Causes Of Diabetic Foot Ulcers
In reality, anyone with diabetes can eventually develop a foot ulcer. An ulcer, being an open wound on the skin, can become worse if not properly treated early as many have to unfortunately amputate their leg because of this. There are people with diabetes that are still living healthy normal lives with a couple of step backs but do not have to go through the pain of an ulcer and there are ways to improve that with good exercise, diet and proper care of your body. Common causes after diabetes include poor circulation, prior disease, poor nerve damage of legs, foot deformities, pressure on feet, and trauma.
Implementation Subgroup And Monitoring Considerations
Topical oxygen therapy supplies continuous or cyclical diffusion of oxygen over the surface of the wound. As this recommendation favours a good standard of care over the intervention in DFU healing, there are no additional considerations for implementation, monitoring and subgroups than those outlined for a good standard of care in earlier wound dressing recommendations .
Visit A Doctor Regularly
Theres only one person who can give you special advice on how to best take care of your diabetic foot ulcer. He can give you medicine prescriptions, tips on how to make it better, and even offer to dress it for you. Also, he can notify you of changes and advise you on what to do. Note that though there are a lot of doctors who are an expert in the field of diabetes, only a few dwell so much into this type of condition, so choose your doctor well.
Also Check: Black Tarry Stools Ulcerative Colitis
You May Like: What Is A Skin Ulcer
What If A Diabetic Foot Ulcer Recurs Even After The Home Treatment
The aforementioned home treatments for diabetic foot ulcers usually work wonderfully. But in some cases, these ulcers tend to reappear again or get aggravated with another flare-up. In such cases, timely medical attention is a must for diabetic foot ulcers. To bring it to your awareness, diabetic foot ulcers can have serious health complications if you leave them untreated for a prolonged time.
So, reach out to a specialist doctor to discuss the treatment options for a diabetic foot ulcer. Depending upon the symptoms, the doctor will recommend the best-suited treatment.
Read Also: How To Treat A Diabetic Ulcer
What Is The Best Ointment For Diabetic Wounds

Topically applied antibiotics such as Neomycin, Gentamycin, and Mupirocin provide effective antibacterial coverage. Silver-containing dressings are available in various formulations and provide excellent antibacterial coverage. Diabetic foot wounds have been successfully treated with silver dressings and polyherbal formulations .
Don’t Miss: Can You Feel A Stomach Ulcer
How To Treat Diabetic Foot Ulcers
November 4, 2016 by Admin2
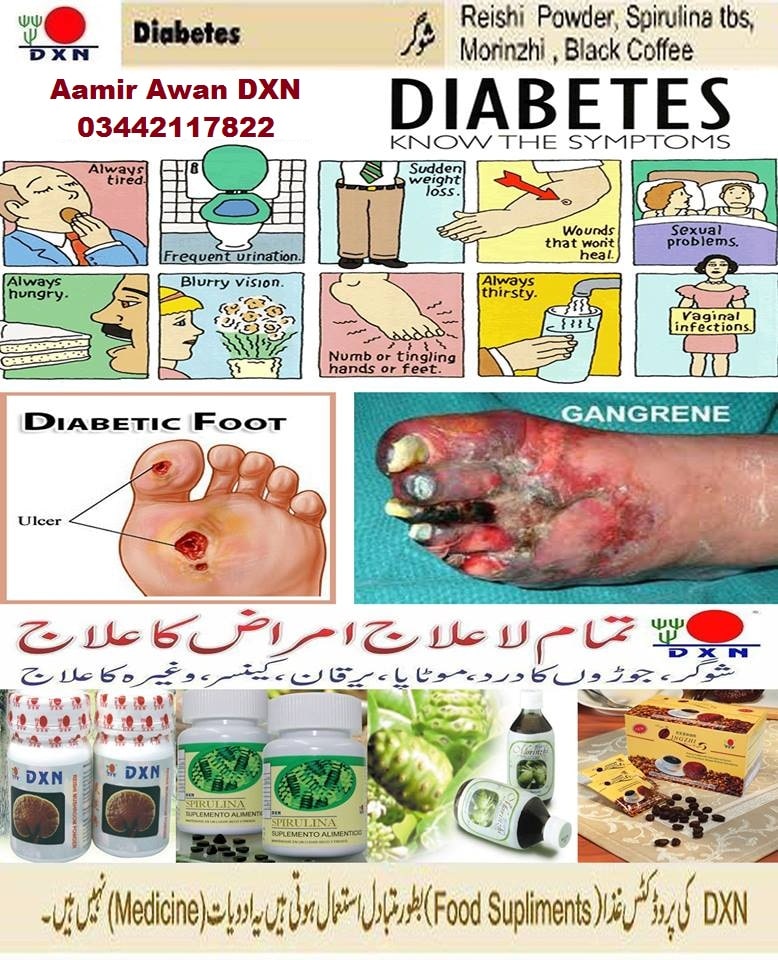
Diabetes is a deadly and life-threatening disease that can bring about unbearable pain and discomforts that are enough to affect the way we live. This includes loss of energy, increased hunger with no appetite, lack of interest and focus, loss of vision, and loss of efficiency for the body to heal wounds. One of the major effects of diabetes is the painful and grotesque wounds that form under your heels. This is called Diabetic foot ulcers and they are serious symptoms of diabetes that can lead to even more complications.
Diabetic foot ulcer is an open wound that occurs under or at the side of your foot and toes. These are painful and can sometimes leak out blood and pus. Diabetic ulcers are formed as a result of changes in the bony shapes of the foot. Other causes are peripheral neuropathy and diseases in the artery. Diabetic foot ulcers can also be caused by wearing tight footwear, rigorous exercises, and getting wounded in the foot.
More than 90% of diabetic patients experience diabetic foot ulcers, and 15% of these patients have been hospitalized due to inflammation and infection. While it is hard to heal diabetic foot ulcers, it is best not to leave them alone for flies and germs to gather around to prevent worsening the condition.
Here are ways you can treat your diabetic foot ulcers:
Implementation Considerations For Recommendations 24
Recommendation 2
In the absence of evidence supporting superiority of one dressing product over another for healing DFUs, dressing selection is paramount as part of a good standard of DFU care. The panel suggests that a good standard of DFU care includes a comprehensive DFU assessment, appropriate debridement, appropriate wound dressings, antimicrobial management if infected, revascularisation considerations if ischaemic and the best available offloading device provided for the patient .
Recommendation 3
Please refer to Recommendation 2 for similar implementation considerations, as well as the panelâs definition of a good standard of wound care for DFU.
Recommendation 4
Read Also: Foods For Acid Reflux And Ulcers
Why Are Diabetics Prone To Foot Ulcers And Other Chronic Wounds
Diabetic patients are more prone to developing chronic wounds for a few reasons. Two of the most influencing factors are nerve damage and blood circulation issues that are common among diabetic patients.
Nerve damage, or neuropathy, tends to occur in patients who have a longer history with diabetes because elevated blood glucose levels damage nerves over time. Neuropathy causes patients to experience reduced, or lack of, sensation in the areas affected.
Many patients can sustain trauma or develop an infection without realizing it because theyre unable to feel pain in the area. Further, neuropathy commonly affects the feet, so a wound on the bottom of the foot can escalate quickly because the patient cannot feel or see the wound easily.
Blood circulation issues also can increase the risk for developing chronic wounds, as well as making the wounds more prone to infection. High blood glucose levels cause the narrowing of blood vessels, which constricts blood supply, Estocado said. Adequate blood supply is essential to normal wound healing. The secondary effect of impaired blood supply is a decrease in white blood cells, which are responsible for fighting infection and maintaining a strong immune system.
Diabetic Wound Healing Products And Supplements
There are many different diabetic wound healing products and supplements you can try to assist with faster wound healing. Remember, before trying any of these options, it is best to discuss their safety and efficacy with your medical health practitioner.
Each one may impact your wounds and your body differently. You and your doctor may want to try each one individually or create a plan that includes multiple options to give you the best results and the fastest healing wounds possible.
Also Check: Best Vitamins For Ulcerative Colitis
Effectively Dressing Diabetic Foot Ulcers
Creating an optimal environment is essential to ensuring rapid healing and preventing complications. However, it can be challenging to effectively dress wounds located on the foot, particularly in cases of deformity or disease such as Charcot foot. To dress these wounds appropriately, health care professionals must often use non-traditional methods. Using best practices and more effective medical adhesive products can allow dressings to stay secure longer, even in unusual locations.2,4
Infection Control Infection in DFUs can lead to inflammation, delayed wound healing, gangrene, and amputation. To reduce the risk of infection and improve outcomes, health care professionals can use dressings that control bacterial load in the wound. Antibacterial agents such metronidazole gel and sisomicin can help control pathogens in the wound area.5
Wound Protection Because DFUs are located on the foot, they are more susceptible to additional injury than wounds in a less exposed location. This makes it important to choose a dressing that provides some amount of mechanical protection. Dressings that are secure and substantial can protect the wound area from additional damage. Using offloading techniques such as total contact casts and removable cast footwear can also help provide support the foot and prevent repetitive trauma.5
Symptoms Of Diabetic Ulcers
Look for signs of bleeding or infection on or around the persons feet. Blood or discharge, an infectious odor, or sections with yellow discoloration can reveal that an infection has taken hold. If any areas have turned black, that indicates gangrene, or tissue death. The same rules apply if the infection is present in a different location, such as the hands, legs, or anywhere on the skin.
Recommended Reading: What To Do If You Have A Stomach Ulcer
How Big Are Foot And Toe Ulcers
There are many different sizes of ulcers. They start as small as 1 centimeter wide and can grow to the size of your entire foot if left untreated.
The depth of the ulcer can change, too. Several different classification systems exist to define the depth of an ulcer. The Wagner Diabetic Foot Ulcer Grade Classification System, for example, has six grades:
- Grade 0: Your skin is intact .
- Grade 1: The ulcer is superficial, which means that the skin is broken but the wound is shallow .
- Grade 2: The ulcer is a deep wound.
- Grade 3: Part of the bone in your foot is visible.
- Grade 4: The forefront of your foot has gangrene .
- Grade 5: The entire foot has gangrene.
Diabetic Foot Ulcer Home Treatment
A diabetic foot ulcer is an open wound that happens due to uncontrolled sugar levels in diabetes patients. It is a troublesome condition that hinders a person from carrying on their daily routines. The worst part about diabetic foot ulcers is that person may not even be aware of its growing seriousness due to the damaged sensation of the affected area.
If you suffer from this problem of a diabetic foot ulcer, here is a sigh of relief for you in the name of home treatments or remedies. Yes, there are things that you can try at home to treat diabetic foot ulcers to some extent.
Also Check: What Is A Stasis Ulcer
Advanced Therapies For Diabetic Foot Ulcers
Physicians of individuals with diabetic foot ulcers may have difficult decisions to make if wounds do not heal. Many of these patients have a significant cardiac risk and health care practitioners need to make complicated decisions about whether to perform invasive procedures like angiography. Other options can be:
- Covering the wound with cultured human cells.
- Heterogenetic dressings or grafts with recombinant growth factors.
- Hyperbaric oxygen therapy.
Wound Care For Diabetic Foot Ulcers
One of the most common problems that diabetics experience is a foot ulcer: about 12-25% of diabetic patients visit a healthcare institution for a foot disorder during their lifetime. A diabetic foot ulcer is an open sore located on the bottom of the foot of a diabetic patient.
One of the most common problems that diabetics experience is a foot ulcer: about 12-25% of diabetic patients visit a healthcare institution for a foot disorder during their lifetime. A diabetic foot ulcer is an open sore located on the bottom of the foot of a diabetic patient.
One of the most common problems that diabetics experience is a foot ulcer: about 12-25% of diabetic patients visit a healthcare institution for a foot disorder during their lifetime. A diabetic foot ulcer is an open sore located on the bottom of the foot of a diabetic patient. It may be caused by too much pressure on one part of the foot and can lead to serious infections and in extreme cases, amputations. Many patients need to be hospitalized due to foot ulcers and need serious wound care for a long time to get better. For a foot ulcer, patients usually get an initial medical assessment from their doctor, who provides immediate medical relief, however to achieve the best outcome usually a multidisciplinary approach is recommended by experts.
Also Check: Home Remedies For Stomach Ulcers During Pregnancy
Research Design And Methods
The data of the present study are derived from a large, prospective multicenter trial that compared a collagen/oxidized regenerated cellulose dressing with moistened gauze in management of diabetic foot ulcers. The methods and results of the study have been reported elsewhere . In brief, the trial was a multicenter study conducted in 11 U.S. sites it was a prospective randomized, controlled trial that was open label with a parallel study design. The study duration was 12 weeks. Patients were eligible for enrollment in the study if they had diabetes and a foot ulcer of at least 30 days duration with an area of at least 1 cm2 . All foot ulcers were uncomplicated by infection or ischemia.
How To Care For Diabetic Foot Ulcers
Here are some tips on how to care for diabetic foot ulcers:
- Keep the wound dry.
- Change the dressing every day.
- Change the dressing when it gets wet or dirty.
- Clean between the toes with a cotton ball each day, using soap and water. This is important for preventing infections between your toes, where it might be hard to see any signs of infection until it becomes very serious and causes deep problems for your feet.
- Keep the bandage dry and clean at all times change out for a clean and fresh dressing as needed .
Don’t Miss: New Biologic Drugs For Ulcerative Colitis
Managing Diabetic Foot Ulcers With Wound Care
In general, managing diabetic foot ulcers involves creating an environment that allows the wound to heal, avoids infection and helps new tissue form. Dressings are essential to this process, although type varies based on the amount of exudate generated. Keeping a wound too moist can hinder the healing process or invite infection.
Cleansing and Dressing Diabetic Foot Ulcers
Start by cleansing the wound with a saline solution. Your doctor will offer recommendations, but typically, patients cleanse their wound once per day on average.
Afterward, youll want to apply an ointment and/or dressing to help heal the wound. This can vary. An antibiotic ointment or wound gel combined with a traditional dressing may be sufficient. However, a more absorbent dressing, like an alginate or foam, may be needed if the injury is deeper or generating a high amount of exudate.
Debriding Diabetic Foot Ulcers
Debridement is the process of removing necrotic tissue and debris from the wound that can impede the healing process and invite bacteria to form. Depending on the wounds severity, this may be done as a mild surgery physically cutting away the dead tissue with a scalpel or scissors.
In other situations, the autolytic method of debridement can be used. Hydrocolloid dressings like Duoderm, transparent films like Bioclusive or hydrogels like Triad may be used in this method. Autolytic debridement is often used as a means to combat the reformation of biofilm after the initial removal.
Diabetic Foot Ulcer Management Strategies
Effective treatment of DFUs starts with physical examination. Patients suspected of having the condition should be examined for signs of clinical presentation. Patients with peripheral vascular disease should immediately receive compression therapy to reduce their risk of developing DFUs. If an ulcer is found, the treatment focus should be on achieving rapid and complete wound healing. The wound should be regularly debrided to keep it free of non-viable tissue, and clinicians should select dressings that reduce bacterial load and provide an optimal healing environment.3
You May Like: Surgical Management Of Ulcerative Colitis Ppt
Recommended Reading: Can I Die From Ulcerative Colitis
Finding The Best Treatment For A Diabetic Foot Ulcer
Youre probably wondering if a person who has no history of diabetes is likely to have a foot ulcer and the answer is yes, its possible. Its important to contact a health professional no matter your current health condition as you do not want symptoms to get worse.
The Wound Institute of America is ready to accept new patients who want to have professional wound care from the number one wound care center in California. To make an appointment with Wound Institute of America or to learn more about your foot ulcer, call 919-4179. You can also learn more about foot ulcers and other wound care treatments on our website here.
Does Peroxide Bubbling Indicate Infection

Although not strictly a error, there is a popular misperception that if hydrogen peroxide bubbles on a cut, it is infectious. Hydrogen peroxide will bubble regardless of whether or not your wound is infected. During cleaning, a chemical reaction produces tiny oxygen bubbles. Dont worry about the bubbles.
Also Check: How To Prevent Ulcers In The Stomach
What Is The Outlook For People With Diabetic Foot
Diabetic foot ulcers are fairly common in people who have had diabetes for a long time. Even with foot checks and careful blood glucose monitoring, some people with diabetes develop infections.
The outlook depends on factors such as:
- How early the wound was found.
- Presence of infection and how much it spreads.
- Treatment effectiveness.
If the infection cant be controlled and spreads too far, amputation may be necessary.
Zinc To Speed Up The Healing
Zinc-rich foods like eggs, nuts, and legumes can prove to be very beneficial for both your diabetes and diabetic foot ulcers. Zinc promotes the production and secretion of insulin in the body and thus helps to keep blood sugar levels in check. Zinc also hastens the healing of the wound by maintaining the structural integrity of the dermal tissue.
Don’t Miss: What Do Diabetic Ulcers On The Feet Look Like
Its Been Longer Than Four Weeks
If wounds dont heal within a month, they are considered chronic wounds. While its possible for chronic wounds to heal on their own, its best to get a doctors help to identify why the wound isnt healing and provide treatment.
Our Wound Healing Center offers advanced treatments for severe and chronic diabetic wounds
Does Walking Help Foot Ulcers
A gradual walking program may protect lower leg muscles and increase plantar tissues stress tolerance and ulcer risk. To present, no randomized controlled research has examined the impact of encouraging weight-bearing physical activity on the risk of foot ulceration in adults with diabetes and peripheral neuropathy.
Also Check: Can Ulcerative Colitis Be Deadly