Is Ulcerative Colitis An Autoimmune Disease
Experts consider ulcerative colitis to be an autoimmune disease. An overactive immune response causes the immune system to attack healthy tissue in the gut, leading to inflammation of the large intestine.
Some medications people with ulcerative colitis take also compromise the immune system. However, this does not necessarily mean a person with ulcerative colitis has a higher risk of infection, including with the virus that causes COVID-19.
In this article, we look at the link between the immune system and ulcerative colitis, whether ulcerative colitis increases the risk of infection, and how treatments work to manage ulcerative colitis.
According to the Benaroya Research Institute, UC is an autoimmune disease.
An autoimmune disease happens when a persons immune system becomes overactive and attacks their healthy tissue.
In UC, the immune system attacks the intestines, causing inflammation in the large intestine.
What Triggers A Uc Flare
One of the most frustrating things about UC is how unpredictable it can be. But getting to know your disease and pinpointing specific triggers can help you take control of your life and reduce flares. While everyone is different, here are some things that may worsen UC symptoms:
-
Not taking your UC medication as directed
-
Taking nonsteroidal anti-inflammatory drugs , like aspirin, ibuprofen, and naproxen, which can irritate your digestive tract
-
Stress, which triggers the release of cortisol and adrenaline, which can in turn jack up inflammation
-
Smoking, another huge driver of inflammation in the body
-
Eating certain foods
-
Taking antibiotics, which can rid your gut of important healthy bacteria
Right Or Middle Abdomen Pain
This pain may feel like cramps in the middle of the abdomen or the RLQ. It is most common with the types of CD known as ileocolitis and ileitis. Together, these subtypes account for 75% of all CD that is diagnosed.
With ileocolitis, which is the cause in 50% of CD cases, the inflammation is found in the ileum, the last section of the small intestine. It also affects part of the colon, or large intestine.
Ileitis, which is diagnosed in 25% of cases, affects only the ileum. People with ileitis sometimes find that their pain or discomfort will arrive within a few hours of eating a meal.
You May Like: Compression Stockings For Leg Ulcers
Colon Cancer And Ulcerative Colitis
When you have ulcerative colitis, you may be more likely to get colon cancer. Your chances go up if you don’t get treatment for UC. That’s because unchecked inflammation can cause changes in the cells in your colon. These cells may turn into cancer down the road.
Your chances of getting colon cancer go up if you’ve had ulcerative colitis for 8 years or longer. The odds are also higher if:
- Your inflammation doesn’t go away.
- You’re a man.
- You have a liver condition called primary sclerosing cholangitis.
- You have a family member who’s had colon cancer.
Some research shows that people with UC may be less likely to get colon cancer now than in the past. Experts think it’s because doctors now have better ways to screen for colon cancer and they do it more often. It also helps that new medicines, like biologics, do a good job of curbing inflammation.
Who Develops Ulcerative Colitis
About 2 in 1,000 people in the UK develop ulcerative colitis. It can develop at any age but most commonly first develops between the ages of 10 and 40. About 1 in 7 cases first develop in people over the age of 60 years. Non-smokers are more likely than smokers to develop ulcerative colitis. However, smoking brings other dangers to health which far outweigh this benefit.
Don’t Miss: Why Do I Have Ulcerative Colitis
What Are The Treatments Complications And Risk Of Cancer For Diverticular Disease Vs Ulcerative Colitis
Diverticular Disease Treatment
A high-fiber diet is the mainstay of diverticulosis and diverticulitis prevention.
- Start a high-fiber diet because it will decrease the risk of complications and the accompanying symptoms however, will not make the diverticula a person has gone away. Foods high in fiber include:
- Whole-grain cereals and bread
- Vegetables
- Beans, peas, and lentils.
In the past patients with diverticulosis/diverticulitis were told that foods to avoid included seeds, corn, and nuts because it was thought fragments of these foods would get stuck in the diverticula and cause inflammation. However, current research has not found this to be the case, and the fiber content of such foods may benefit individuals with diverticulosis/diverticulitis. Discuss your diet or potential diet changes with your doctor.
Treatment for diverticulitis depends on the severity of the condition.
Treatment consists of IV or oral antibiotics, bowel rest, and possibly surgery.
If diverticulitis attacks are frequent or severe, the doctor may suggest surgery to remove a part of the patients colon.
- As with any surgery, there are risks the patient should discuss with his or her doctor.
- Sometimes the operation requires at least two separate surgeries on different occasions.
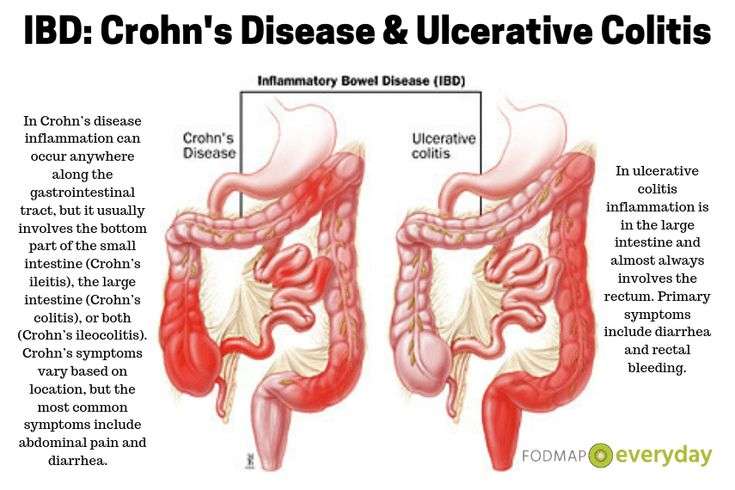
What Is Ulcerative Colitis
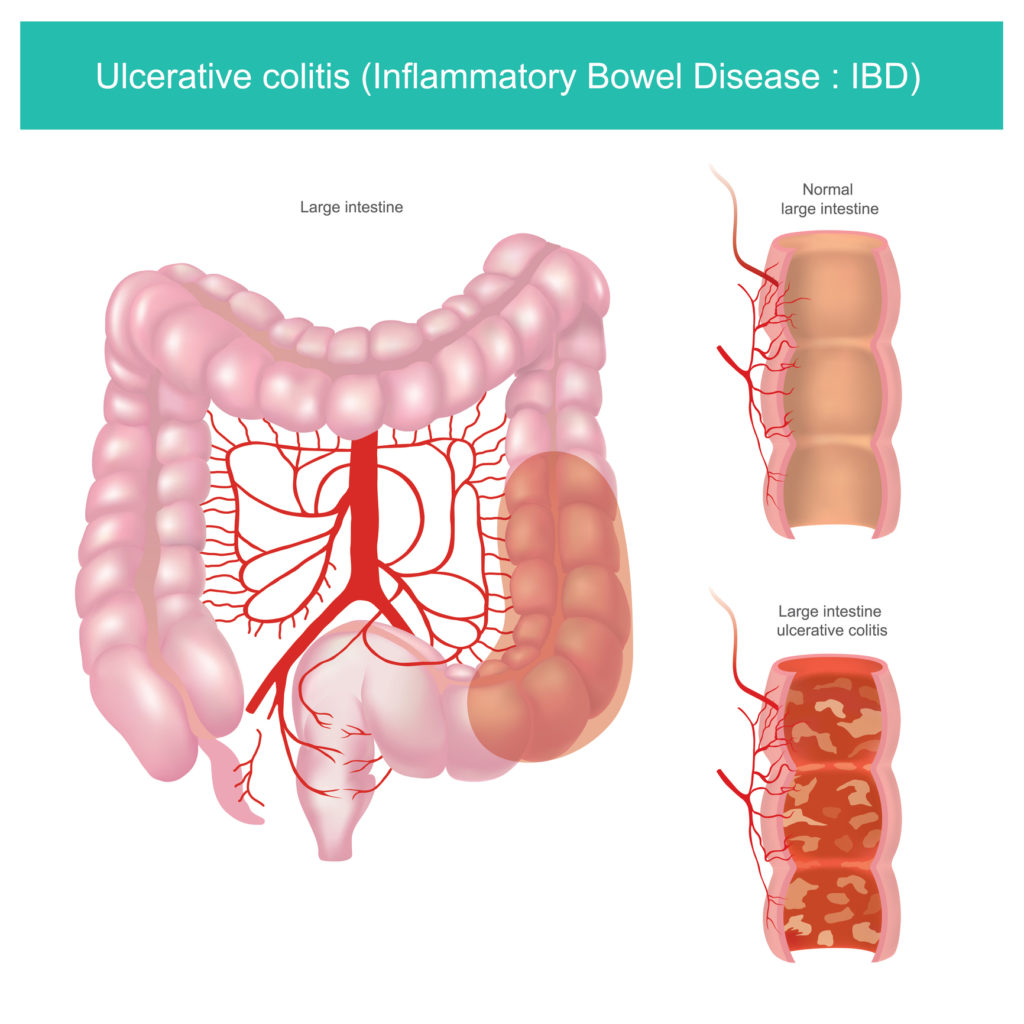
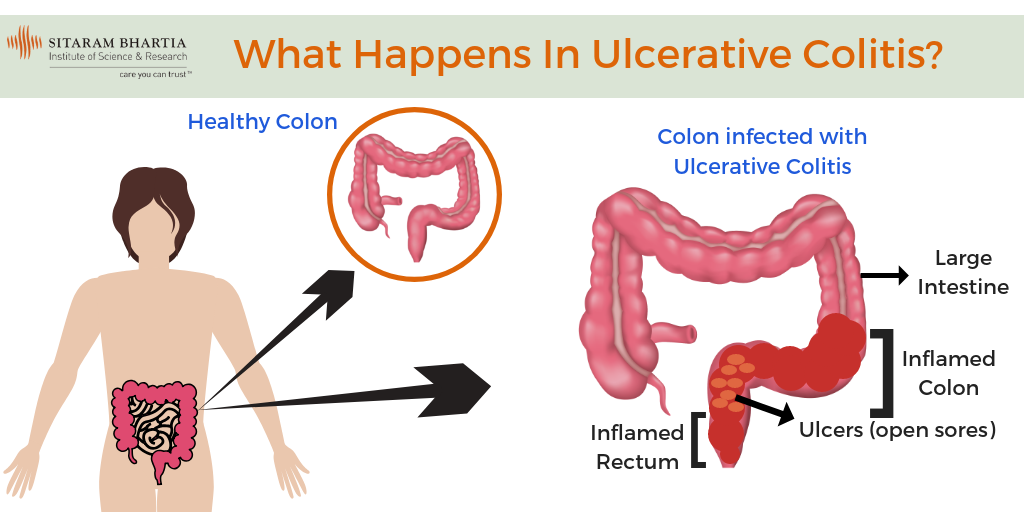
Ulcerative colitis causes irritation and ulcers in the large intestine . It belongs to a group of conditions called inflammatory bowel disease . It often causes diarrhea with blood, cramping and urgency. Sometimes these symptoms can wake a person up at night to go to the bathroom as well.
The severity of UC depends on the amount of inflammation and the location. Everyone is a little different. You could have severe inflammation in the rectum or very mild inflammation in the entire colon .
If you have ulcerative colitis, you may notice a pattern of flare-ups , when symptoms are worse. During times of remission, you might have little to no symptoms. The goal with therapy is to remain in remission as long as possible .
Recommended Reading: What Is Best Medicine For Ulcer
Don’t Miss: What To Eat To Heal An Ulcer
Smoking Increases The Risk Of Both Ulcerative Colitis And Crohns Disease But Nicotine Has Different Effects On Colonic Versus Small Bowel Inflammation
There are two commonly accepted beliefs about the relationship between smoking and Crohnâs disease and ulcerative colitis: smoking increases the risk of Crohnâs disease but protects an individual from developing ulcerative colitis, and smoking increases the severity of Crohnâs disease, but decreases the severity of ulcerative colitis. If ulcerative colitis and Crohnâs disease are both caused by MAP, how can these apparently dichotomous effects be explained? An excellent review article by Lakatos and colleagues helps elucidate the reasons for the different effects of smoking on these diseases.
First, in children, smoking increases the risk of developing both ulcerative colitis and Crohnâs disease. In a study of inflammatory bowel disease in Kentucky children , children who started smoking before 10 years of age were 7 times more likely to develop ulcerative colitis than nonsmokers, and over 3 times more likely to develop Crohnâs disease than nonsmokers. If they started smoking before age 15, they were over three times more likely to develop both diseases. Smoking increased the risk of developing both Crohnâs disease and ulcerative colitis, and in this one study increased the risk of ulcerative colitis more than it increased the risk of Crohnâs disease .
What Are The Signs & Symptoms Of Ulcerative Colitis
The most common symptoms of ulcerative colitis are cramping belly pain and diarrhea. Other symptoms include:
- blood in the toilet, on toilet paper, or in the stool
- urgent need to poop
- low energy
- weight loss
Ulcerative coliits can cause other problems, such as rashes, eye problems, joint pain and arthritis, and liver disease. Kids with ulcerative colitis may not grow well as well as other kids their age and puberty may happen later than normal.
You May Like: Is Ulcerative Colitis Genetically Inherited
Early Symptoms Of Ulcerative Colitis
If you think that you might have ulcerative colitis, keep an eye out for the following early symptoms of this IBD:
- Frequent diarrhea
- Mild to severe cramping or other pain in the lower abdomen
- Blood, mucus, or pus in the stool, or rectal bleeding
- Constant urge to empty the bowel, even when it is empty or has been emptied recently
- Urgent bowel movements
As always, talk to your doctor about these symptoms and let them know if any symptoms develop or worsen.
Turmeric And Ginger Tea
Turmeric, a relative of ginger, has been used in Ayurvedic medicine for millennia to help treat inflammatory diseases. Curcumin, the active component of turmeric, may be a safe, effective therapy for maintaining or inducing UC remission when administered with standard treatments, according to a review published in July 2020 in Nutrients. Try this soothing concoction submitted by nascarrunner71 at AllRecipes.com: Hot or cold, this tea combines ginger, turmeric, and honey or maple syrup for a rich and flavorful tea.
Read Also: Stomach Ulcer Treatment Over The Counter
Also Check: Causes Of Bleeding Ulcers In Stomach
Avoiding Certain Pain Relievers
The authors also found that participants accessed health services less often after receiving vitamin D supplements.
Vitamin D supplements are available for purchase online.
Probiotics
Research from 2018 suggests that an imbalance in intestinal bacteria may cause the inflammation that occurs in people with UC.
In a meta-analysis from 2019, researchers found that people who took probiotics and an aminosalicylate had higher remission rates than those who only took an aminosalicylate.
Probiotics may help reduce UC symptoms by:
- preventing the growth of harmful gut bacteria
- regulating the immune system
- reducing inflammation in the colon
- improving the function of the intestinal barrier, which prevents toxins and harmful bacteria from entering the bloodstream
Probiotics are available for purchase online.
Curcumin
Some plants in the ginger family produce the chemical curcumin.
In a 2012 review , researchers investigated whether curcumin could help maintain UC remission.
Compared with the placebo group, fewer people who took curcumin experienced a relapse after 6 months. However, the results were not statistically significant, and confirming the benefits of curcumin will require more research.
Curcumin supplements are available for purchase online.
Prescription medications, as well as some lifestyle and dietary changes, can help people with UC maintain remission. A person is likely to benefit from:
- managing stress, when possible
- exercising regularly
- taking care to avoid food triggers
Care For Your Child Before And After Surgery
Before either surgery, your childs surgical team will explain the details, including:
- What will happen before, during and after your childs operation
- How long its likely to take
- How long your child may need to stay in the hospital afterward
- What kind of care your child will need at home after surgery
Some children who have pouch surgery have complications afterward. The IBD Center team provides care and support for these conditions, which include urgent need to use the bathroom, bleeding, inflammation of the pouch and problems emptying stool from the pouch. Treatment options offered through the IBD Center include dietary therapies, antibiotics, probiotics, medicines that reduce inflammation, treatments done with an endoscope and surgery.
Also Check: Bland Diet Recipes For Ulcerative Colitis
The Disability Experts Of Florida Can Help
Your ulcerative colitis or Crohns condition can make you eligible for disability benefits. If your condition is impairing you from working, the experts at DEF can help. With over 100 years of combined experience, we know how to navigate the SSAs application process and we can help you prove your disability caseweve done it for thousands of other people just like you!
Dont put off filing your application in fear of rejection. The anxiety and discomfort caused by the disease, and the pressure of having to work 40 hours a week or more in order to keep a roof over your head, can take a huge toll on your health. Let our team of experts help you get the benefits that you deserve.
You May Like: Do Tums Help Ulcerative Colitis
Inflammatory Bowel Disease And Disability Insurance: A Claimants Guide
The symptoms and uncertainty associated with inflammatory bowel disease can turn your life upside down. If youre unable to work due to your ulcerative colitis or Crohns disease, you may be eligible for long-term disability benefits. However, the process of getting benefits can feel overwhelming especially during a flare.
At Bryant Legal Group, we guide people through their complex disability insurance claims and help them get the benefits they deserve. In this article, we discuss the essentials of IBD-related disability claims.
Also Check: How To Find Out If You Have Ulcerative Colitis
Read Also: How Long Does An Ulcerative Colitis Flare Up Last
When To See A Doctor If You Have Bowel Concerns
If youre having bloody diarrhea, dont wait to get help. Talk to a health professional sooner rather than later, so you can start working on a treatment plan that will get you out of the bathroom and back to normal.
Dr. Philpott also recommends keeping track of your symptoms. It can be hard to assess your response to treatment if you dont know where you started, Dr. Philpott notes. Document your symptoms down to the number of bowel movements you have. Life can be so hard with this condition that people sometimes have a hard time communicating. If you keep track of the symptoms objectively, its easier for your doctor to see how youre doing.
You dont have to just live with uncomfortable symptoms, even if youre already taking medications, Dr. East says, as adjustments to your treatment plan may be necessary. Long-term poorly controlled inflammation increases your bowel cancer risk and decreases your quality of life. New treatments could ease you into remission faster and keep you there longer.
Donât Miss: Pediatric Ulcerative Colitis Treatment Guidelines
Treatment Of Ibd Complications
Treatment depends on the particular complication, but may include:
- complications caused by nutritional deficiencies vitamin and mineral supplements , changes to diet or a liquid diet in severe cases
- inflammation in other body areas usually ease when the bowel inflammation is controlled with medication
- fistulas small openings that often heal by themselves, with treatment to ease the inflammation. A person may need surgery to close a larger fistula. Abscesses may need antibiotics and surgical drainage
- intestinal obstruction in some cases, medical treatment to ease the inflammation will clear the obstruction. In severe cases, the person will need surgery
- toxic megacolon the person goes to hospital, and receives fluids and nutrients intravenously instead of by mouth, plus antibiotics and steroids to reduce inflammation. Sometimes, the doctor will remove the contents of the persons stomach with a slender tube . A ruptured bowel needs surgical repair or removal. In severe cases, the whole of the large bowel may need to be surgically removed.
You May Like: Ulcerative Colitis Is It Contagious
Fatigue From Ulcerative Colitis Can Be Brutal
Exhaustion from ulcerative colitis can be so severe its hard to get through day-to-day life. For Sam, fatigue was one of the first signs that something was wrong. Im usually a pretty energetic person, she says. I like running every day, things like that. And I just couldnt do it anymore.
After developing ulcerative colitis, you might have to be more careful than youre used to about how you use your energy. Some days Im just hit with a truck of fatigue, Skomski says. So I always give myself an out. If I have plans with friends or were going out of town, Ill tell the other people, I might not feel good and we might have to reschedule.
Sam has had to have similarly frank conversations about the fact that her energy can take a major dip sometimes. Ive had to teach everyone around me that it doesnt mean Im mad at them, it doesnt mean Im not happy, she says. Its just that I have a very concrete amount of energy that day.
When You’re In The Hospital
You were in the hospital because you have ulcerative colitis. This is a swelling of the inner lining of your colon and rectum . It damages the lining, causing it to bleed or ooze mucus or pus.
You probably received fluids through an intravenous tube in your vein. You may have received a blood transfusion, nutrition through a feeding tube or IV, and medicines to help stop diarrhea. You may have been given medicines to reduce swelling, prevent or fight infection, or help your immune system.
You may have undergone a colonoscopy. You also may have had surgery. If so, you may have had either an ileostomy or colon resection .
You May Like: Compression Therapy For Venous Leg Ulcers
How Ulcerative Colitis Is Treated
Treatment for ulcerative colitis aims to relieve symptoms during a flare-up and prevent symptoms from returning .
In most people, this is achieved by taking medication such as:
- aminosalicylates
- corticosteroids
- immunosuppressants
Mild to moderate flare-ups can usually be treated at home. However, more severe flare-ups need to be treated in hospital to reduce the risk of serious complications, such as the colon becoming stretched and enlarged or developing large ulcers. Both of these can increase the risk of developing a hole in the bowel.
If medications arenât effective at controlling your symptoms, or your quality of life is significantly affected by your condition, surgery to remove your colon may be an option.
Read more about:
When To Call Your Doctor
If youre having any of the above UC symptoms, especially bloody stool, endless diarrhea, or severe pain, make an appointment with your primary-care doctor. It could always be something other than UC, but its important to get it checked out.
The sooner you treat UC and work to stop the damage to your intestinal lining and overall health, the better. If your GP suspects UC, they will likely refer you to a gastroenterologist, which is a type of physician specializing in digestive health care. This doc can further evaluate your symptoms, run any necessary tests, and get you a diagnosis.
If youve already been diagnosed with UC, call your gastro if youre experiencing any increase in symptoms like bloody stools, diarrhea, and pain, along with weight loss, fatigue, and fever.
And we totally get it. Talking about UC symptoms with your doctoror anyone!can feel awkward or embarrassing . But its hugely important that youre honest about whats going on so your doctor can get you the best treatment possible.
You May Like: Artificial Sweeteners And Ulcerative Colitis