reading: Colon Cancer Symptoms Vs Ulcerative Colitis
Read Also: What Doctor Treats Ulcerative Colitis
Other Ways To Treat Ibd Pain And Cramps
Sometimes, the pain is very difficult to control, even with medication. Your health care provider may suggest therapy or antidepressants in order to help you cope with the unrelenting pain.9
Antidepressants have not been well studied in people with inflammatory bowel disease. Therapy may improve anxiety, depression, and coping skills. However, it does not improve Crohn’s disease or ulcerative colitis.
Nutrition Tips For Inflammatory Bowel Disease
Inflammatory Bowel Disease is a term used for two specific and separate diseases: Crohn’s disease and ulcerative colitis. Nutritional recommendations are different for each disease and for each individual patient. It is important to discuss the treatments that are right for you with a registered dietitian and with your doctor.
You May Like: What Are The Signs And Symptoms Of Ulcerative Colitis
When Should You Call Your Doctor
If youre experiencing certain symptoms, chances are, your current treatment is not working and its time to consider a change in therapy, says Ha. Call your doctor if:
- Cramping is severe
- Youre experiencing a significant amount of abdominal pain that requires medication
- You have a fever that lasts longer than a couple of days
- You experience nausea or vomiting
- You have ongoing diarrhea or blood in your stool
What Is Uc Cramping
Abdominal pain and cramping from UC is most commonly caused by the conditions inflammatory process, according to Christina Ha, MD, a gastroenterologist at Cedars-Sinai Medical Center in Los Angeles. Such inflammation usually starts at the rectum and moves throughout the large colon. The greater the inflammation, the more severe the pain.
You May Like: How Do You Heal A Bleeding Ulcer
This Gastrointestinal Disease Is Known For Its Stabbing Pain And Cramping But An Upset Stomach Is Often Not Far Behind
by Health Writer
If youre dealing with ulcerative colitis , you know all about the desperate sprints to the bathroom and finding yourself doubled over in pain from abdominal cramps. Another symptom thats less discussed? That feeling like you are on a rocky boat in the middle of the ocean, about to lose your lunch. isnt as commonly associate with nausea, but when it hits it can be debilitating.
Like many , nausea can be caused by many things beyond your chronic condition. As such, it take some investigating to be sure that the queasiness you feel is related to your ulcerative colitis and not another cause. We asked the experts for indicators that nausea may be due to this gastrointestinal disease, plus ways to get your gut back on track so you can feel your best.
Can Surgery Affect Nutritional Status
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
You May Like: What Desserts Can I Eat With Ulcerative Colitis
What Are The Most Common Ulcerative Colitis Symptoms
Early ulcerative colitis symptoms usually include things that could easily be overlooked. Dont be afraid to talk to a doctor if youre having any worries though, even if your symptoms seem mild. If symptoms are ongoing and start to feel more severe, like persistent pain in your abdomen or unintentional weight loss, you should seek medical treatment as soon as possible.
Here are some of the most common symptoms of ulcerative colitis to watch out for, per the NIDDK:
Okay, so this isnt the most pleasant one to start with, but it is actually the most common ulcerative colitis symptomits also a pretty good tip-off that something isnt quite right and that you should schedule an appointment with your doctor. Remember those ulcers we talked about earlier? Yeah, thats where the blood in your stool comes from, and you might also see mucus in there as well.
This is another pretty common symptom, and contrary to popular belief, those ulcers in the colon are not actually what causes the pain. Instead, its a combination of abdominal cramping and bowel distension that occurs due to the inflammation in the intestines, according to a 2013 study published in Inflammatory Bowel Diseases.1
With all thats going on in the digestive tract with ulcerative colitis, nausea can sometimes be an issue. This occurs more often when symptoms are severe, or if the inflammation affects more of the large intestine, according to the NIDDK.
What Medicines Treat Ibd
Medicines used to treat IBD help reduce inflammation, relieve symptoms, and prevent future flare-ups. Your doctor may give you:10,15
- Medicines to control inflammation, such as:
- Aminosalicylates, which may also help prevent flare-ups. Most people with mild to moderate ulcerative colitis and some people with Crohn’s disease are treated with aminosalicylates.
- Biologic therapies, which block substances in your body that cause inflammation
- Antibiotics, which may help if you have an infection or overgrowth of bacteria
You may need to try several different medicines before you find what works best for you.
Also Check: How Can Ulcers Be Treated