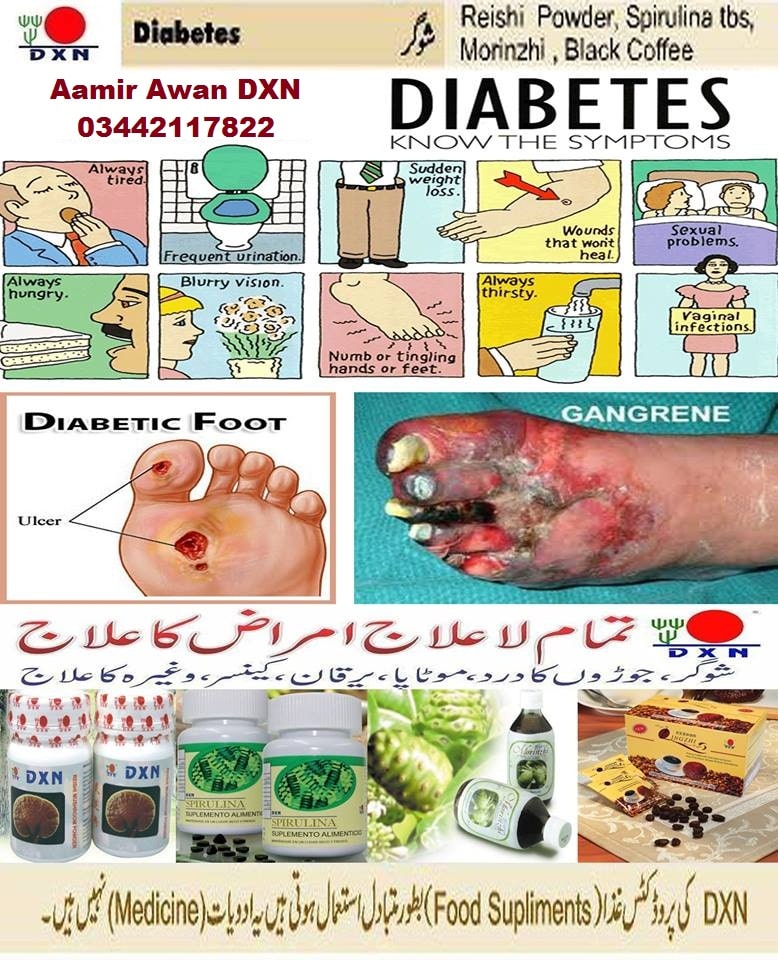
How Do Diabetic Foot Ulcers Form
Ulcers form due to a combination of factors, such as lack of feeling in the foot, poor circulation, foot deformities, irritation , and trauma, as well as duration of diabetes. Patients who have diabetes for many years can develop neuropathy, a reduced or complete lack of ability to feel pain in the feet due to nerve damage caused by elevated blood glucose levels over time. The nerve damage often can occur without pain and one may not even be aware of the problem. Your podiatric physician can test feet for neuropathy with a simple and painless tool called a monofilament.
Etiology Of Foot Ulceration
The etiology of diabetic foot ulcers usually has many components.4,7 A recent multicenter study8 attributed 63 percent of diabetic foot ulcers to the critical triad of peripheral sensory neuropathy, trauma, and deformity. Other factors in ulceration are ischemia, callus formation, and edema. Although infection is rarely implicated in the etiology of diabetic foot ulcers, the ulcers are susceptible to infection once the wound is present. Many of the risk factors for foot ulcer are also predisposing factors for amputation, because ulcers are primary causes leading to amputation.5,7,9 Recognized risk factors for diabetic foot ulceration are listed in Table 1.4
The rightsholder did not grant rights to reproduce this item in electronic media. For the missing item, see the original print version of this publication.
What Causes Diabetic Foot Ulcers
DFUs are commonly caused by high blood sugar, which is also called hyperglycemia. Type one and type two diabetes cause the levels of blood glucose to elevate. The rise in glucose can create a stiffening in the bodys arteries. Narrowing blood vessels are another systematic issue. The two of these symptoms team up in a villainous manner by restricting the blood and oxygen flow to support the bodys ability to heal itself naturally.
Another cause may be circulation problems. People with diabetes are at substantial risk for peripheral arterial disease . PAD hinders the blood from flowing properly to the legs and the feet. If a chronic wound, especially a DFU, is present, it is a hindrance to the bodys ability to heal naturally as well. If PAD is untreated, it can be the cause of amputation.
Uncontrolled glucose levels can easily lead to nerve damage. Diabetic neuropathy is a condition that is in a group of nerve diseases that cause sensation loss, therefore the ability to feel pain is greatly diminished . If a diabetes patient suffering from neuropathy somehow cuts their foot, or has a blister or surgical incision, the pain from the wound may not be felt. This can lead to wound neglect, which could result in infection and create a stubborn DFU that is slow to recover.
Don’t Miss: Can You Eat Tomatoes With Ulcerative Colitis
Proper Dressing Infection Control And Offloading
Its essential to use the proper types of wound dressing, infection control, and offloading to prevent your diabetic wound from regressing during or after treatment.
The best wound dressing maintains a healthy amount of moisture on the foot to create a favorable environment for the wound. It must be changed at least once or twice per day, depending on the stage and severity of the ulcer. Wound dressing helps control infection, as do antibiotics.
Offloading is also a very important but often overlooked component of diabetic foot ulcer treatment. When you offload, you remove pressure from your injured foot and give new, healthy cells the opportunity to thrive. Crushes, knee scooters, and wheelchairs all accomplish offloading.
How Is Gastroparesis Treated
Gastroparesis is a chronic condition. This means that treatment usually doesnt cure the disease, but you can manage it and keep it under control. People who have diabetes should try to control their blood glucose levels to reduce the problems of gastroparesis.
Some people may benefit from medications, including:
- Reglan: You take this drug before you eat, and it causes your stomach muscles to contract to help move food out of your stomach. Reglan also helps cut down on vomiting and nausea. Side effects include diarrhea and, rarely, a serious neurological disorder.
- Erythromycin: This is an antibiotic that also causes stomach contractions and helps move food out. Side effects include diarrhea and development of resistant bacteria from taking the antibiotic for a long time.
- Antiemetics: These are drugs that help control nausea.
Surgery for gastroparesis
People with gastroparesis who still have nausea and vomiting even after taking medications may benefit from surgery. One type of surgery for gastroparesis is gastric electrical stimulation, which is a treatment that sends mild electric shocks to your stomach muscles. In this procedure, your provider inserts a small device called a gastric stimulator into your abdomen. The stimulator has two leads that are attached to your stomach and provide mild electric shocks, which help control vomiting. Your provider can adjust the strength of the electric shocks. The device runs on a battery that lasts up to 10 years.
You May Like: Can Ulcers Heal On Their Own
Custom Orthotics And Braces
To relieve pressure from an ulcer and help it heal, NYU Langone doctors can provide custom-fit orthotic shoe inserts or braces.
Orthotics, or shoe inserts, help redistribute the weight of your body across the bones and joints of your foot while you walk. These inserts are firm but soft and may contain foam or gel to support your foot and make walking more comfortable.
Our doctors can create inserts with soft, donut-shaped padding to surround and support an ulcer. This helps relieve pressure and protect the ulcer from friction when you wear shoes. A custom shoe insert can also shift weight away from the area of the injury to further relieve pressure and help the ulcer heal.
If your doctor recommends taking more weight off of the affected foot, he or she can provide a custom-fit brace that is worn over the foot and leg. There are many types of braces. One version, called a patellar tendon bearing brace, shifts the weight of the body off of the affected part of the foot and onto the strong tendon in the front of the knee, called the patellar tendon.
Our diabetic foot specialists take a mold of your foot to ensure that the custom orthotic insert or brace fits you well and is comfortable. It takes about two weeks for the device to be made, at which time your doctor schedules an appointment to show you how to use it.
Do You Have A Diabetic Foot Ulcer
Your nerve damage and poor circulation may reduce your ability to sense an injury on your foot. The very best way to identify the presence of a diabetic foot ulcer is to perform a visual inspection every day, especially along your heel, the bottom of your big toe, and the ball of your foot.
If you notice any of the following signs, seek medical care immediately:
- Drainage from your foot is staining your socks or leaking from your shoe
- Unusual swelling
- Foul odor from one or both feet
- Black tissue surrounding a wound on the foot
- Extensive callus on base of foot around wound
Responding to the symptoms of a foot ulcer immediately can make the difference between a long, expensive hospital stay and a relatively easy recovery.
Read Also: Foods Safe For Ulcerative Colitis
Treatment For Vascular Ulcers
Its important to note that not all skin ulcers are caused by diabetes, and that even people who dont have diabetes can suffer from chronic wounds. Even people without diabetes can be susceptible to vascular ulcers. Vascular ulcers are caused by problems with the vascular system .
These types of ulcers can happen to people who suffer from veins or arteries that dont function properly, causing blood flow in the legs to be limited. This can lead to an increased risk of wounds that may not heal normally and can become infected.
The Wound Care Center at Harrington also provides full service care for these types of wounds, including on-site X-rays, MRI and lab work.
To make an appointment at the Harrington Wound Care Center, call 248-8105. You can also learn more on our website here.
Treatment Still Requires Regular And Ongoing Foot Self
The best treatment for a foot ulcer, according to the American Podiatric Medical Association, ”is to prevent its development in the first place.” To prevent diabetes-related foot wounds from occurrng, you should have your feet checked at least annually, and more often if you have poor circulation or other symptoms.
Besides seeing your endocrinologist or a podiatrist regularly, you can reduce your risk by assessing your time-in-range and making adjusting to improve your blood sugar control, quiting if you are still smoking, and taking the necessary steps to achieve good blood cholesterol levels.
Ask your podiatrist about the best shoes to wear and how best to inspect your feet to spot problems early.
Dr. Armstrong has no relevant disclosures. Dr. Frykberg received AOTI research funds to conduct the study and has received speaking honoraria. The study was sponsored by AOTI, Inc. which makes the device.
Recommended Reading: Best Dressing For Decubitus Ulcers
Preventing Diabetic Foot Ulcers
There are several ways to prevent a foot ulcer. In addition to daily checks of your feet for any signs of an ulcer or other abnormality, the following can be done to help with prevention:
- Never walk barefoot, and always wear socks to protect your feet
- Wear shoes that fit properly and do not rub
- Keep your blood sugar under control and monitored
- Eat a healthy diet
- Avoid alcohol and tobacco products
- Seek immediate medical attention if you have a foot wound that is not healing
Treatment For Diabetic Foot Ulcers
If a diabetic foot ulcer does occur, its important to seek medical care as soon as possible this is not a wound you should attempt to treat at home on your own. The faster a foot ulcer is properly treated, the greater chance it will heal completely and without infection or complications.
A diabetic wound care specialist, such as the Wound Care Center at Harrington, can provide the most advanced and comprehensive diabetic wound treatment. Your primary care physician can provide a referral to the wound care center. Our Wound Care Center team will then continue working hand-in-hand with your doctor throughout the wound treatment process.
Our specialized diabetic wound treatment services include:
Don’t Miss: Icd 10 Code For Ulcerative Colitis With Bleeding
What Is A Diabetic Foot Ulcer
A diabetic foot ulcer is an open sore or wound that occurs in approximately 15 percent of patients with diabetes, and is commonly located on the bottom of the foot. Of those who develop a foot ulcer, six percent will be hospitalized due to infection or other ulcer-related complication.
Diabetes is the leading cause of nontraumatic lower extremity amputations in the United States, and approximately 14 to 24 percent of patients with diabetes who develop a foot ulcer have an amputation. Research, however, has shown that the development of a foot ulcer is preventable.
Signs And Symptoms Of Diabetic Foot Ulcers

Diabetic Foot Ulcers present with different signs and symptoms. Some of the diabetic foot ulcer symptoms are:
- Changes in skin colour
- Swelling in the foot or ankle
- Pain in the legs
- Open sores on the feet that are draining and slow to heal
- Ingrown toenails or toenails affected with fungus
- Corns or calluses
- Dry cracks in the skin, especially around the heel or other areas of the feet
- Foot odour that is unusual or that will not go away
All of these signs and symptoms may not be present all at once, depending on the severity of the condition.
Recommended Reading: Does Ulcerative Colitis Cause Back Pain
Also Check: Is There A Natural Cure For Ulcerative Colitis
Why Are Foot Ulcers So Common For People With Diabetes
Diabetes interrupts the bodys healing process by restricting its efficiency and slowing its speed. Chronically high blood sugar levels act like a stranglehold to white blood cells and impair their function. Without white blood cells to fight away bacteria, infection can effortlessly take root and spread throughout any wound.
Diabetes is also correlated with poor circulation, which exacerbates an already compromised wound-healing process. Consistently strong circulation is essential to help red blood cells deliver nutrients to the wound. Without strong circulation, diabetic patients become even more vulnerable to infections and ulcers.
Of course, diabetes also causes overwhelming nerve damage. This means that you might not be able to feel or sense the infected, slow-healing wound on your body, even as it causes you significant harm. Since the feet endure so much pressure on a regular basis and often remain trapped in dark, moist shoes and socks, theyre the first place where diabetic ulcers develop.
Praise For Emuaid From Satisfied Customers
We are very thankful for the early arrival of your fine product. My sister, in less than 24 hours, is now completely Pain free. Very, very grateful,*
Dennis L F
I use Emuaid for my skin condition that causes constant itching. Since using Emuaid the itching is completely gone. Its a great product!*
Theresa S.
Emuaid max is a great product that I have bought several times.I am diabetic and it is slow healing but it does help alot*
Anonymous Customer
I am so glad I found this cream to help my husband, in one week I could see a big different. Today we had a Doctor appoinment , she was so surprise how it got better, she took me to the computer to show me the picture from last week and now what a different, I just have to tell her about your cream, she said , she never heard about this cream. I strongly recomend r*
David J
It is the only meds that i have ever found that totally works. the shopping exp, was awesome thanks*
Maggie T.
This stuff is so good. I got the extra strength this time. I am assured that it will work as well or better. Nothing I have tried before worked until I discovered this product. Its a miracle in a jar.*
Paul
Show/Hide all customer reviews +
D. G.
My order came within the promised time and my sore parts were better in 2 days. I cant wait to try it on other skin issues to test its effectiveness. When I talk to my Dr. again I am going to suggest he recommend this to his patients with any skin ailment.*
ElizabethLucyRalphAliceRolandAlbieFred
Recommended Reading: What To Use For Mouth Ulcers
Visit A Doctor Regularly
Theres only one person who can give you special advice on how to best take care of your diabetic foot ulcer. He can give you medicine prescriptions, tips on how to make it better, and even offer to dress it for you. Also, he can notify you of changes and advise you on what to do. Note that though there are a lot of doctors who are an expert in the field of diabetes, only a few dwell so much into this type of condition, so choose your doctor well.
Keeping Your Feet Healthy
Patients with diabetes must be diligent about wound prevention. The first step is properly managing the diabetes itself which includes maintaining a balanced diet and exercise routine, keeping blood glucose levels in the recommended range, avoiding alcohol and tobacco, and addressing any co-occurring disorder such as cardiovascular disease or obesity.
The next step is to commit to daily skin inspections, and especially your feet when sensation is impaired, Estocado said. This inspection should be thorough, and include the sole, sides and in between the toes. Even the smallest blister or scrape can escalate for diabetic patients, so call your doctor at the first discovery of any abnormality.
Don’t Miss: Best Wound Care For Diabetic Foot Ulcer
How Are Foot And Toe Ulcers Diagnosed
Your healthcare provider can tell what type of ulcer you have based on four observations:
- The appearance of the ulcer.
- Location of the ulcer.
- The appearance of the borders.
- The appearance of the surrounding skin.
Your primary healthcare provider can diagnose an ulcer, but they might send you to a specialist for treatment. You might see a podiatrist, a provider who works with feet, or a wound specialist. For more complicated cases that require surgery, you might also see a plastic surgeon, anesthesiologist, orthopedic surgeon and/or vascular surgeon.
What Is The Best Ointment For Diabetic Wounds
Topically applied antibiotics such as Neomycin, Gentamycin, and Mupirocin provide effective antibacterial coverage. Silver-containing dressings are available in various formulations and provide excellent antibacterial coverage. Diabetic foot wounds have been successfully treated with silver dressings and polyherbal formulations .
You May Like: Different Types Of Ulcerative Colitis
Also Check: Signs Of Ulcerative Colitis In Adults
Manage Your Blood Sugar Levels
One of the most important things you can do to treat diabetic ulcers is to keep your blood sugar levels under control by monitoring them on a regular basis.
You can also help treat and prevent high blood sugar levels by following a healthy diet, exercising regularly, and taking any medication prescribed by your doctor.
Who Can Get A Diabetic Foot Ulcer

Anyone who has diabetes can develop a foot ulcer. Native Americans, African Americans, Hispanics and older men are more likely to develop ulcers. People who use insulin are at a higher risk of developing a foot ulcer, as are patients with diabetes-related kidney, eye, and heart disease. Being overweight and using alcohol and tobacco also play a role in the development of foot ulcers.
You May Like: What Are The Signs And Symptoms Of Ulcerative Colitis