What Are Venous Ulcers
Venous ulcers are due to high blood pressures in the superficial veins. Leakage of blood under high pressure from the deep veins into the superficial system, particularly in the region of constantly placed perforators over the medial side of the leg, results in venous dilatation, leathery induration, and pigmentation of the skin as a result of stagnation of the circulation and eventually ulceration. A suggestion is that the deposition of fibrin outside the capillose wall and the trapping of white cells in the microcirculation are responsible for impairing the transportation of oxygen and nutrients to the tissues, resulting in the pathological changes found.
Patients with venous veins may have a past history of deep vein thrombosis, and they may have visible varicosities of the superficial system. Also, upon investigation, many patients will show to have had a previous unrecognized deep vein thrombosis or venous hypertension owing to deep vein valve incompetence. Signs of venous ulcers include varicose veins, perforator incompetence, and, lipodermatosclerosis.
Figure 1: Varicose veins are a sign of Venous Ulcers
Signs And Symptoms Of Arterial Ulcers
Typically, arterial ulcers are extremely painful. However, its important to remember that patients who also experience peripheral neuropathy may not feel them at all.
Chronic arterial ulcers look like deep, round hole punches with regular, well-defined, raised borders. The area around the ulcer will feel dry and cold and the skin may be cracked. The pedal pulses will be weak or absent.
Arterial ulcers are mostly located on the toes, between the toes, around the lateral ankle, or on the tibia. Severe late-stage arterial ulcers can present as gangrenous chronic limb ischemia involving the toes.
Chronic arterial ulcers are due to arteries that are slowly blocked over time. These ulcers are usually seen in older adults. The progressive blockage of the arteries decreases blood flow to an area which causes the tissue to die. The pain that is associated with these arterial blockages can be improved by dangling the leg, which increases blood flow to the area.
Figure 2. Arterial ulcers are typically deep with round, regular, and well-defined borders. On ultrasound, you can visualize plaque buildup within an artery that has led to the appearance of a chronic arterial ulcer.
Skin Grafts And Artificial Skin
Two layers of skin created from animal sources as a skin graft has been found to be useful in venous leg ulcers.
Artificial skin, made of collagen and cultured skin cells, is also used to cover venous ulcers and excrete growth factors to help them heal. A systematic review found that bilayer artificial skin with compression bandaging is useful in the healing of venous ulcers when compared to simple dressings.
Recommended Reading: Is Alcohol Bad For Ulcerative Colitis
What Are The Symptoms Of A Diabetic Foot Ulcer
Not all diabetic foot ulcers are symptomatic. Patients that suffer from severe diabetes may not even know that they have a foot ulcer because of various problems with sensation and paresthesias and neuropathy, until it is identified at a follow-up visit or is noticed later on. Presenting symptoms may include pain, a malodour, discoloration, or gangrene, which are usually clear signs of a diabetic foot ulcer.
Caring For Venous Ulcers
Venous ulcers need proper care and treatment to prevent infection and to heal. It’s important to have any venous ulcers checked right away by your healthcare provider.
Treatment may require focusing on the circulatory or vein problems that are causing the ulcers. Or it may mean removing some tissue around the wound. You may be asked to:
-
Clean the wound regularly
-
Apply a dressing to the ulcer
-
Avoid products that cause skin sensitivity
-
Wear compression stockings to prevent blood from pooling in the legs and to speed healing
-
Apply an antibacterial ointment or another topical medicine to prevent or treat an infection
-
Take oral antibiotic medicines to prevent or treat an infection
-
Have allergy testing done
Wearing a compression wrap to keep blood flowing back up to your heart can also help ulcers heal more quickly. In some cases, surgery or a skin graft is needed to close up the opening in the skin.
Recommended Reading: What Does Asacol Do For Ulcerative Colitis
What Is An Ulcer
Ulcers are defined as abnormal breaks in the skin or mucous membranes. This long-lasting sore or wound is typically characterized as slow-healing or non-healing when it has taken more than 5 to 6 weeks to heal. Although leg ulcers can develop anywhere on the leg or foot, they usually develop on the inside of the calf, just above the ankle.
What Are Arterial Ulcers
Skin ischemia, usually in association with atherosclerotic peripheral vascular disease, causes arterial ulcers. Ulceration normally occurs on the toes, dorsum of the foot, anterior tibial area, or heel and appears as patches of dry gangrene. Buergers disease, a disease seen in men aged between 20 and 40 years, may also be associated with skin gangrene. Small vessel vasculitis may also cause ulceration in patients with rheumatoid arthritis and other collagen disorders.
Figure 2: Ulcers
Arterial insufficiency may be evident from a history of intermittent claudication, rest pain, or the presence of ischemic changes of the limb. Presence of the ulcer suggests severe ischemia therefore, local treatment of the ulcer is unlikely to be successful unless arterial supply is restored. Pain relief is necessary because pain can be so severe that the patient needs regular painkillers. Cessation of smoking is essential. The dressing should be simple, and dry gangrene area should be exposed. Loose slough has to be cleaned, and pus drained. Direct arterial surgery and lumbar sympathectomy can help to restore the circulation.
You May Like: How To Ease Stomach Ulcer Pain
Causes Of Venous Ulcers
Venous ulcers most often form around the ankles.
Venous ulcers typically occur because of damage to the valves inside the leg veins. These valves control the blood pressure inside the veins. They allow it to drop when you walk. If the blood pressure inside your leg veins doesn’t fall as you’re walking, the condition is called sustained venous hypertension. That increase in blood pressure causes ulcers to form on your ankles.
Venous ulcers may also be caused by other problems with your leg veins. These include:
-
Varicose veins. These are large, bulging leg veins. They occur when valves in the leg veins dont work well, allowing blood to collect in the lower leg.
-
Chronic venous insufficiency. Like varicose veins, this condition occurs when your leg veins cant pump blood back up to your heart. Blood then pools in your lower legs, causing your legs to swell. Since the blood can’t flow well in your legs, the swelling may be extreme. This extreme swelling can put so much pressure on your skin that venous ulcers form.
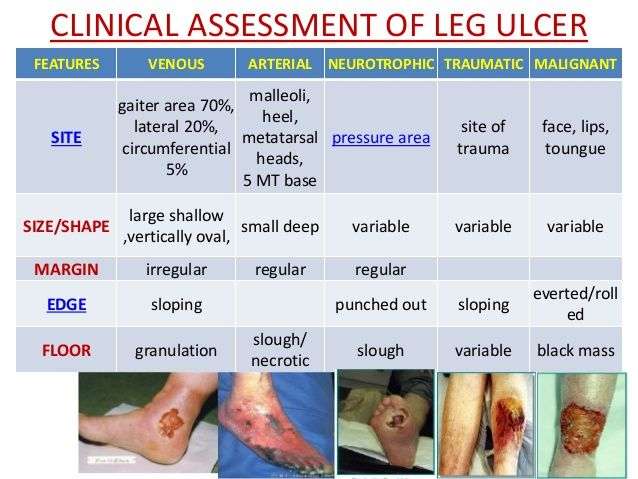
Symptoms Of Arterial Ulcers
Arterial ulcers are characterized by a punched-out look, usually round in shape, with well-defined, even wound margins. Arterial ulcers are often found between or on the tips of the toes, on the heels, on the outer ankle, or where there is pressure from walking or footwear. The wounds themselves are characteristically deep, often extending down to the underlying tendons, and will frequently display no signs of new tissue growth. The base of the wound typically does not bleed, and is yellow, brown, grey or black in color.
Often the limb will feel cool or cold to the touch, and the extremity will have little to no distinguishable pulse. The skin and the nails on the extremity will also appear atrophic, with hair loss on the affected extremity, while also taking on a shiny, thin, dry, and taut appearance. In addition, the base color of the extremity may turn red when dangled and pale when elevated. An additional sign of an arterial ulcer is delayed capillary return in the affected extremity.
These ulcers are generally very painful, especially while exercising, at rest, or during the night. A common source of temporary relief from this pain is dangling the affected legs over the edge of bed, allowing gravity to aid blood flow to the ulcerous region.
Arterial ulcers are distinguishable from venous ulcers in that venous ulcers present with redness and edema at the site of the ulcer, and may be painless.
Figure 1: An ischemic leg ulcer with deep ‘punched out’ appearance
You May Like: What Causes Acute Ulcerative Colitis
What Causes These Ulcers
Poor blood circulation often causes ulcers. When theres reduced blood flow, skin and tissues in the affected areas are deprived of oxygen and nutrients. These areas will become inflamed and form an open wound.
Though ulcers can form anywhere on the body, arterial and venous ulcers are more commonly found on the legs and feet.
Can Leg Ulcers Be Prevented
To prevent and promote healing of ulcers:
- Avoid injury, particularly when pushing a supermarket trolley. Consider protective shin splints.
- Walk and exercise for at least an hour a day to keep the calf muscle pump working properly.
- Lose weight if you are overweight.
- Stop smoking.
- Check your feet and legs regularly. Look for cracks, sores or changes in colour. Moisturise after bathing.
- Wear comfortable well-fitting shoes and socks. Avoid socks with a tight garter or cuff. Check the inside of shoes for small stones or rough patches before you put them on.
- If you have to stand for more than a few minutes, try to vary your stance as much as possible.
- When sitting, wriggle your toes, move your feet up and down and take frequent walks.
- Avoid sitting with your legs crossed. Put your feet up on a padded stool to reduce swelling.
- Avoid extremes of temperature such as hot baths or sitting close to a heater. Keep cold feet warm with socks and slippers.
- Consult a chiropodist or podiatrist to remove a callus or hard skin.
- Wear at least Grade 2 support stockings if your doctor has advised these. This is particularly important for the post-thrombotic syndrome, leg swelling or discomfort, and for long-distance flights.
- Have a vascular ultrasound assessment and consult a vascular surgeon to determine whether any vein treatment should be carried out.
- Horse chestnut extract appears to be of benefit for at least some patients with venous disease.
Recommended Reading: Foods That Cure Ulcerative Colitis
What Is Venous Ulcer
The identifying feature of a venous ulcer is its irregular appearance. The wound is granular in appearance and itchy, unlike arterial ulcers. This is caused when the blood from the leg is not returned to the heart and remains stagnant in the affected area.
The underlying cause thus does not always oxygenated blood to reach this area and hence cause tissue to almost undergoes oxygen starvation and hence crack up and bleed continuously. Usually, the site of occurrence of venous ulcers is the medial side of the leg and aspects such as the gaiter of the leg.
Sometimes hair may develop from the wound. Usually, they are also painless however show periodicity of pain. Usually, the pain is during the nighttime only. The affected area, however, remains warm, unlike arterial ulcers that occur cold to touch or perceive.
The risk factors of venous ulcers are pregnancy, diabetes, obesity, thrombosis, malnutrition, vein surgeries, varicose vein, and any such reason causing the blood to be stagnant in the area. Dilation of veins occurs at the leg, which is a common symptom of venous ulcers.
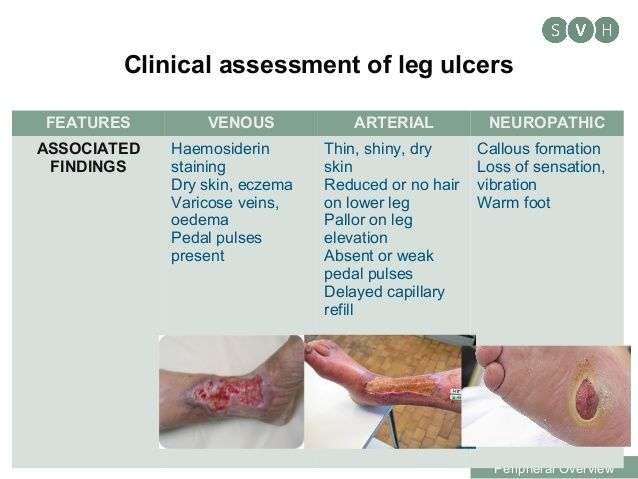
The Importance Of Vascular Assessment
Performing a thorough systematic assessment of the patient is vital for correctly diagnosing underlying causes and optimal treatment in these patients. Differentiating venous from arterial wounds should be performed by including an evaluation of anatomical location, wound shape, and wound color as a baseline, followed by vascular studies as indicated. Inappropriate treatment can lead to wound deterioration and possible limb loss or death. Utilizing various strategies and newer modalities in patients with lower extremity wounds can lead to not only better healing outcomes, but also better quality of life and lower financial burden on the patient.2
How much do you know about lower extremity wounds? Take our 10-question quiz to find out!
Accurate vascular assessment is necessary to determine correct diagnosis and treatment. Providers should examine and document both legs, including palpating pulses, edema if present , skin pigmentation changes, varicose veins, eczema, atrophie blanche, and lipodermatosclerosis. Determine sensation, activity level, and range of motion. A thorough wound assessment should include evaluation of wound site, size, depth, tissue type, exudate, edges or margins, periwound, and surrounding skin.
Don’t Miss: What Not To Eat With Bleeding Ulcers
How To Differentiate Between Arterial Venous And Diabetic Ulcers
Discerning the cause of a patients foot or lower leg ulcer can be difficult. However, there are ways to differentiate between arterial, venous, and diabetic ulcers. This is great news since ordering arterial and venous insufficiency studies for every wound is expensive and a waste of resources.
Sometimes the cause of an ulcer is a combination of arterial disease, venous disease, and diabetes. However, ulcers often have one primary cause, and there are ways to tell these types of ulcers apart.
There are three steps to follow when you begin to evaluate a patient with a foot or lower leg ulcer:
Venous Ulcers Up Close
Unlike the arterial side, which has an inherently higher pressure to push the blood out to the body, the venous side has a much lower pressure to ensure proper return of the blood back to the heart. A number of mechanisms have to be involved and properly functioning. I often refer to them as the 3 Ps: pumps, pressure, and plumbing.
Since the venous side does not have the benefit of the heart to move the blood as effectively as it does for the arterial side, the veins rely on muscles to pump the blood uphill against gravity. Every time the calf muscles contract with walking, they squeeze the veins creating pressures upwards of 300 mmHg. If we remember back to physics class, we know a liquid will move from high to low pressure, hence the blood is forced away from the contracting muscle. However, that is not enough. The veins have one-way valves that direct the blood in one direction towards the heart.
When this system of the 3 Ps begins to fail, the blood will begin to pool in the lower extremities and stagnate in the venous system. The intravenous pressure increases and then fluid begins to leak out into the interstitial space resulting in edema. Left unchecked, this will lead to a multitude of changes in the tissue including potential ulcerations.
Unlike arterial ulcers, venous ulcers are not spontaneous, as about 75% are triggered as a result of trauma, burns, cellulitis, and insect bites to name a few and the other 25% are being studied to what triggers them.
Don’t Miss: Venous Stasis Ulcer Right Lower Leg Icd 10
Arterial Ulcers Vs Venous Ulcers For Pvd
Arterial vs. venous ulcers nursing review that covers the differences between these two types of lesions that can occur when a patient has peripheral vascular disease.
As a nursing student or nurse, you must be familiar with these types of ulcers. What should you know for exams? Its important to know the location variations between arterial and venous ulcers along with their defining characteristics.
How To Tell If A Patient With Diabetes Also Has Arterial Cli
A patient with diabetes can have diabetic ulcers in conjunction with arterial CLI. Thus, if the patients pulses are weak and the wound has arterial CLI characteristics, it warrants a quick ABI test.
If the pulses are bounding, the arterial ultrasound will likely reveal arterial wall calcification rather than atherosclerosis. Arterial wall calcification will show up as black acoustic shadowing on ultrasound. Depending on which wall the plaque is on, the shadowing can happen over the whole artery , or under the artery alone .
Figure 5. Arterial wall calcification can be identified on ultrasound by the appearance of black acoustic shadowing either over the whole artery or under the artery alone.
Don’t Miss: How To Heal Venous Stasis Ulcers
What Is Arterial Ulcer
The identifying feature of an arterial ulcer is its punched-out appearance. The wound of an arterial ulcer has well-defined edges and is pale in colour, and has necrotic tissue around it. This wound is chronic and takes days to heal. The long time it takes to heal is because of the lack of blood supply to this area.
Ulcers are caused due to underlying regions like lack of oxygenated blood to the tissue causing it to break and cause the wound. This wound is also known to bleed heavily associated with pain. Leg pain is common and is the most at night. The wound occurs in weight-bearing areas of the body like the tips of toes, heels, phalangeal head and so on.
The leg usually turns cold at this spot, the skin turns dry, and in extreme cases can also turn into infected gangrene. Sometimes exudate may come from these wounds in case there is an infection, or else there is no exudate at all.
The risk factors of an arterial ulcer include diabetes, improper footwear, atherosclerosis, inborn foot deformity, smoking, vascular disease, obesity and any such disease that may prevent blood flow to the body. The leg is the most commonplace occurrence of an ulcer as it is a peripheral part of the blood where the blood reaches the last.
Arterial Vs Venous Ulcers Understand The Difference
Ulcers can be defined as open wounds in the skin or mucous membranes. It is sometimes long-lasting. When it does not have even after 5-6 weeks it can be termed as a non-healing or slow healing wound. This mostly occurs in legs or feet.
Looking for Best Arterial Leg Ulcers specialist in Oxnard? Well, there are plenty but first, you need to know what ulcer is and the difference between arterial and venous ulcers. People mostly confuse between arterial and venous ulcers. Go through this article to know the difference between them.
Recommended Reading: What Does Ulcerative Colitis Mean