Is It Important To Treat A Flare Early Or Is It Ok To Wait A Bit
Inflammation typically does not resolve without treatment and early intervention has a better outcome than waiting to treat. At an early stage of a flare, a more optimal baseline treatment is often enough to get the inflammation under control. If you wait, there is a greater risk that you might need drugs with greater side effects, such as oral steroids. By waiting, you will have to manage longer with your symptoms before getting relief. Living with constant or longer periods of inflammation might increase your risk for future complications, as inflammation might cause damage to the gut wall that accumulates in severity with each flare.
If you are experiencing worsening symptoms, you have probably already had the flare for some time without symptoms. Evidence shows that a stool test for inflammation in the colon, called fecal calprotectin, is often elevated for two to three months before any symptoms appear. Your colon might also start to show visual evidence of inflammation before you have symptoms, or at least indicate an increased risk for a flare.
What Is The Best Diet For Ulcerative Colitis
Theres no single diet that works best for ulcerative colitis. If the disease damages the lining of the colon, your body might not absorb enough nutrients from food. Your healthcare provider may recommend supplemental nutrition or vitamins. Its best to work with your provider and nutritionist to come up with a personalized diet plan.
Food As Trigger Of Flare
Participants frequently discussed the possibility that certain foods could trigger flares, but had great difficulty in identifying common themes across participants.
I never could figure out what triggers it. When Ive got a flareup going, I mean, its always, I eat, and then half an hour later Im in the bathroom.
I know until I kept a food journal, I had no concept of what would or wouldnt trigger it. I just its hard to isolate.
Don’t Miss: Tofacitinib Acute Severe Ulcerative Colitis
What Causes Ulcerative Colitis Flareups
When youre in remission from ulcerative colitis, youll want to do everything you can to prevent a flareup. Things that may cause a flareup include:
- Emotional stress: Get at least seven hours of sleep a night, exercise regularly and find healthy ways to relieve stress, such as meditation.
- NSAID use: For pain relief or a fever, use acetaminophen instead of NSAIDs like Motrin® and Advil®.
- Antibiotics: Let your healthcare provider know if antibiotics trigger your symptoms.
When To Get Medical Advice
You should see a GP as soon as possible if you have symptoms of ulcerative colitis and you have not been diagnosed with the condition.
They can arrange blood or stool sample tests to help determine what may be causing your symptoms.
If necessary, they can refer you to hospital for further tests.
If you have been diagnosed with ulcerative colitis and think you may be having a severe flare-up, contact a GP or your care team for advice.
You may need to be admitted to hospital.
If you cannot contact your GP or care team, call NHS 111 or contact your local out-of-hours service.
Don’t Miss: Best Feed For Ulcer Prone Horses
Ulcerative Colitis Adversely Affects Many Patients And Current Treatments Are Relatively Ineffective
Ulcerative colitis adversely affects the quality of life of many patients with symptoms that include frequent diarrhea, urgent bowel movements, rectal bleeding, and fatigue. Patients quality of life and economic productivity are significantly impaired by chronic ulcerative colitis . This disease often strikes individuals in their teens and twenties, and continues to wax and wane for the remainder of their lives. The severity of the symptoms, as well as the unpredictability of flares of disease, can significantly impair the lives of those affected .
Current therapies for ulcerative colitis are only modestly effective, as up to 45% of patients eventually have total surgical removal of their colon . This is a daunting and irreversible choice for young patients to make. It is particularly difficult for young females, in whom the scarring of the pelvic organs after total colectomy can result in a three-fold increase in infertility . Therefore, it is quite important to evaluate all the symptoms that patients perceive as important in assessing disease activity, to determine whether the current medical treatment is truly effective.
Can Ulcerative Colitis Go Into Remission Without Medication
“If a person with ulcerative colitis has a deep remission without any sign or symptoms for many years, it might be possible to stop treatment, but there’s little information to support this, he says. For most people, continuing to take your medication is the best way to stay in remission and avoid a flare.
Recommended Reading: Remicade Infusion For Ulcerative Colitis
Your Uc Flare Management Plan
Your doctor may help you deal with a flare by changing your medications or offering new ones. Treatment of flares can include mesalamine products and usually a steroid, such as prednisone,” says Desi.
There are also some things you can do at home to temper a flare. These include:
During an ulcerative colitis flare, its recommended that you schedule regular visits to see your doctor, at least once every three months until the symptoms go away. After the flare has subsided, physicians recommend one or two checkups a year to manage the disease.
When an ulcerative colitis flare strikes, you have options for getting your life back on track. Its important to learn what you can about maintaining your health and work with your doctor to find the best ways to safely control UC. And remember to always let your doctor know when new or persistent symptoms arise.
Symptoms Of Ulcerative Colitis
The main symptoms of ulcerative colitis are:
- recurring diarrhoea, which may contain blood, mucus or pus
- needing to empty your bowels frequently
You may also experience fatigue , loss of appetite and weight loss.
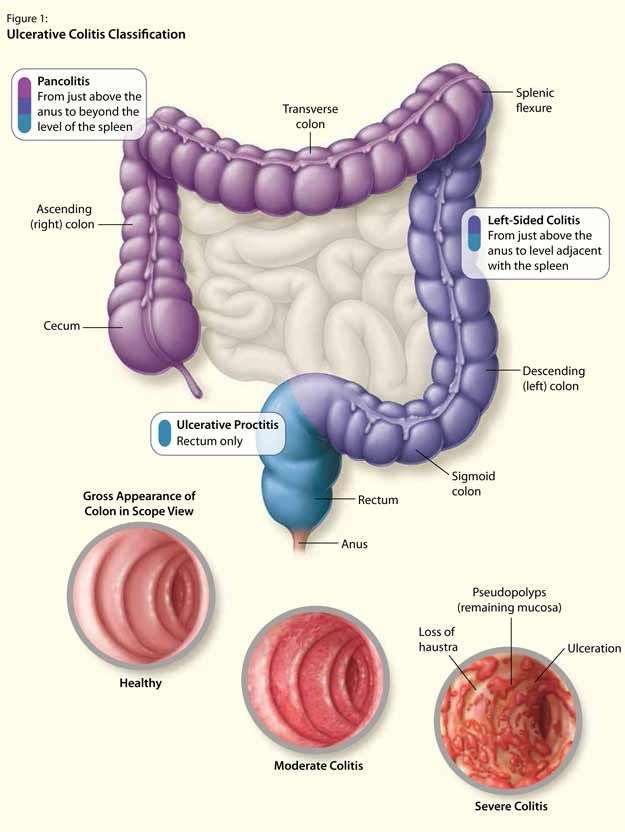
The severity of the symptoms varies, depending on how much of the rectum and colon is inflamed and how severe the inflammation is. For some people, the condition has a significant impact on their everyday lives.
Recommended Reading: How To Tell Stomach Ulcer
How Much Vitamin D Should I Take For Crohn’s
Replenishing low vitamin D helps heal active mucosal inflammation in the intestines, and oral supplementation is well-absorbed and tolerated. This was confirmed by a study published in June 2015 in the United European Gastroenterology Journal, which found a dose of 2000 international units per day to be …
Anxiety And Control Over Activities
Participants acknowledged a large amount of anxiety resulting from a pattern of their symptoms controlling their lives and the resulting effects of their disease on their quality of life.
Ive got a full-blown flareup, and uh, I try and schedule things around when Ive got to go to the bathroom in a half hour, so lets not start this meeting or lets get this meeting over, um, excuse me, Ive gotta go.
if I dont go in the morning, then its in the back of my head, Ok, whens it going to hit? But if I go in the morning, right after I get up, I have no worries the rest of the day.
You end up planning your whole life around what your gut is doing.
I mean, you plan your life around it .
When it started, I just had to stay home because so often I couldnt handle it and it had absolutely no control, and when you teach, you cannot have that in the classroom.
Also Check: What Foods Should You Eat If You Have An Ulcer
What Happens If Ulcerative Colitis Is Left Untreated
Untreated ulcerative colitis can increase the risk of colonic dysplasia and colorectal cancer. The only cure for ulcerative colitis involves the surgical removal of the colon. However, medications and diet can relieve symptoms, slow progression, and help a person stay in remission for longer.
Read also
Avoiding Certain Pain Relievers

According to the Crohns and Colitis Foundation , the following over-the-counter or prescription pain relievers can cause intestinal ulcers:
- nonsteroidal anti-inflammatories, or NSAIDs, such as ibuprofen
- COX-2 inhibitors, including the brands Celebrex and Vioxx
The CCF recommend that people avoid taking these drugs unless they are necessary to treat a serious health issue, such as heart disease.
Don’t Miss: What Is An Ulcer Diet
What Triggers An Ulcerative Colitis Flare
Triggers of ulcerative colitis flare-ups vary from person to person. It is helpful to identify factors that trigger or worsen your symptoms in order to try and avoid them. You may want to use a symptom diary or tracking app. Some of the most common include:
- **Diet. **Certain foods may trigger flares or worsen symptoms. Try to identify any foods that impact your ulcerative colitis.
- Medications. Pain relieving medications such as non-steroidal anti-inflammatories or antibiotics can worsen symptoms of ulcerative colitis
- Not taking medication as prescribed. Missing ulcerative colitis medications or taking an incorrect dose can lead to a flare-up.
- Stress. In some people, stress may impact ulcerative colitis symptoms.
How To Reduce Flare
While flare-ups often dont have a single, identifiable cause, several factors may contribute to them or make them worse, including:
- Missing your UC medications or taking the wrong dose
- Taking non-steroidal anti-inflammatory drugs or antibiotics
- Smoking
- Stress
- Certain foods
If flares occur even when a patient takes their medications as prescribed, it may be a sign that a change in medication type, dosage or frequency is needed.
Read Also: Psc Liver Disease Ulcerative Colitis
Identifying And Avoiding Trigger Foods
According to the CFF, some people with UC experience an increase in cramping, bloating, and diarrhea after eating certain foods.
Although these trigger foods vary from person to person, some common examples include:
- fatty foods
of people with IBD have insufficient vitamin D levels.
Participants with low vitamin D also needed more medications, emergency department visits, hospital admissions, and surgeries.
The authors also found that participants accessed health services less often after receiving vitamin D supplements.
Vitamin D supplements are available for purchase online.
Probiotics
Research from 2018 suggests that an imbalance in intestinal bacteria may cause the inflammation that occurs in people with UC.
In a different analysis from 2019, researchers found that people who took probiotics and an aminosalicylate had higher remission rates than those who only took an aminosalicylate.
Probiotics may help reduce UC symptoms by:
- preventing the growth of harmful gut bacteria
- regulating the immune system
- reducing inflammation in the colon
- improving the function of the intestinal barrier, which prevents toxins and harmful bacteria from entering the bloodstream
Probiotics are available for purchase online.
Curcumin
Some plants in the ginger family produce curcumin, a chemical.
In 2012, researchers investigated whether curcumin could help maintain UC remission.
Curcumin supplements are available for purchase online.
How Long Do Flares Last
Flares occur at different times and may last for days or weeks. They can happen anywhere from weeks to years apart, depending on the person and the effectiveness of treatment.
Your doctor will work with you to treat your flare and help return your UC to a more manageable state.
The Crohns & Colitis Foundation recommends waiting to become pregnant until UC has been in remission for at least 3 months.
If you conceive during a flare-up, you may have more symptoms during pregnancy.
Youre likely to have a healthy pregnancy if you have UC, but youll still have a higher chance of complications than someone without the condition. Particularly if your UC is active, you may have a greater risk for:
- miscarriage
In general, UC medications can be taken during pregnancy.
Talk with your doctor about any possible changes to your medications while pregnant.
Ideally, having a conversation with your doctor prior to getting pregnant can allow them to prepare a UC treatment plan in advance that can be revised, if and as needed, during your pregnancy.
Also Check: What Is The Best Treatment For Ulcerative Proctitis
Diet Tips During A Flare
A modified diet may help you manage and reduce your UC symptoms. Depending on the person, specific foods may trigger flare-ups or worsen symptoms. As a result, its important to identify and limit these foods.
Your doctor and a dietitian can work with you to find a diet that best manages your symptoms while providing the nutrition you need.
Analysis Of Focus Group Data
Each focus group meeting was audiotaped and fully transcribed. Each transcript was entered into NVivo version 2.0. Two members of the study team independently reviewed each transcript with a holistic view of symptoms and themes from each of the five focus group meetings and generated a list of symptom domains and common themes discussed by participants of each focus group . These lists were compared for agreement and consensus was reached . This list served as a template for a coding scheme used to analyze each transcript. The transcripts were independently coded by symptom domain and theme by J.C.J. and A.K.W. and codes were compared for agreement.
You May Like: How To Check A Horse For Ulcers
Manage Symptoms Of Ulcerative Colitis Flare
How to deal with colitis flare-up can be approached different ways. Some people have reported that herbal remedies help manage their symptoms. Probiotics, the spice turmeric, and the herb boswellia have been used to control ulcerative colitis. Studies have also shown that gingko biloba has been effective in treating colitis in rodents.
Since stress has been linked to the disease, exercises like yoga and meditation are often recommended to patients. At the same time, certain foods have a higher chance of aggravating those who suffer from ulcerative colitis, so obviously avoiding such food items is a good idea. Some examples of foods to stay away from are, whole-grain bread, whole-grain pasta, beans, raw vegetables, and dried fruit. Keeping a diary of what you eat can often help you pinpoint what causes a flare-up.
A diary or journal can also help when you are taking medications. For example, if you experience a flare-up while taking an over-the-counter medication, discuss an alternative with your doctor and/or pharmacist.
When it comes to controlling ulcerative colitis flare-up, it can take time. Some people will have multiple triggers and wont be able to make all the necessary lifestyle adjustments all at once. Sometimes, just a few changes can make a huge difference though. The following simple steps have proved to help many people tame their flare-ups:
Understanding Ulcerative Colitis Flare

A flare-up is the reappearance of disease symptoms. And for people living with ulcerative colitis , an inflammatory bowel disease , flare-ups can be unpredictable, lasting hours, days, or weeks.
- Frequent and/or urgent bowel movements
- Diarrhea
- Lack of appetite
- Joint and body aches
Because these symptoms may also be caused by something other than UC, it can sometimes be difficult to tell whether you’re experiencing a flare-up. Below, we look at factors that might affect a UC flare-up, and what can help if you are experiencing a UC flare-up.
Don’t Miss: How To Cure Ulcerative Proctitis
Can I Get Surgery For My Ulcerative Colitis
Surgery is an option if medications arent working or you have complications, such as bleeding or abnormal growths. You might develop precancerous lesions, or growths that can turn into colorectal cancer. A doctor can remove these lesions with surgery or during a colonoscopy.
Research shows that about 30% of people with ulcerative colitis need surgery sometime during their life. About 20% of children with ulcerative colitis will need surgery during their childhood years.
There are two kinds of surgery for ulcerative colitis:
Proctocolectomy and ileoanal pouch
The proctocolectomy and ileoanal pouch is the most common procedure for ulcerative colitis. This procedure typically requires more than one surgery, and there are several ways to do it. First, your surgeon does a proctocolectomy a procedure that removes your colon and rectum. Then the surgeon forms an ileoanal pouch to create a new rectum. While your body and newly made pouch is healing, your surgeon may perform a temporary ileostomy at the same time. This creates an opening in your lower belly. Your small intestines attach to the stoma, which looks like a small piece of pink skin on your belly.
After you heal, waste from your small intestines comes out through the stoma and into an attached bag called an ostomy bag. The small bag lies flat on the outside of your body, below your beltline. Youll need to wear the bag at all times to collect waste. Youll have to change the bag frequently throughout the day.
What Meals Are Protected For Folks With Ulcerative Colitis
Foods which can be normally tolerated properly by folks with UC embody:
- Breads, noodles and pastas produced from refined white flour
- Boiled white rice
- Crackers and cereals produced from white flour
- Cooked fruits
- Fruits with out peels and seeds
- Cooked greens with out skins and seeds
- Pureed greens and vegetable soups
- Soft, tender meats with out pores and skin
- Fish
You May Like: Causes Of Bleeding Ulcers In Stomach
When To Get Treatment
An increase in inflammation causes a flare, and the nature of inflammation means that you should treat it as quickly as you can. Inflammation grows exponentially, because inflammation itself causes an increase in inflammation. The longer you leave it untreated, the worse it will get. In addition, untreated inflammation not only leads to the symptoms associated with ulcerative colitis, it can also increase your risk of developing complications such as colorectal cancer down the line. Pay attention to your symptoms, and visit your physician if you notice that they change or increase even a small amount.
Correlation Between Disease Activity And Endoscopic Findings
There was a consensus that endoscopic findings would usually affirm patients own assessment of their level of disease activity.
Testing has always been pretty much a confirmation of how Im feeling at the time.
The colonoscopy reports and photos are basically, well, heres what this looks like and this looks like and heres the issue. So, theyre pretty in synch.
Read Also: Foods To Avoid With Peptic Ulcer