Consult The Gastroenterologist Regularly:
During your treatment, your gastroenterologist needs to see you for regular checkups and if you have any concerns or need help to manage Ulcerative Colitis flare-up, you should consult the physician. Establish a good relationship with your doctor and be honest about your symptoms and condition as how they are affecting you because this all helps the gastroenterologist to determine an appropriate treatment plan for you or makes changes in the prescribed treatment plan.
Warning Signs Of A Flare
Flares often are acute, meaning they come on suddenly. They can last from days to weeks. Between flare-ups, you may experience weeks, months, or years of remission.
Symptoms of a flare may be different depending on the severity and location of the inflammation in the colon and rectum. Nevertheless, common symptoms include:
- Abdominal pain or cramps
- Fever
Watch What You Eat And Drink
You may have heard about diets for people with ulcerative colitis. Thereâs no evidence certain foods can cause or cure it. But if youâre having a flare, what you eat and drink can make symptoms worse:
- Fried or greasy foods can cause diarrhea and gas.
- Foods like beans, cabbage, and broccoli are likely to give you gas.
- Dairy products can cause gas, diarrhea, and cramps if youâre lactose intolerant.
- Alcohol and caffeine can cause diarrhea.
When youâre having a flare:
- Smaller meals eaten more often may be easier on your system.
- Drink plenty of water. Diarrhea that comes with UC can make you dehydrated.
UC can make it hard to eat normally, so you may lose weight. Your body also may not be able to absorb the nutrients you need. A nutritionist can help come up with an eating plan that works for you. Talk to your doctor to see if they recommend you take supplements.
Don’t Miss: How Long Does An Ulcerative Colitis Flare Up Last
What To Do During An Ulcerative Colitis Flare To Minimize Symptoms
Youll inevitably experience another UC flare-up at some point, despite your best prevention efforts. When this happens, there are a few ways youll need to tweak your normal routine to minimize the severity of your symptoms and get back into remission ASAP. Even some of your typically healthy habits like loading up on veggies may be a no-go. Here are a few natural remedies that may help:
Ways To Naturally Treat Ulcerative Colitis
Is yoga the key to soothing ulcerative colitis? Will an herb provide relief? Natural remedies for ulcerative colitis may not be your primary treatment approach, but they can help you manage symptoms and reduce the frequency of flares.
To date, there is no cure for UC, a chronic disease of the large intestine in which inflammation brought on by a faulty immune response creates sores or ulcers in the lining of the colon.
The chronic condition affects nearly 1 million Americans and tends to run in families. Epidemiological research shows that Westernized populations and people with diets high in fat are at higher risk for UC, as well as Caucasians and Ashkenazi Jews. But no one has yet uncovered the main cause of the disease.
Although the official cause of ulcerative colitis has evaded the medical community, its important to understand that it results from an interaction of genetic, environmental, and lifestyle factors, says Benjamin Snider, ND, a naturopathic doctor in private practice in Kitchener, Ontario.
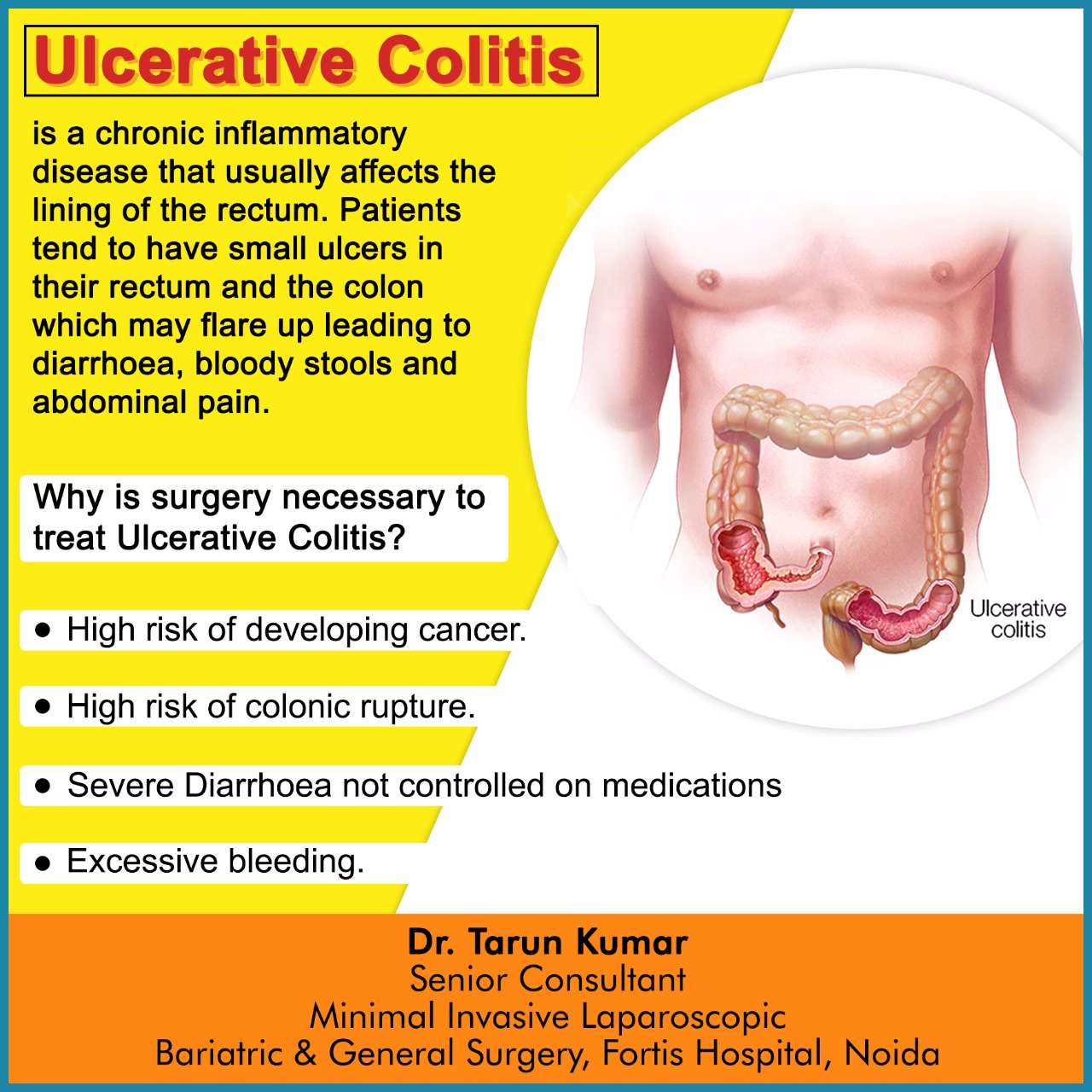
Treatments for ulcerative colitis include medications such as nonsteroidal anti-inflammatory drugs, immune system suppressors, and steroids to control inflammation and other symptoms of the condition. Surgery to remove the colon and rectum is another form of treatment if medication doesnt prove effective.
- Wheatgrass juice
- Curcumin
Read on to learn about some different kinds of natural therapies.
Recommended Reading: What Foods Not To Eat If You Have An Ulcer
Prevent Bloating With A Change In Diet
The easiest way to prevent bloating is to avoid gas-causing foods as mentioned above. When changing your diet in a drastic way, please consult your doctor before doing so.
We hope that you use our tips on how to relieve ulcerative colitis, but if your abdomen feels tender, your bloating worsens or is accompanied by other symptoms, please seek immediate medical attention. If your symptoms dont go away, you will likely need medical interference. Stop by Village Emergency Centers in Katy, River Oaks, Clear Creek, or Jersey Village for the quality medical care that you deserve.
Further Reading:
When To Seek Medical Advice
You should see your GP as soon as possible if you have symptoms of ulcerative colitis and you haven’t been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms. If necessary, they can refer you to hospital for further tests.
Read more about diagnosing ulcerative colitis.
If you’ve been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact your GP or care team for advice. You may need to be admitted to hospital.
If you can’t contact your GP or care team, call NHS 24 111 service or contact your local out-of-hours service.
Recommended Reading: How Do They Check For Ulcers
Medical Treatment For Ulcerative Colitis
Anti-inflammatory drugs are often the first step in the medical treatment of Ulcerative Colitis, with the type, dose and duration all dependent on the severity of the condition. The most common anti-inflammatory medications are Asacol HD and mesalamine.
Corticosteroids, such as prednisone and hydrocortisone, work to reduce longstanding inflammation in severe cases. They are not suitable for long-term use due to side effects, such as diabetes, weight gain, osteoporosis, and many more.
And if patients dont respond to these medications, immunosuppressants are typically the next option. They work to suppress the bodys immune response and the most common immunosuppressants are Humira and Remicade.
Antibiotics, pain relievers, iron supplements, and anti-diarrheal medications may also be recommended to help manage the symptoms of Ulcerative Colitis. In up to one-third of people with UC, surgery is performed and the most common procedure is an ileostomy.
If we consider the fact that most people with UC are diagnosed between the ages of 15 and 30 years old, this means relying on prescription drugs for nearly a lifetime
How do these medications affect our long-term health?Do they address the emotional symptoms?Do medications address the root cause of autoimmunity?
Among all the questions, heres what we DO know healing the gut is a powerful thing and it cant be overlooked when it comes to UC .
What Can I Expect If I Have A Diagnosis Of Ulcerative Colitis
Ulcerative colitis is a lifelong condition that can have mild to severe symptoms. For most people, the symptoms come and go. Some people have just one episode and recover. A few others develop a nonstop form that rapidly advances. In up to 30% of people, the disease spreads from the rectum to the colon. When both the rectum and colon are affected, ulcerative symptoms can be worse and happen more often.
You may be able to manage the disease with medications. But surgery to remove your colon and rectum is the only cure. About 30% of people with ulcerative colitis need surgery.
Read Also: What Not To Eat With Bleeding Ulcers
Limit Intake Of Animal Products
Especially meats/red meats. I have read in many articles that because many people have low stomach acidity and poor digestion, meats tend to rot in our guts, thus producing pus and contributing to inflammation . This rotting can produce more intestinal gas and overall slower digestion. I personally try to limit my meat intake to 1-2 meals per week !
How Does Pediatric Ulcerative Colitis Affect My Childs Mental/emotional Health
Like many conditions, ulcerative colitis can have a negative psychological effect, especially on children. They can experience physical, emotional, social and family problems. Because of the medications and/or general stress from the situation, your child may experience:
- Mood swings.
- Worry about appearance and physical stamina.
- Vulnerability because their body doesnt function normally.
- Poor concentration.
- Misunderstandings with friends and family.
Children need mutual support from all family members. Its helpful for the entire family to learn about the disease and try to be empathetic. Seek out a psychiatrist and therapist to help your child manage such challenges of their ulcerative colitis.
Also Check: Support Surfaces For Pressure Ulcer Prevention
Cut Out Raw Veggies And Other Gut Irritants
In the midst of a ulcerative colitis flare, you want to be as gentle on your digestive system and colon as possible. Give your gut a little vacation, says Cohen. This ideally means eliminating or scaling back on: raw vegetables, raw and cooked fruits, high-fat foods , high fiber foods , spicy foods, alcohol, and caffeinated beverages. Basically, any food that takes significant digestive effort or stimulates the bowels.
Be Consistent With Treatment Drugs
Take your medications consistently. Dont miss or skip a dose even when in remission. Dont try to wean yourself off of a treatment drug as these changes can all lead to flares.
Contact Digestive Health Services at if you have any changes to your flares, or if you think you might have ulcerative colitis.
Tags:
Recommended Reading: What Are The First Signs Of A Stomach Ulcer
Triggers For Ulcerative Colitis
Environmental factors are a BIG reason IBD is on the rise, as they can turn on the genes for Ulcerative Colitis in genetically susceptible individuals.
The most common environmental triggers of Ulcerative Colitis are:
Vitamin D Deficiency Most popular for its role in bone health, vitamin D is rapidly gaining recognition for its role in chronic disease. This study of 504 IBD patients found that lower vitamin D levels were associated with a modest increase in disease activity. Improvement in the severity of intestinal inflammation was noted within 2 weeks of supplementing with Vitamin D.
Nonsteroidal Anti-Inflammatory Drugs This study shows how NSAIDs affect the gut flora, which we now know to be extremely important when it comes to our general health. Another study demonstrated high doses, prolonged duration, and frequent use of NSAIDs were associated with an increased risk of UC.
Antibiotics Antibiotics alter the gut microbiome and can interfere with the bodys ability to handle diverse bacteria. One study shows antibiotic use within the first year of life was more common among pediatric IBD cases. A similar analysis among adult IBD subjects revealed that individuals receiving 3 rounds of antibiotics 2 or more years prior to diagnosis had greater odds of suffering with IBD.
For more information on stool testing, please read this post on why you should get stool testing done.
Medications For Other Conditions
A medication you take for another condition can also trigger a flare-up.
This might happen if you take an antibiotic to treat a bacterial infection. Antibiotics can sometimes disrupt the balance of intestinal bacteria in the gut and cause diarrhea.
Certain over-the-counter nonsteroidal anti-inflammatory drugs , such as aspirin and ibuprofen , may also irritate the colon and cause a flare-up.
This doesnt mean you should stop taking antibiotics or pain medications, but you should speak with your doctor before taking these drugs.
If you take an antibiotic, you may also need a temporary antidiarrheal medication to combat possible side effects.
If you experience stomach pain after taking an NSAID, your doctor may suggest acetaminophen to reduce pain instead.
Also Check: How To Check A Horse For Ulcers
How Long Do Flares Last
Flares occur at different times and may last for days or weeks. They can happen anywhere from weeks to years apart, depending on the person and the effectiveness of treatment.
Your doctor will work with you to treat your flare and help return your UC to a more manageable state.
The Crohns & Colitis Foundation recommends waiting to become pregnant until UC has been in remission for at least 3 months.
If you conceive during a flare-up, you may have more symptoms during pregnancy.
Youre likely to have a healthy pregnancy if you have UC, but youll still have a higher chance of complications than someone without the condition. Particularly if your UC is active, you may have a greater risk for:
- miscarriage
In general, UC medications can be taken during pregnancy.
Talk with your doctor about any possible changes to your medications while pregnant.
Ideally, having a conversation with your doctor prior to getting pregnant can allow them to prepare a UC treatment plan in advance that can be revised, if and as needed, during your pregnancy.
Can Probiotics Prevent Flares In Ulcerative Colitis
Its a well-known fact that probiotics promote healthy bacteria in the gut and work to strengthen the immune system. These popular gut health supplements are also proving to be effective in preventing flares in UC.
Ulcerative Colitis is a disorder where aggressive luminal bacteria attack the mucosa causing inflammation. Probiotics, on the other hand, can help alter the existing bacterial environment to promote less aggressive and more anti-inflammatory bacteria.
Experts also agree that any therapy or treatment that works at the level of the mucosa should be considered, since Ulcerative Colitis is a mucosal disease.
New Research on Probiotics and Ulcerative Colitis:
Escherichia coli Nissle is a non-pathogenic strain of E. coli that rivals some of the top medications for the treatment of UC. In a number of large clinical trials, researchers compared it to the medical drug mesalamine and was found to be just as effective for both inducing and maintaining remission over a 1-year period.
VSL#3 is another potent probiotic that has shown to be effective for those with UC. It has a combination of the following strains: Bifidobacterium breve, B. longum, B. infantis, Lactobacillus acidophilus, L. plantarum, L. paracasei, L. bulgaricus, and Streptococcus thermophilus.This study of 32 UCpatients showed 77% of the patients went into remission after VSL#3 was administered for 6 weeks. *Consult a physician before using this medical food grade supplement.
Recommended Reading: Can Ulcerative Colitis Cause Cancer
What Causes Rectal Bleeding
In general, hemorrhoids and diverticular disease are the most common causes of rectal bleeding.2,5 Other common causes include:
- Angiodysplasia of the colon
- Colon inflammation from many causes
- Polyps
- Stomach ulcers
- Colorectal cancer
Bleeding in the lower digestive tract has been linked to taking non-steroidal anti-inflammatory drugs , such as Aleve, Advil, and Motrin.4 Once you have been diagnosed with IBD, NSAIDs are not recommended.6
However, research about the link between NSAIDs and IBD is ongoing and so far, inconclusive. No studies have shown that taking these medications is a cause of IBD.7
Can Surgery Affect Nutritional Status
Some patients need surgery for severe inflammation, strictures, fistulas and abscesses. In Crohn’s disease, the affected portion of the digestive tract is removed. In ulcerative colitis, the colon is often removed and the ileum may be attached to the anus.
Removal of portions of the intestine can affect nutritional status. When sections of the small or large intestine are removed, surface area for absorption of nutrients is decreased. The following diagram illustrates where nutrients are absorbed. If certain portions of the intestine are severely inflamed, or have been removed, absorption of nutrients may be affected. Malnutrition and nutrient deficiencies can result.
If you have had or are planning to have surgery to remove intestines, talk to your doctor or registered dietitian about which vitamins and minerals you need to take.
Also Check: How Do You Cure Mouth Ulcers
Are Your Ulcerative Colitis Symptoms Under Control
She emphasizes that your doctor will likely be just as focused on ensuring your treatment also leads to endoscopic remission and histologic/deep remission .
Studies show that those who are in endoscopic and deep remission do best long term, as far as lower chances of hospitalizations for flare-ups and lower chances of complications, including surgery, she says.
Still, your doctor will also recommend that when you do feel your digestion is off that you recognize it and react as quickly as possible.
Pay extra attention if you are exposed to any potential ulcerative colitis triggers. For example, some common medications may prompt flares. The two biggest culprits are antibiotics and nonsteroidal anti-inflammatory drugs , such as ibuprofen, aspirin, and naproxen. Other triggers may include stress and foods that aggravated your symptoms in the past.
Diet Progression Following Flares For Ulcerative Colitis And Crohn’s Disease
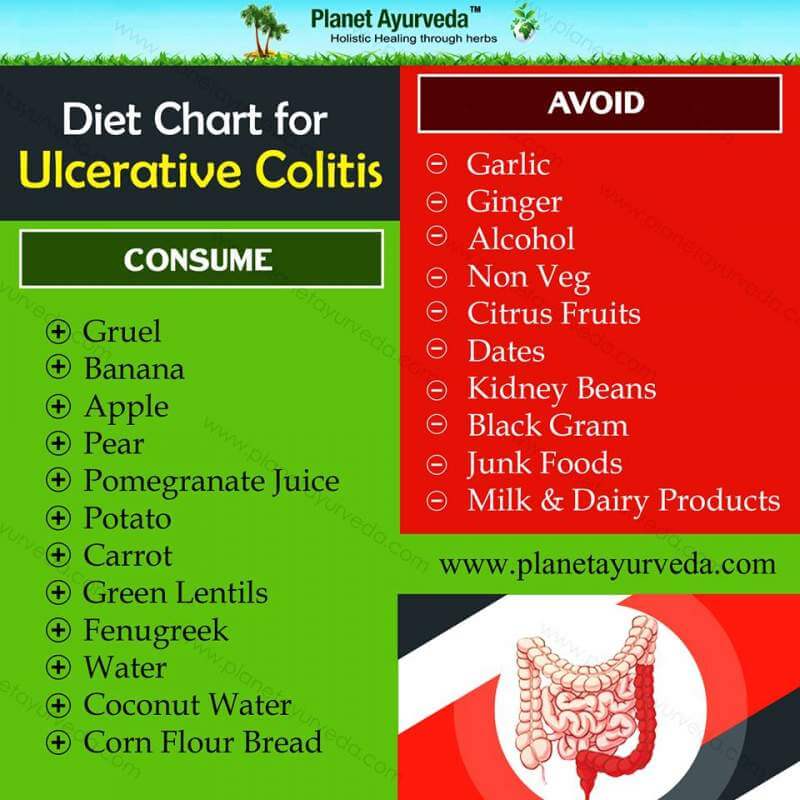
- Continue to follow a low residue diet and slowly add back a variety of foods.
- Begin with well-tolerated liquids and advance to soft solids, then solids .
- Introduce one or two items every few days and avoid any foods that cause symptoms.
- Add fiber to diet as tolerated. Well-tolerated fiber sources include tender cooked vegetables, canned or cooked fruits, and starches like cooked cereals and whole wheat noodles and tortillas.
- Between flares, eat a wide variety of foods as tolerated. This includes fruits, vegetables, whole grains, lean protein, and low-fat and nonfat dairy products.
- Increase your calorie and protein intake following a flare. Abdominal pain, diarrhea and decreased appetite may have caused poor food intake. Steroids used to treat flares also can increase protein needs.
Suggestions for first foods after a flare include:
- Diluted juices
Recommended Reading: How To Treat Skin Ulcer On Leg
Ways To Manage Symptoms And Flares Of Ulcerative Colitis
A flare of ulcerative colitis can be painful and embarrassing not only for you, but for those around you. Once you have one flare, are you going to have more? That anxiety can make you feel even worse and trigger one. Lets investigate 6 ways to manage symptoms and flares of ulcerative colitis.